Health
Diagnosis and acute management of migraine

|
|
See related review article at www.cmaj.ca/lookup/doi/10.1503/cmaj.221607 (to be published February 6, 2023) and a first-person account of the difficulty of finding migraine treatment at www.cmaj.ca/lookup/doi/10.1503/cmaj.221813
KEY POINTS
-
Migraine is a leading cause of disability across all age groups.
-
Routine imaging is not recommended in patients with migraine who have no red flags, atypical symptoms or abnormal findings on neurologic examination.
-
A stratified approach for acute migraine treatment empowers patients to choose from different treatment options depending on attack symptoms and severity and encourages patients to combine medications from different classes.
-
Effective acute migraine treatment includes acetaminophen, nonsteroidal anti-inflammatory drugs and triptans.
-
Ubrogepant and rimegepant are new, effective migraine treatments, suitable for patients with cardiovascular disease in whom triptans are contraindicated.
Migraine affects about 12% of adults, with a prevalence of 18% in women and 6% in men.1–3 Globally, in 2019, migraine was the second leading cause of disability among men and women across all age groups, and the leading cause of disability in women aged 15–49 years (expressed as years lived with disability). 4 In the United States, more than 70% of all migraine-related visits are to primary care providers,5 who play a central role in diagnosing and managing migraine. Recently, several new classes of migraine-specific medications have been shown to be effective and the evidence for the effectiveness of non-pharmacologic interventions is growing. In this article, we discuss the diagnosis and acute management of migraine, based on original research evidence, reviews and clinical practice guidelines (Box 1). We discuss prevention of migraine in a second article.6
Box 1: Evidence used in this review
We conducted a targeted search of Google Scholar and PubMed to identify original research, review articles and clinical practice guidelines published through November of 2021, using search terms that included, but were not limited to, “migraine acute treatment,” “migraine preventive treatment,” “migraine CGRP monoclonal antibodies,” “migraine 5-HT1F,” “migraine behavioural treatments” and “migraine neuromodulation.” We also consulted the most recent guidelines from the Canadian Headache Society and the American Headache Society, and the International Classification of Headache Disorders, 3rd edition.
What is the current understanding of migraine pathophysiology?
Migraine is characterized by neuronal hyperexcitability. Many genetic variants have been associated with increased susceptibility for migraine, suggesting a strong genetic basis.7 Migraine attacks can be broken down into 5 phases: prodrome, aura, headache, postdrome and interictal. However, not every migraine attack progresses through all phases (e.g., only one-third of people with migraine will experience aura) and the phases do not necessarily occur in succession (e.g., aura and headache can occur simultaneously).8,9
The pathophysiology of the headache phase is widely accepted to result from activation of the trigeminovascular pathway, which consists of peripheral trigeminal afferent nerves that innervate the dura and large cerebral arteries. When these neurons are stimulated, they release vasoactive neuropeptides such as calcitonin gene-related peptide (CGRP) and transmit nociceptive signals to the trigeminal nucleus caudalis. Nociceptive signals from the trigeminal nucleus caudalis and the dorsal horn of the upper cervical roots (C1–C2) converge at the trigeminal cervical complex before being relayed to central structures involved in pain processing (brain stem, thalamus, hypothalamus, basal ganglia and cortex).8,9 Levels of CGRP increase during a migraine attack and decrease with treatment and between attacks, and CGRP infusion can trigger a migraine attack.10 Calcitonin gene-related peptide facilitates migraines through various mechanisms, including arterial vasodilation, inflammation in the dura, facilitation of neuronal signalling and modulation of nociceptive signal transmission at the trigeminal cervical complex.10 The hypothesis that migraine can be aborted or prevented by blocking the action of CGRP has been central to the development of drugs that target the CGRP ligand or receptor.11
What are the diagnostic criteria for migraine?
