Health
COVID-19 in B.C.: Data confirms unvaccinated at most risk; over 600 new cases and over 6000 active cases; and more – The Georgia Straight


Today’s new case count remained high.
Hospitalized cases continued to increase in number, heading towards 200.
Active cases continued to climb in number in all regions except for one—Vancouver Coastal Health—where active cases have been decreasing for a few days now.
Today (August 31), B.C. provincial health officer Dr. Bonnie Henry and Health Minister Adrian Dix presented a modelling update.
Although the data didn’t provide any unexpected insights, it did reaffirm and provide further evidence of what has been previously been said—that the vast majority of new cases, hospitalizations, and deaths remain among unvaccinated people.
In looking over the geographic distribution of cases, Henry observed that there isn’t a place in the province that hasn’t been affected by COVID-19 cases, the Lower Mainland has borne the brunt of the cases, and some hotspots across the province remain.
Among the places with the highest average daily rate of cases per 100,000 population in each region (from August 20 to 26) are:
- Interior Health: Golden, Grand Forks, Creston, Nelson, and Enderby, but Henry also noted that cases in Central Okanagan has levelled off and are decreasing;
- Northern Health: Nisga’a, Nechako—Henry said there are low immunization numbers in these areas, and she added that there are continuing high rates in Peace River, Fort Nelson, and Prince George (where she said there are concerning increases);
- Fraser Health: Mission;
- Vancouver Coastal Health: Vancouver Centre North (Henry said particularly areas around the Downtown Eastside);
- Island Health: Alberni-Clayoquot.
When looking at the overall curve, Henry acknowledged that case numbers have been increasing steadily since mid-July.
But she pointed out that what isn’t increasing at the same rate as in previous waves is the number of hospitalizations. She did say that in regions where they are rising, such as Interior and Northern Health, these increased hospitalizations are affecting the ability to provide healthcare.
She said that about 50 percent of the cases over the past month have been in Interior Health, which has about 15 percent of the province’s population.
When it comes to vaccinations among cases, from July 30 to August 26, the vast majority of cases were among the unvaccinated: 70 percent of cases, 81 percent of hospitalizations, and 52 percent of deaths.
Information from today’s modelling update can be downloaded from the lefthand column.
Today, the B.C. Health Ministry is reporting 655 new COVID-19 cases (including 15 epi-linked cases).
Currently, there are 6,045 active cases—an increase of 127 cases since yesterday.
The new and active cases include:
- 242 new cases in Interior Health, with 2,495 total active cases (71 more cases than yesterday);
- 186 new cases in Fraser Health, with 1,418 total active cases (47 more cases);
- 99 new cases in Vancouver Coastal Health, with 1,026 total active cases (50 fewer cases);
- 68 new cases in Island Health, with 620 total active cases (33 more cases);
- 60 new cases in Northern Health, with 479 total active cases (26 more cases);
- no new cases of people who reside outside of Canada, with seven total active cases (same number as yesterday).
An increase of 11 patients since yesterday means 187 individuals are now in hospitals and 103 of those patients are in intensive care units (12 more than yesterday).
Sadly, two new deaths (both in Island Health) have been reported. B.C. has now recorded an overall total number of 1,816 COVID-19-related fatalities during the pandemic.
With 522 recoveries since yesterday, 157,941 people who tested positive have now recovered.
During the pandemic B.C. has reported a cumulative total of 166,068 cases.
As previously noted, Dix said that over the past week, there has been a notable increase in vaccinations (following the announcement of the B.C. Vaccine Card program).
In particular, he said that there have been increases particularly among those up to 30 years old (Dix said that vaccinations among those in this age range have increased twice the provincial average) and that the “highest uptake” among regions has been in Interior and Northern Health, which previously had low rates of vaccinations.
From August 16 to 29, people not fully vaccinated accounted for 80.2 percent of cases and 88.7 percent of hospitalizations.
Out of a total of 4,698 cases from August 23 to 29, there were:
- 3,285 unvaccinated people (69.9 percent);
- 485 partially vaccinated people (10.3 percent);
- 928 fully vaccinated people (19.8 percent).
Out of a total of 186 hospitalized cases from August 16 to 29, there were:
- 150 unvaccinated people (80.6 percent);
- 15 partially vaccinated people (8.1 percent);
- 21 fully vaccinated (11.3 percent).
