Health
Details of loan program coming and Trump’s use of malaria drug; In The News for May 20

|
|
In The News is a roundup of stories from The Canadian Press designed to kickstart your day. Here is what’s on the radar of our editors for the morning of May 20 …
—
COVID-19 in Canada …
The federal government is beefing up efforts to persuade businesses to rehire workers now that Canada’s economy is starting to emerge from the COVID-19 lockdown.
It is expected today to unveil more details of its promised loan program for large corporations and commercial rent relief for small- and mid-sized businesses.
That includes more information on how businesses can apply for the programs and what conditions will apply.
Today’s focus follows last week’s extension of the 75 per cent wage subsidy for three months, to the end of August, and Tuesday’s announcement that the government is expanding the eligibility criteria for its small business loan program.
The latter program provides interest-free loans of $40,000 for eligible small businesses to cover costs like rent and utilities, with the possibility of forgiving one-quarter of the amount if it is paid off by the end of 2022.
Tuesday’s fix extended the program to companies that don’t have traditional payrolls, such as family-run businesses that pay themselves in dividends and companies that employ only contractors.
“This is about getting people back to work and giving businesses the confidence to reopen, rehire and even grow because the way our economy will recover and the way our country will remain resilient and successful is by getting Canadians back to work,” Prime Minister Justin Trudeau said Tuesday.
—
In other Canadian news …
Statistics Canada is expected to report that the consumer price index decreased in April, the first full month the economy was gripped by the COVID-19 pandemic.
Economists on average had expected a reading of negative 0.28 per cent for April, according to financial markets data firm Refinitiv.
That’s a further decline from March when the annual pace of inflation in Canada was 0.9 per cent, marking the biggest one-month decrease in more than a decade.
It was down from 2.2 per cent in February as the price of oil collapsed and the economy then ground to a halt when governments ordered the closure of non-essential businesses in mid-March to slow the spread of COVID-19.
The Consumer Price Index measures price changes for a fixed basket of goods and services that are divided into eight major components.
These are food, shelter, household operations, furnishings and equipment, clothing and footwear, transportation, health and personal care, recreation, education and alcoholic beverages, tobacco products and recreational cannabis.
—
Also this …
As provinces take their cautious first steps to allow people back into local businesses, a new poll suggests most Canadians don’t think province-wide measures are the best way to reopen the economy.
The latest poll on the COVID-19 pandemic by Leger and the Association for Canadian Studies suggests only 35 per cent of people thought restrictions should be loosened for entire provinces.
In contrast, 47 per cent thought those decisions should apply to specific regions within each province. Just 18 per cent said reopening measures should apply to all of Canada at once.
Still, just over half of those polled said they trust provinces to make the call about what businesses should reopen and when, whereas about one-third said that should be up to Ottawa and 14 per cent said local governments should decide.
That is essentially what happened in Quebec, where the provincial government delayed the planned reopening of schools, daycares and businesses in the Greater Montreal area for one week because of the particularly high COVID-19 infection rate in the area and a shortage of health-care workers.
The proportion of people who said they would like decisions to be made region by region were highest in that province at 73 per cent, followed by Alberta at 52 per cent.
—
COVID-19 in the U.S. …
President Donald Trump emphatically defended himself against criticism from medical experts that his announced use of a malaria drug against the coronavirus could spark wide misuse by Americans of the unproven treatment with potentially fatal side effects.
Trump’s revelation a day earlier that he was taking hydroxychloroquine caught many in his administration by surprise and set off an urgent effort by officials to justify his action. But their attempt to address the concerns of health professionals was undercut by the president himself.
He asserted without evidence that a study of veterans raising alarm about the drug was “false” and an “enemy statement,” even as his own government warned that the drug should be administered for COVID-19 only in a hospital or research setting.
“If you look at the one survey, the only bad survey, they were giving it to people that were in very bad shape,” Trump said. That was an apparent reference to a study of hundreds of patients treated by the Department of Veterans Affairs in which more of those in a group who were administered hydroxychloroquine died than among those who weren’t.
“They were very old. Almost dead,” Trump said. “It was a Trump enemy statement.” During a Cabinet meeting, he elicited a defense of his practice from other officials, including VA Secretary Robert Wilkie who noted that the study in question was not conducted by his agency.
But the drug has not been shown to combat the virus in a multitude of other studies as well. Two large observational studies, each involving around 1,400 patients in New York, recently found no COVID benefit from hydroxychloroquine. Two new ones published last week in the medical journal BMJ reached the same conclusion.
No large, rigorous studies have found the drug safe or effective for preventing or treating COVID-19.
—
COVID-19 around the world …
President Donald Trump’s declaration that he was taking a malaria drug of dubious effectiveness to help fend off the coronavirus will likely be welcomed in India.
Trump’s previous endorsement of hydroxychloroquine catalyzed a tremendous shift in the South Asian country, spurring the world’s largest producer of the drug to make much more of it, prescribe it for front-line health workers treating the virus and deploy it as a diplomatic tool, despite mounting evidence against using the drug for COVID-19.
Trump said Monday that he was taking hydroxychloroquine as a measure of protection against the virus. The U.S. Food and Drug Administration, however, has cautioned against using it outside of hospitals because of the risk of serious heart problems.
Suhhil Gupta, a pharmacist in New Delhi, said Tuesday that Trump’s announcement shouldn’t carry any weight in India.
“He’s not a pharmacist. His statements are not relevant to the field,” Gupta said.
Still, India’s policy on the decades-old drug, used to prevent malaria and treat lupus and rheumatoid arthritis, drastically changed after Trump tweeted in March that the drug, used together with an antibiotic, could be “game changers” in the fight against the pandemic. India’s health ministry quickly approved it as a prophylactic for health care workers and others at high risk of infection, and as a treatment for critically ill patients.
—
In non-COVID-19 entertainment news …
Alanis Morissette is among the special guests set to appear in next week’s finale of the new incarnation of “Fraggle Rock” on Apple TV Plus.
The Ottawa-born singer-songwriter will appear along with several other stars in the sixth instalment of “Fraggle Rock: Rock On!” next Tuesday.
She’ll sing the classic “Fraggle Rock” theme song, along with Common, Jason Mraz, Neil Patrick Harris, Tiffany Haddish, and Ziggy Marley.
The original 1980s version of the children’s puppet series from the Jim Henson Company was filmed in Toronto.
The new U.S.-shot series features mini episodes that have appeared every Tuesday for free on the streaming service since last month.
—
COVID-19 in sports …
Alberta’s Jason Kenney is the latest premier to make a pitch for his province to host National Hockey League games should the league resume play.
The league suspended its season in February and is now eyeing a format to complete it with an improvised playoff scenario. One possibility is a tournament of 24 teams spread over two hub cities.
Kenney says he is working with the Edmonton Oilers on a proposal to be a host city and expects to be discussing the issue later this week with NHL commissioner Gary Bettman.
He says Edmonton would be a prime location, given it has low COVID numbers and a new downtown rink with a hotel attached to provide an isolation safe zone for players.
“I think we’ve got a tremendous pitch to make,” Kenney says.
—
This report by The Canadian Press was first published May 20, 2020