In the third edition of the International Classification of Headache Disorders (ICHD-3), migraine is subclassified into 6 categories: migraine without aura, migraine with aura, chronic migraine, complications of migraine, probable migraine and episodic syndromes that may be associated with migraine.12
Changes from ICHD-2 include modification of migraine with aura so that aura symptoms must meet 3 of 6 aura characteristics (at least 1 aura symptom spreads gradually over 5 min or more, 2 or more aura symptoms occur in succession, each individual aura symptom lasts 5–60 min, at least 1 aura symptom is unilateral, at least 1 aura symptom is positive, the aura is accompanied — or followed within 60 min — by headache), to better distinguish migraine aura from symptoms of transient ischemic attack.13 The diagnosis previously known as basilar artery migraine has been renamed “migraine with brain stem aura,” to reflect the low likelihood that the basilar artery is involved.12 Chronic migraine has been reclassified as a subtype of migraine rather than a complication of migraine, highlighting that it is a distinct entity with unique treatments. Although the diagnostic criteria for chronic migraine still require that headache be present on 15 or more days per month for more than 3 consecutive months, migraine-type headache need be present on only 8 of the headache days each month, in recognition that patients can often experience a mixture of headache phenotypes, including tension-type.12
The Visual Aura Rating Scale (VARS) has been validated for use in distinguishing migraine with visual aura from nonspecific visual symptoms and it has a 91% sensitivity and 96% specificity for diagnosis of visual aura when the score is ≥ 5. The 5 characteristics of the visual symptoms that make up the the scale are duration 6–60 minutes (3 points), develops gradually over 5 minutes or more (2 points), scotoma present (2 points), zigzag line present (2 points) and unilateral (1 point).14
The ID Migraine Screener, a tool that has been validated in primary care, screens for 3 key migraine-associated features: photophobia, functional impairment and nausea (with the mnemonic “PIN the diagnosis”). The screen is positive for migraine if the patient has 2 or more of the features, and a study of 563 patients presenting for routine primary care appointments and reporting headaches in the past 3 months found the sensitivity to be 0.81 (95% confidence interval [CI] 0.77–0.85), specificity to be 0.75 (95% CI 0.64–0.84) and the positive predictive value to be 0.93 (95% CI 0.54–0.82).15
When should imaging be ordered in patients with migraine?
For patients with stable headaches who meet criteria for migraine and have a normal neurologic examination, guidelines from the American College of Radiology and the American Headache Society strongly recommend against routine neuroimaging.16,17 A meta-analysis found that in such patients, the prevalence of important intracranial abnormalities on neuroimaging ranged from 0% to 3.1%, with a combined prevalence of 0.18% (upper 95% CI 0.59%).18 This is comparable to the prevalence of abnormalities detected on neuroimaging among the general population (neoplastic abnormalities 0.7% [95% CI 0.47%–0.98%], nonneoplastic abnormalities 2% [95% CI 1.10%–3.15%]).19 The detection of incidental findings can trigger undue patient anxiety and unnecessary investigations and procedures.16,17
Neuroimaging should be ordered in patients with an abnormal neurologic examination or red flags on history. Headache red flags consist of patient characteristics, features of the headache, and clinical symptoms or signs that should be assessed in every patient presenting with headache. The mnemonic SNOOP4 is a widely used, simple, yet comprehensive way to remember the headache red flags (Table 1).20,21 Neuroimaging should also be ordered in patients with unilateral headache that always occurs on the same side (side-locked), a feature of trigeminal autonomic cephalalgias, which can be mimicked by underlying central nervous system pathologies such as pituitary tumours, intracranial dissections or aneurysms, and infections; aura symptoms that are unusual, prolonged or persistent, a feature that could indicate an underlying lesion or seizure; and post-traumatic headache, because of the increased risk for intracranial hemorrhage or vascular injuries.17
Magnetic resonance imaging (MRI) is preferred over computed tomography (CT) as it provides better visualization of the brain parenchyma and is more sensitive in detecting subtle lesions.22 The use of contrast can further help with visualizing the brain parenchyma and meninges and should be considered when intracranial mass, infection or inflammation are suspected.16 However, CT is preferred when hemorrhages or fractures are suspected and should be performed first when there is concern for an acute abnormality and when MRI is not readily available.22 When headache is accompanied by optic disc edema, CT or MRI with venogram is suggested to rule out cerebral venous sinus thrombosis as a cause of high intracranial pressure.16 In some patients, additional investigations such as lumbar puncture, electroencephalogram and blood work may be indicated, but this is beyond the scope of this review. A comprehensive review of neuroimaging and workup of secondary causes of headache was recently published.23
What is the approach to acute treatment of a migraine attack?