For cases per 100,000 population from August 23 to 29:
- 212.1 unvaccinated people;
- 124.9 partially vaccinated people;
- 28.7 fully vaccinated people.
For cases hospitalized per 100,000 population from August 16 to 29:
- 9.6 unvaccinated people;
- 3.5 partially vaccinated;
- 0.7 fully vaccinated people.
Since December, B.C. has administered 7,463,858 doses of Pfizer, Moderna, and AstraZeneca vaccines.
As of today, 84.3 percent (3,908,860) of eligible people 12 and older in B.C. have received their first dose of COVID-19 vaccine and 76.5 percent (3,547,751) received their second dose.
In addition, 85 percent (3,676,744) of all eligible adults in B.C. have received their first dose and 77.6 percent (3,355,134) received their second dose.
Interior Health has declared a new healthcare facility outbreak at Kamloops Seniors Village.
Vancouver Coastal Health has imposed restrictions at the Arbutus Care Centre in Vancouver, but has not yet declared an outbreak.
As of today, there are 19 active outbreaks, including:
- longterm care: Heritage Village (Fraser Health); Brock Fahrni (Vancouver Coastal Health); Village at Mill Creek, Nelson Jubilee Manor, Kootenay Street Village, Cottonwoods Care Centre, Brookhaven Care Centre, Spring Valley Care Centre, and Kamloops Seniors Village (Interior Health); and Sunset Lodge (Island Health);
- acute care: Peace Arch Hospital and Chilliwack General Hospital (Fraser Health); and Fort St. John Hospital (Northern Health);
- assisted or independent living: Nicola Meadows, Hawthorn Park, David Lloyd Jones, Sun Pointe Village, Hardy View Lodge, and Rose Woods Village (Interior Health).
None of the five regional health authorities listed any new community outbreaks, business closures, or public exposure events.
Health
Canada's opioid deaths double in 2 years, men in their 20s, 30s hit hardest – Surrey Now Leader

Opioid-related deaths doubled in Canada between 2019 and the end of 2021, with Manitoba, Saskatchewan and Alberta experiencing a dramatic jump, mostly among men in their 20s and 30s, says a new study that calls for targeted harm-reduction policies.
Researchers from the University of Toronto analyzed accidental opioid-related deaths between Jan. 1, 2019 and Dec. 31, 2021 in those provinces as well as British Columbia, Ontario, Quebec, New Brunswick and Nova Scotia, and the Northwest Territories.
Manitoba saw the sharpest rise in overdose deaths for those aged 30 to 39 – reaching 500 deaths per million population, more than five times the 89 deaths per million population recorded at the beginning of the study period.
In Saskatchewan, the death toll for that age group nearly tripled to 424 per million, up from 146 per million, while Alberta’s rate spiked more than 2.5 times to 729 fatalities per million, up from 272 per million. Ontario’s death rate reached 384, up from 210 per million.
British Columbia, which has been the epicentre of the overdose crisis, recorded 229 deaths per million for that age group in 2019, climbing to 394 in 2020. All data for 2021 from that province’s coroners service was not yet available when researchers completed their work based on information collected by the Public Health Agency of Canada.
Nationally, the annual number of opioid overdose deaths surged from 3,007 to 6,222 over the three-year study period, which researchers note coincided with pandemic public health measures that reduced access to harm reduction programs and imposed border restrictions that may have increased the toxicity of the drug supply.
“In addition, for many, the pandemic exacerbated feelings of anxiety, uncertainty, and loneliness, contributing to increased substance use globally,” they said.
The study was published Monday in the Canadian Medical Association Journal.
Senior author Tara Gomes said one in four deaths involved people in their 20s and 30s. More than 70 per cent of the overall deaths were among men.
A spokesman with the coroners service in British Columbia said 78 per cent of people that fatally overdosed in that province between 2019 and the end of 2021 were men.
The sharp surge in fatal overdoses – especially among young adults in the Prairies – suggests provinces must act quickly, said Gomes, an epidemiologist who called for more harm-reduction services including supervised consumption sites.
“Being slow and not being as nimble as we would like to be in our responses can have really devastating impacts,” said Gomes, also lead principal investigator of the Ontario Drug Policy Research Network.