Health
Quebec successfully pushes back against rise in measles cases – CBC.ca
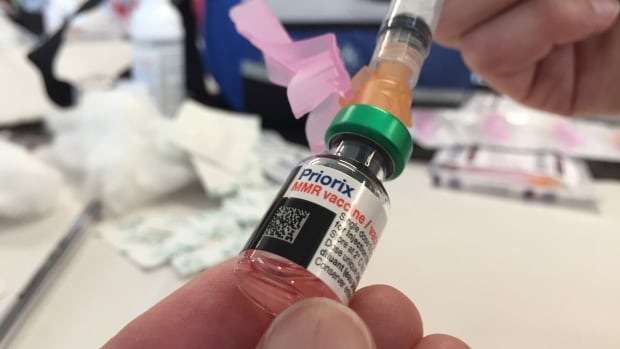
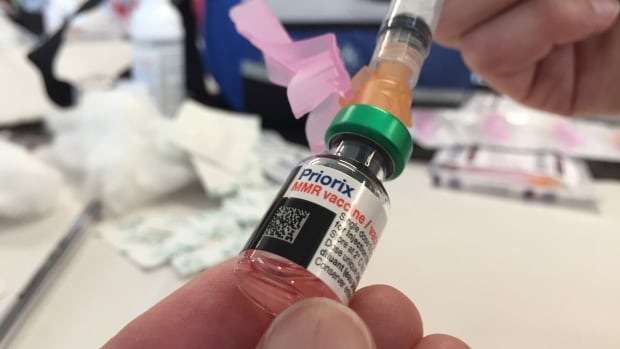
Quebec appears to be winning its battle against the rising tide of measles after 45 cases were confirmed province-wide this year.
“We’ve had no locally transmitted measles cases since March 25, so that’s good news,” said Dr. Paul Le Guerrier, responsible for immunization for Montreal Public Health.
There are 17 patients with measles in Quebec currently, and the most recent case is somebody who was infected while abroad, he said.
But it was no small task to get to this point.
Le Guerrier said once local transmission was detected, news was spread fast among health centres to ensure proper protocols were followed — such as not letting potentially infected people sit in waiting rooms for hours on end.
Then about 90 staffers were put to work, tracking down those who were in contact with positive cases and are not properly vaccinated. They were given post-exposure prophylaxis, which prevents disease, said Le Guerrier.
From there, a vaccination campaign was launched, especially in daycares, schools and neighbourhoods with low inoculation rates. There was an effort to convince parents to get their children vaccinated.
Vaccination in schools boosted
Some schools, mostly in Montreal, had vaccination rates as low as 30 or 40 per cent.
“Vaccination was well accepted and parents responded well,” said Le Guerrier. “Some schools went from very low to as high as 85 to 90 per cent vaccination coverage.”
But it’s not only children who aren’t properly vaccinated. Le Guerrier said people need two doses after age one to be fully inoculated, and he encouraged people to check their status.
There are all kinds of reasons why people aren’t vaccinated, but it’s only about five per cent who are against immunization, he said. So far, some 10,000 people have been vaccinated against measles province-wide during this campaign, Le Guerrier said.
The next step is to continue pushing for further vaccination, but he said, small outbreaks are likely in the future as measles is spreading abroad and travellers are likely to bring it back with them.
Need to improve vaccination rate, expert says
Dr. Donald Vinh, an infectious diseases specialist from the McGill University Health Centre, said it’s not time to rest on our laurels, but this is a good indication that public health is able to take action quickly and that people are willing to listen to health recommendations.
“We are not seeing new cases or at least the new cases are not exceeding the number of cases that we can handle,” said Vinh.
“So these are all reassuring signs, but I don’t think it’s a sign that we need to become complacent.”
Vinh said there are also signs that the public is lagging in vaccine coverage and it’s important to respond to this with improved education and access. Otherwise, microbes capitalize on our weaknesses, he said.
Getting vaccination coverage up to an adequate level is necessary, Vinh said, or more small outbreaks like this will continue to happen.
“And it’s very possible that we may not be able to get one under control if we don’t react quickly enough,” he said.
Health
Pregnant women in the Black Country urged to get whooping cough vaccine – BBC.com