The goal of treatment of migraine attacks is to provide rapid relief from pain and other migraine-related symptoms, to restore patient function and to prevent recurrence. Ideally, treatment should be self-administered, effective, well tolerated and affordable, and require minimal redosing.24 A stratified approach to treatment that empowers patients to choose from different options, depending on attack symptoms and severity, and encourages them to combine medications from different classes (e.g., nonsteroidal anti-inflammatory drugs and triptans) for severe or prolonged attacks, is preferred.25,26 Migraine attacks associated with mild disability can be treated with simple analgesics, with an additional dose of the same or a different agent in the next 2–24 hours, if needed. The Traffic Light of Headache is a tool that can help patients make acute treatment decisions using a stratified treatment plan, according to their level of functional impairment.27 All patients should be educated and screened for medication overuse, which can lead to medication-overuse headache and is a risk factor for transformation of episodic to chronic migraine.25,26
Classic pharmacologic acute treatments for migraine
Guidelines from the Canadian Headache Society and American Headache Society both indicate that acetaminophen, acetylsalicylic acid, diclofenac, ibuprofen, naproxen sodium and triptans have the highest level of evidence for treatment of migraine attacks (Table 2).26,28 Dihydroergotamine, which has been available for decades, can be useful as a first-line agent in some patients (patients with severe attacks or who do not respond well to triptans, or both). However, the Canadian Headache Society recommends against routine use of dihydroergotamine, given potential drug interactions and a high risk of vascular adverse effects, such as bradycardia and prolonged vasoconstriction (coronary, peripheral and central).26 Dihydroergotamine is contraindicated in patients who are pregnant or have a history of peripheral vascular disease, coronary artery disease, uncontrolled hypertension, stroke, sepsis, and renal or hepatic dysfunction.24 The Canadian Headache Society also strongly recommends against the routine use of combination analgesics containing codeine or tramadol, opioids, and butalbital-containing medications, owing to the high risk of sedation, dependence and the development of medication overuse headache.22,26
Table 2:
Traditional medications for acute migraine treatment26
New pharmacologic acute treatment of migraine
Two classes of orally administered small-molecule drugs have recently been approved by the US Food and Drug Administration for the treatment of migraine attacks with and without aura: ditans (lasmiditan) and gepants (ubrogepant and rimegepant) (Table 3). They can be used in patients with cardiovascular disease in whom triptans are contraindicated.29–31 The gepants are currently being considered by Health Canada, but at the present time, lasmiditan will not be marketed in Canada.
Table 3:
New pharmacologic therapies for acute treatment of migraine, with or without aura
The safety and efficacy of each class of drug has been evaluated in phase 3, randomized, placebo-controlled trials, which assessed acute treatment response during a single migraine attack.29,30,32–35 Study design and inclusion and exclusion criteria were similar across the trials. The co-primary outcomes were freedom from pain at 2 hours and resolution of the most bothersome migraine symptom at 2 hours. Inclusion criteria were a minimum 1-year history of migraine or migraine with aura, onset before age 50 years and 2–8 moderate-to-severe migraine headaches per month. Patients were excluded if they had 15 or more headache days per month, a history of medication overuse or a change in their baseline preventive treatment within the previous 3 months. Although patients with cardiovascular risk factors (e.g., obesity, diabetes, dyslipidemia, smoking) were included in all trials, patients with clinically important cardiovascular disease were excluded from all studies except 1 trial that evaluated lasmiditan.30 This is the most notable limitation of these studies, given that the greatest potential advantage of the ditans and gepants is their suitability for use in patients with clinically important cardiovascular disease in whom triptans are contraindicated.
Trial participants had a mean age between 40 and 42 years, 84.0%–88.0% were women and 75.0%–82.5% were white. All 3 drugs met the co-primary outcomes (freedom from pain at 2 h and resolution of the most bothersome migraine symptom at 2 h) compared with placebo, and treatment-related adverse effects were mild and transient (Table 3).29,30,32–35 The most common adverse effects with the gepants were nausea, dizziness, dry mouth and dyspepsia.32,34 Open-label extension trials have not identified any long-term safety or tolerability concerns for up to 1 year.36,37 Dizziness and sedation were the most common adverse effects seen with lasmiditan, resulting in a label warning patients not to drive within 8 hours of its use (Table 3). Ongoing collection of real-world data is needed to monitor for emergence of additional potential adverse effects with use beyond 1 year.
No head-to-head studies have compared ditans or gepants with triptans. However, a recent systematic review and meta-analysis quantified the effect of lasmiditan, rimegepant and ubrogepant compared with triptans in treatment of migraine attacks.38 In terms of efficacy, triptans (except naratriptan 2.5 mg and almotriptan 6.25 mg) were more strongly associated with freedom from pain at 2 hours than lasmiditan (50 mg, 100 mg), rimegepant 75 mg and ubrogepant (50 mg, 100 mg). Patients treated with rizatriptan, sumatriptan and zolmitriptan had more adverse events than patients treated with rimegepant and ubrogepant.38 Patients treated with lasmiditan had more adverse events than most other treatments (triptans and gepants) at all doses, owing to a high incidence of dizziness and sedation. In summary, most triptans are more efficacious than the new drugs, but with similar or poorer tolerability than gepants. Lasmiditan appears to be associated with the most adverse events.