Bernadette Smith, Manitoba’s minister of housing, addiction, homelessness and mental health, said the province plans to open its first supervised consumption site in Winnipeg next year and will also offer drug-testing machines so people can check if their illicit substances are toxic.
“We came out of a previous government that didn’t take a harm-reduction approach, unfortunately,” said the New Democrat, whose party defeated the Progressive Conservatives last fall.
“We’re working with front-line organizations because they have not been listened to or worked with for the last seven years in our province, which has been a real problem.”
Manitoba plans to train family doctors to treat addiction with medications including Suboxone and methadone, said Smith, noting the physicians typically refer patients to detox for care.
“We’re creating a model so that folks aren’t having to go to a bunch of different places to get different services,” said Smith.
She declined to say whether Manitobans will have access to a prescribed safer supply of drugs.
Tanya Hornbuckle of Edmonton said her son Joel Wolstenholme was 30 when he died in 2022. He became addicted to illicit substances at about age 14, starting with cannabis before shifting to methamphetamine, cocaine and other drugs that were increasingly laced with fentanyl.
He also battled a mental illness but getting help for both that issue and addiction in a single service was challenging, Hornbuckle said.
Wolstenholme tried multiple times to detox but there were never enough beds at a clinic where people had to line up at 8 a.m., she said.
“It would happen over and over and then he would call me. I went and stood in line or I drove him there and waited with him in the lineup. They wouldn’t have enough beds.”
Her son’s anxieties and addiction worsened when pandemic restrictions prevented her from entering an emergency room with him because he did not trust staff, Hornbuckle said.
On Feb. 6, 2022, Hornbuckle went to her son’s home so they could cook together. She found him dead.
The Alberta government’s strategy of focusing more on recovery and abstinence-based treatment than harm reduction, mental health and housing is the wrong approach, said Hornbuckle, noting that for a time her son slept in parks and abandoned houses after losing his vehicle and apartment to addiction.
Rebecca Haines-Saah, an associate professor of community health services at the University of Calgary, called the deaths of young people from overdose a tragedy, and said many more suffer from brain injury due to toxic substances.
“Obviously, we have the incorrect response. We do not have the approach and services available to keep people alive,” said Haines-Saah, who also called for more harm-reduction services.
“We don’t have a full-scale public health response that is required. We don’t have any plans to fund anything that relates to what we would call harm reduction.”
Much of the current approach to addiction excludes a large number of recreational drug users, said Gomes. She said between a third and half of the deaths in Ontario involved people without an opioid use disorder diagnosis.
“So, focusing on (residential treatment) alone is something that really concerns me because we really need to make sure that we have different options for different people.”
READ ALSO: Stories from the overdose crisis’ front lines
READ ALSO: Make overdose education mandatory in B.C. schools amid drug emergency, advocates say
Health
Manitoba significantly impacted by opioid-related deaths at start of pandemic | CTV News – CTV News Winnipeg
A new study out of Ontario and posted in the Canadian Medical Association Journal is highlighting the significant increase in accidental opioid-related deaths in Canada leading into the COVID-19 pandemic, with Manitoba being one of the most impacted provinces in the country.
The research looked at opioid-related deaths between 2019 and 2021 in nine provinces and territories in Canada.
Across Canada, opioid-related deaths more than doubled from 2019 with 3,007, to 6,222 in 2021.
It also found the years of life lost per 100,000 people climbed from 3.5 years in 2019 to seven in 2021.
After dipping halfway through 2019, opioid-related deaths spiked dramatically through the first quarter of 2020 and spiked again in the third quarter of 2021.
People in their 20s and 30s were most impacted by opioid deaths as they represented 29.3 per cent of all deaths in people aged 20 to 29 and 29 per cent of all deaths for people between 30 and 39.
“The disproportionate loss of life in this demographic group highlights the critical need for targeted prevention efforts,” the report said.
The data also showed men were much more likely to suffer an opioid-related death compared to women, with more than 4,500 deaths in 2021 compared to more than 1,600 women.
Manitoba one of the most impacted provinces by opioid-related deaths
Breaking down the provinces individually, the research found the Prairie provinces were impacted the most by opioid-related deaths.
Alberta and Saskatchewan both recorded fatality numbers that more than doubled between 2019 and 2021 – 619 deaths to 1,618 in Alberta and 109 to 322 deaths in Saskatchewan.