Pregnant women urged to get whooping cough vaccine
Pregnant women in the Black Country are being urged to get vaccinated against whooping cough after a rise in cases.
The bacterial infection of the lungs spreads very easily and can cause serious problems, especially in babies and young children.
The Black Country Integrated Care Board (ICB) is advising pregnant women between 16 and 32 weeks to contact their GP to get the vaccine so their baby has protection from birth.
The UK Health Security Agency warned earlier this year of a steady decline in uptake of the vaccine in pregnant women and children.
Symptoms of the infection, also known as “100-day cough”, are similar to a cold, with a runny nose and sore throat.
Sally Roberts, chief nursing officer for the ICB, which covers Wolverhampton, Dudley, Walsall and Sandwell, said anyone could catch it, but it was more serious for young children and babies.
“Getting vaccinated while you’re pregnant is highly effective in protecting your baby from developing whooping cough in the first few weeks of their life – ideally from 16 weeks up to 32 weeks of pregnancy,” she said.
“If for any reason you miss having the vaccine, you can still have it up until you go into labour.”
Follow BBC West Midlands on Facebook, X and Instagram. Send your story ideas to: newsonline.westmidlands@bbc.co.uk
Health
Measles cases stabilize in Montreal – CityNews Montreal
The number of measles cases has stabilized, according to the Montreal Public Health.
Since March 25, there have been no contaminations reported within the community.
“Our teams have identified all contact cases of measles,” said media relations advisor Geneviève Paradis. “It’s a laborious task: each measles case produces hundreds of contacts.”
All community transmission cases since February 2024 have been caused by returning travelers who were either unvaccinated or partially vaccinated.
Currently, there are 18 measles cases in Montreal – with 46 total in Quebec. This according to the April 18 figures from the provincial government.
“With the summer vacations approaching, if you’re travelling, it is essential to check if you are protected against measles,” explained Paradis.
According to Montreal Public Health, a person needs to have received two doses after the age of 12 months to be immunized against the virus.
They’ve launched a vaccination campaign throughout the region, and currently, 11,341 people have been vaccinated against measles in Montreal between March 19 and April 15.
Vaccination is also being provided in schools and at local service points.
“The vaccination operation is under the responsibility of the five CIUSSS of the territory,” concluded Paradis.
-



 Tech22 hours ago
Tech22 hours agoCytiva Showcases Single-Use Mixing System at INTERPHEX 2024 – BioPharm International
-



 Health18 hours ago
Health18 hours agoSupervised consumption sites urgently needed, says study – Sudbury.com
-
News18 hours ago
Canada's 2024 budget announces 'halal mortgages'. Here's what to know – National Post
-



 Science5 hours ago
Science5 hours agoJeremy Hansen – The Canadian Encyclopedia
-
News17 hours ago
2024 federal budget's key takeaways: Housing and carbon rebates, students and sin taxes – CBC News
-



 Tech20 hours ago
Tech20 hours agoNew EV features for Google Maps have arrived. Here’s how to use them. – The Washington Post
-
Tech23 hours ago
Nintendo Indie World Showcase April 2024 – Every Announcement, Game Reveal & Trailer – Nintendo Life
-



 Science18 hours ago
Science18 hours agoGiant, 82-foot lizard fish discovered on UK beach could be largest marine reptile ever found – Livescience.com