According to current evidence, triptans should remain the mainstay of acute treatment of migraines, while ditans and gepants can be alternatives for patients who cannot tolerate or do not respond well to triptans, as well as patients with cardiovascular disease in whom triptans are contraindicated. As of May 2021, rimegepant was also approved in the US for prevention for episodic migraine, making it the first oral medication with indications for both acute and preventive treatment, the latter being the subject of a subsequent article.6,33,35,39
What are the device- and procedure-related treatment options for migraine?
Neuromodulation devices and peripheral nerve blocks have a role in the management of a small number of patients with migraine. Evidence to support these is discussed in Appendix 1 (available at www.cmaj.ca/lookup/doi/10.1503/cmaj.211969/tab-related-content). Neuromodulation devices, of which 2 are available in Canada, can be used alone or together with pharmacotherapy for the acute treatment of migraine. They are noninvasive and have minimal adverse effects. Peripheral nerve blockade with local anesthetic injection can be performed at various nerve branches of the trigeminocervical system and it is covered by most provincial public health plans in Canada.
Conclusion
Migraine is a leading cause of disability. Treatment of migraine attacks should aim to provide rapid relief from headache pain and related symptoms, restore patient functioning and prevent recurrence. Older medications remain effective, although newer medications may be preferred for certain groups of patients. In Box 2, we provide a practical clinical approach to management of the patient with migraine. Nonpharmacologic and pharmacologic approaches to the prevention of migraine will be discussed in a separate article.6
Box 2: A clinical approach to managing migraine
-
Identify that the primary headache type is migraine.
-
Order brain imaging to exclude secondary causes of headache if red flags or abnormalities on physical examination are present.
-
Categorize the disorder (episodic v. chronic migraine).
-
Identify comorbidities and exacerbating factors.
-
Assess disability and attack characteristics.
-
Review previous treatments, unmet needs and patient’s treatment goals.
-
Formulate a treatment plan.
-
Take a stratified approach to acute migraine treatment.
-
Individualized drugs: choose the medication best suited for the patient; with oral prevention drugs, start low and go slow.
-
Consider comorbidities and coverage for migraine prevention (e.g., consider an antidepressant if patient has comorbid psychological symptoms, avoid divalproex acid in people of childbearing age, be aware that calcitonin gene-related peptide monoclonal antibodies (CGRP mAbs) and onabotulinumtoxinA require a trial of at least 2 oral preventatives before they can be covered by public or private funding and that CGRP mAbs are approved for both episodic and chronic migraine, while onabotulinumtoxinA is approved only for chronic migraine).
-
Footnotes
-
Competing interests: Werner Becker reports receiving consulting fees from AbbView, Novartis, Lundbeck, Eli Lilly, Teva and McKesson, and honoraria for lectures, presentations, manuscript writing and educational events from AbbVie, Novartis, Weber and Weber, Lundbeck and Teva. Dr. Becker serves as a volunteer member on the board of Migraine Canada and on the board of the Pain Society of Alberta. In the past, he has served on the boards of the Canadian Headache Society and the American Headache Society. Tommy Lik Hang Chan reports receiving unrestricted education grants from AbbVie, Teva and Novartis; honoraria from AbbVie, Eli Lilly, Miravo and Novartis; and travel stipends for attending conferences and meetings from AbbVie. Dr. Chan is on the advisory board for AbbVie, Eli Lilly, Teva, Lundbeck, Miravo and Novartis. No other competing interests were declared.
-
This article was solicited and has been peer reviewed.
-
Contributors: All of the authors contributed to the conception and design of the work, drafted the manuscript, revised it critically for important intellectual content, gave final approval of the version to be published and agreed to be accountable for all aspects of the work.