Meanwhile, Manitoba’s opioid-related deaths spiked nearly five-fold by 2021. There were 54 deaths in the province in 2019 and by the end of 2021, there were 263.
“In Manitoba, 70 per cent of opioid toxicity deaths in 2019 had fentanyl or fentanyl analogues detected, increasing to 86 per cent in 2020,” the report said.
Arlene Last-Kolb, a member of Moms Stop the Harm, lost her son Jessie to fentanyl drug poisoning in 2014.
She said the toxic drug supply is one of the main issues that needs to be addressed.
“We’re losing a whole generation of young people like my son,” Last-Kolb said. “It’s going to take a lot more than safe spaces and more treatment to address the toxic drug supply, including opiates, fentanyl that we have on our streets.”
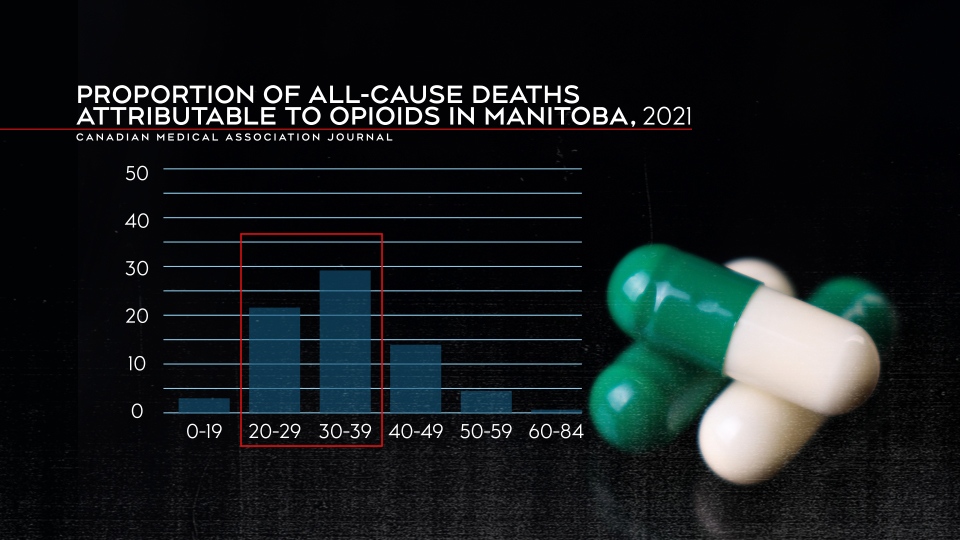
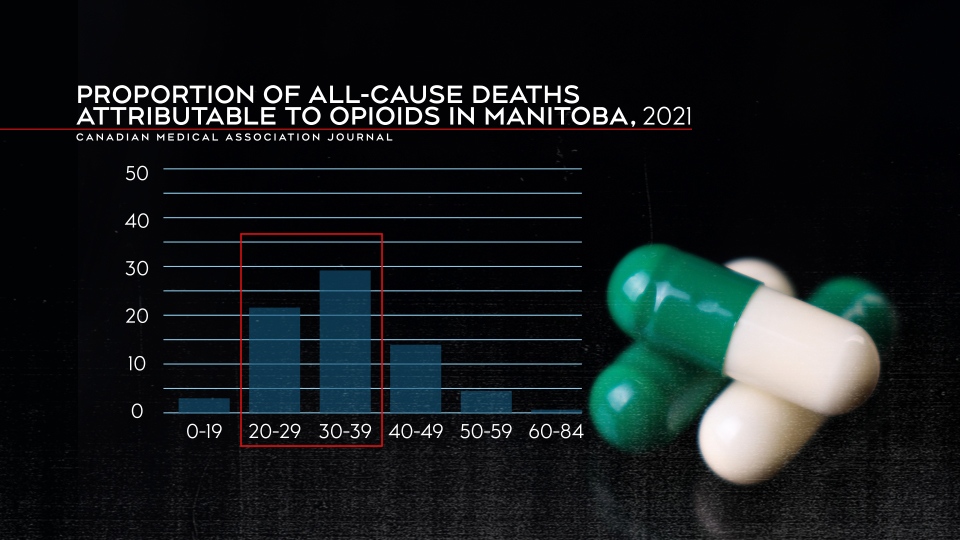
Proportion of all-cause deaths attributable to opioids in Manitoba in 2021. (Canadian Medical Association Journal)
The years of life lost also jumped dramatically in Manitoba, going from 1.8 per 100,000 to 8.5 per 100,000 in 2021.