This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY-NC-ND 4.0) licence, which permits use, distribution and reproduction in any medium, provided that the original publication is properly cited, the use is noncommercial (i.e., research or educational use), and no modifications or adaptations are made. See: https://creativecommons.org/licenses/by-nc-nd/4.0/





Health
Quebec successfully pushes back against rise in measles cases – CBC.ca
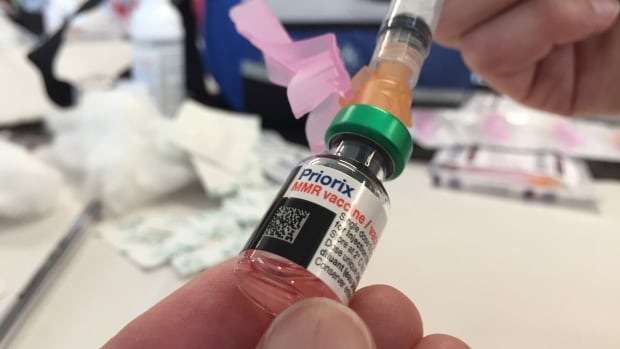
Quebec appears to be winning its battle against the rising tide of measles after 45 cases were confirmed province-wide this year.
“We’ve had no locally transmitted measles cases since March 25, so that’s good news,” said Dr. Paul Le Guerrier, responsible for immunization for Montreal Public Health.
There are 17 patients with measles in Quebec currently, and the most recent case is somebody who was infected while abroad, he said.
But it was no small task to get to this point.
Le Guerrier said once local transmission was detected, news was spread fast among health centres to ensure proper protocols were followed — such as not letting potentially infected people sit in waiting rooms for hours on end.
Then about 90 staffers were put to work, tracking down those who were in contact with positive cases and are not properly vaccinated. They were given post-exposure prophylaxis, which prevents disease, said Le Guerrier.
From there, a vaccination campaign was launched, especially in daycares, schools and neighbourhoods with low inoculation rates. There was an effort to convince parents to get their children vaccinated.
Vaccination in schools boosted
Some schools, mostly in Montreal, had vaccination rates as low as 30 or 40 per cent.
“Vaccination was well accepted and parents responded well,” said Le Guerrier. “Some schools went from very low to as high as 85 to 90 per cent vaccination coverage.”
But it’s not only children who aren’t properly vaccinated. Le Guerrier said people need two doses after age one to be fully inoculated, and he encouraged people to check their status.
There are all kinds of reasons why people aren’t vaccinated, but it’s only about five per cent who are against immunization, he said. So far, some 10,000 people have been vaccinated against measles province-wide during this campaign, Le Guerrier said.
The next step is to continue pushing for further vaccination, but he said, small outbreaks are likely in the future as measles is spreading abroad and travellers are likely to bring it back with them.
Need to improve vaccination rate, expert says
Dr. Donald Vinh, an infectious diseases specialist from the McGill University Health Centre, said it’s not time to rest on our laurels, but this is a good indication that public health is able to take action quickly and that people are willing to listen to health recommendations.
“We are not seeing new cases or at least the new cases are not exceeding the number of cases that we can handle,” said Vinh.
“So these are all reassuring signs, but I don’t think it’s a sign that we need to become complacent.”
Vinh said there are also signs that the public is lagging in vaccine coverage and it’s important to respond to this with improved education and access. Otherwise, microbes capitalize on our weaknesses, he said.
Getting vaccination coverage up to an adequate level is necessary, Vinh said, or more small outbreaks like this will continue to happen.
“And it’s very possible that we may not be able to get one under control if we don’t react quickly enough,” he said.
Health
Pregnant women in the Black Country urged to get whooping cough vaccine – BBC.com


Pregnant women urged to get whooping cough vaccine
Pregnant women in the Black Country are being urged to get vaccinated against whooping cough after a rise in cases.
The bacterial infection of the lungs spreads very easily and can cause serious problems, especially in babies and young children.
The Black Country Integrated Care Board (ICB) is advising pregnant women between 16 and 32 weeks to contact their GP to get the vaccine so their baby has protection from birth.
The UK Health Security Agency warned earlier this year of a steady decline in uptake of the vaccine in pregnant women and children.
Symptoms of the infection, also known as “100-day cough”, are similar to a cold, with a runny nose and sore throat.
Sally Roberts, chief nursing officer for the ICB, which covers Wolverhampton, Dudley, Walsall and Sandwell, said anyone could catch it, but it was more serious for young children and babies.
“Getting vaccinated while you’re pregnant is highly effective in protecting your baby from developing whooping cough in the first few weeks of their life – ideally from 16 weeks up to 32 weeks of pregnancy,” she said.
“If for any reason you miss having the vaccine, you can still have it up until you go into labour.”