Those in the 30 to 39 age range were most impacted by opioid-related deaths in Manitoba. Almost 30 per cent of deaths in that age group were attributable to opioids.
Marion Willis, the founder and executive director of St. Boniface Street Links, called the numbers horrifying. She says something needs to be done as soon as possible.
“If that is not the strongest statement ever to support that we need a plan to address the drug crisis in this city, in this province – I don’t know what it takes,” said Willis.
She said plans for a new safe consumption site are a good first step, but agreed the drug supply also needs to be addressed.
“Safe consumption needs to include safer supply, or will we still have people using the same toxic drugs off the street.”
Bernadette Smith, the minister of housing, addictions and homelessness, said the province has a number of items on its agenda to help deal with the problem.
“That’s exactly what our government is doing. So supervised consumption site, drug testing machines, that’s our first step – getting those up and running,” said Smith.
However, Willis and Last-Kolb want to see action now.
“This is a challenge that is impacting all members of our human family. We’re all losing our loved ones, you know, from the wealthiest families to the poorest families. This is affecting everybody,” said Willis.
“It’s frustrating to talk about things that are going to happen down the road when somebody dies here every single day,” said Last-Kolb.
Health
Dr. Theresa Tam to visit 3 Nunavut communities regarding TB outbreaks – pentictonherald.ca


Canada’s chief public health officer, Dr. Theresa Tam, will tour Nunavut this week.
The communities of Naujaat, Pond Inlet (Mittimatalik), and Iqaluit are on her itinerary, to coincide with the launch of a community-wide screening clinic for tuberculosis (TB) in Naujaat.
Naujaat and Pond Inlet are currently experiencing TB outbreaks. Tam’s visit to Nunavut will be an opportunity for Canada’s top doctor to work with Nunavut Tunngavik Incorporated (NTI) and the Government of Nunavut, to observe social issues, such as housing shortages and food insecurity, that have significant impacts on the health of Nunavut Inuit, according to NTI.
Tam will be accompanied in her travels by NTI vice-president Paul Irngaut, Government of Nunavut Minister of Health John Main, and Nunavut’s deputy chief public health officer Dr. Ekua Agyemang, among others.
TNCMS.AdManager.init
(
domain: “www.pentictonherald.ca”,
secureDomain: “pentictonherald.ca”,
virtualregion:
popup: __tnt.ads.popup
,
callback:
expandable: __tnt.ads.expandable,
html: __tnt.ads.html,
image: __tnt.ads.image,
pagecurl: __tnt.ads.curl,
text: __tnt.ads.text,
video: __tnt.ads.video
);
“Nunavut Inuit face challenges that don’t affect most Canadians when accessing healthcare,” Irngaut said. “Having Dr. Tam on the ground visiting Nunavut communities will give her the opportunity to see firsthand some of the barriers that Inuit face when trying to navigate the healthcare system in Nunavut.”
Canada’s top doctor’s tour will conclude with two days of meetings and events in Iqaluit.
Although TB remains the focus of the visit for Tam, she will also meet with community groups and organizations to discuss related territorial issues such as homelessness, health education, mental health and health research initiatives.
-
Media13 hours ago
DJT Stock Plunges After Trump Media Files to Issue Shares
-
Business12 hours ago
FFAW, ASP Pleased With Resumption of Crab Fishery – VOCM
-
Media12 hours ago
Marjorie Taylor Greene won’t say what happened to her Trump Media stock
-



 Tech20 hours ago
Tech20 hours agoHow funny? Australian researchers use AI to generate cartoon captions – Digital Journal
-
Business13 hours ago
Javier Blas 10 Things Oil Traders Need to Know About Iran's Attack on Israel – OilPrice.com
-
Media11 hours ago
Trump Media stock slides again to bring it nearly 60% below its peak as euphoria fades – National Post
-
News23 hours ago
Anyone want a camper? It's a buyer's market for RVs as pandemic-era sales fizzle – CBC.ca
-



 Sports23 hours ago
Sports23 hours agoSerdachny scores overtime winner as Canada edges U.S. for women's hockey worlds gold – CBC Sports