Follow BBC West Midlands on Facebook, X and Instagram. Send your story ideas to: newsonline.westmidlands@bbc.co.uk
Health
Measles cases stabilize in Montreal – CityNews Montreal
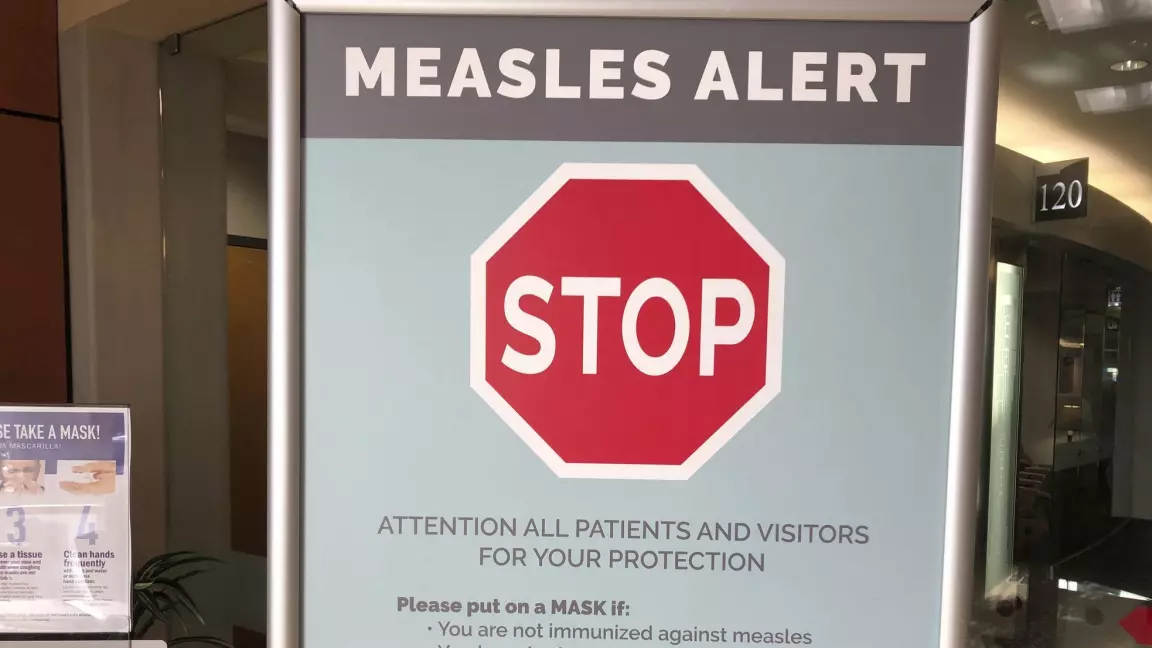
The number of measles cases has stabilized, according to the Montreal Public Health.
Since March 25, there have been no contaminations reported within the community.
“Our teams have identified all contact cases of measles,” said media relations advisor Geneviève Paradis. “It’s a laborious task: each measles case produces hundreds of contacts.”
All community transmission cases since February 2024 have been caused by returning travelers who were either unvaccinated or partially vaccinated.
Currently, there are 18 measles cases in Montreal – with 46 total in Quebec. This according to the April 18 figures from the provincial government.
“With the summer vacations approaching, if you’re travelling, it is essential to check if you are protected against measles,” explained Paradis.
According to Montreal Public Health, a person needs to have received two doses after the age of 12 months to be immunized against the virus.
They’ve launched a vaccination campaign throughout the region, and currently, 11,341 people have been vaccinated against measles in Montreal between March 19 and April 15.
Vaccination is also being provided in schools and at local service points.
“The vaccination operation is under the responsibility of the five CIUSSS of the territory,” concluded Paradis.
-



 Tech23 hours ago
Tech23 hours agoCytiva Showcases Single-Use Mixing System at INTERPHEX 2024 – BioPharm International
-



 Health19 hours ago
Health19 hours agoSupervised consumption sites urgently needed, says study – Sudbury.com
-



 Science5 hours ago
Science5 hours agoJeremy Hansen – The Canadian Encyclopedia
-
News18 hours ago
Canada's 2024 budget announces 'halal mortgages'. Here's what to know – National Post
-
News17 hours ago
2024 federal budget's key takeaways: Housing and carbon rebates, students and sin taxes – CBC News
-



 Tech21 hours ago
Tech21 hours agoNew EV features for Google Maps have arrived. Here’s how to use them. – The Washington Post
-



 Science18 hours ago
Science18 hours agoGiant, 82-foot lizard fish discovered on UK beach could be largest marine reptile ever found – Livescience.com
-
Tech24 hours ago
Nintendo Indie World Showcase April 2024 – Every Announcement, Game Reveal & Trailer – Nintendo Life





