Health
Disrupting viral packaging may be key to pandemic preparedness, Stanford researchers find – Stanford Medical Center Report
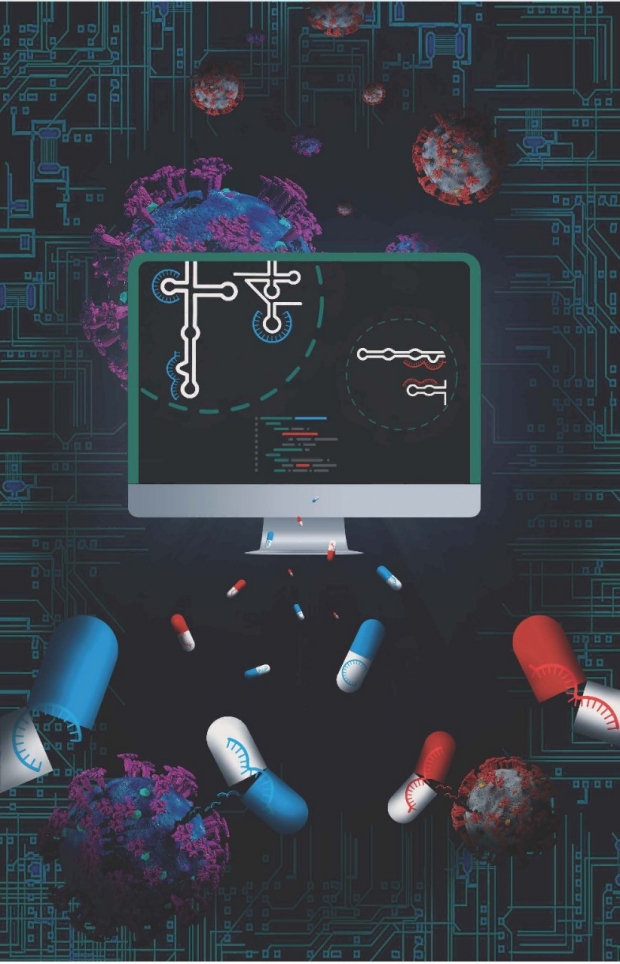
Disrupting a virus’s genome packaging can halt replication and jumpstart a natural immune response against subsequent exposures, a Stanford Medicine study finds.
August 26, 2022
– By Krista Conger
Like savvy international travelers, viruses know exactly how to pack. With the genetic instructions for the next generation folded just so, snuggled into a custom-made outer covering studded with cell-grabbing proteins, these tiny invaders quest for new digs on the reg. When they find them, they get to work. Each newly infected cell soon releases thousands of perfectly packed, fresh-faced viral particles — fueling an infection’s exponential growth.
Now a Stanford Medicine study of influenza and of SARS-CoV-2 — the virus that causes COVID-19 — shows that antiviral drugs that disrupt this game of genomic Tetris can bring infections to a screeching halt. At the same time, these drugs allow just enough exposure to the virus to jumpstart a natural immune response that confers lasting protection.
Because tried-and-true packing strategies are shared among viral family members, one antiviral drug can be effective against several closely related viruses, such as seasonal influenza A, swine flu and bird flu. And because it’s difficult to rejigger a three-dimensional puzzle, viruses are unlikely to become resistant to a treatment that harnesses this tactic.
“These antivirals can be tailored to nearly any virus,” Jeffrey Glenn, MD, PhD, professor of microbiology and immunology, said. “They provide immediate protection when administered either prior to or after exposure, and they stimulate a lasting immune response that neutralizes a subsequent challenge of even a tenfold lethal dose of influenza. This is really exciting.”
The study, which was conducted in mice, hamsters and human cells grown in the laboratory, was published online in Nature Medicine Aug. 18. Glenn, the Joseph D. Grant Professor II, is the senior author of the study. Research scientist Rachel Hagey, PhD, is the lead author of the paper.
A tool for the next pandemic
The discovery suggests the possibility of quickly dampening the spread of some of humankind’s deadliest viruses with off-the-shelf custom antivirals designed, manufactured and stockpiled before the next outbreak occurs.
The findings are the first to come out of Stanford’s newly formed SyneRx, which is one of nine Antiviral Drug Discovery Centers for Pathogens of Pandemic Concern funded by the National Institute for Allergy and Infectious Diseases, and ViRx@Stanford, which is Stanford Medicine’s Biosecurity and Pandemic Preparedness Initiative. Glenn leads the center, which received $69 million in May to help design antivirals to combat COVID-19 and other diseases with the potential to cause future pandemics.
Vaccines that fight viruses typically encourage the body’s immune system to recognize and react to critical viral proteins, such as the spike protein of SARS-CoV-2. But, as has become obvious during the ongoing pandemic, proteins can mutate in subtle ways to evade the immune system, leading to breakthrough infections in vaccinated people.


Jeffrey Glenn
Glenn and Hagey wondered if antiviral drugs targeting more mundane, but equally important, steps in the viral life cycle could stop or slow infections — genome packaging, for example. After all, packing may be boring, but it’s key to a successful trip, whether you’re going to Paris or to the cell next door. And it can be surprisingly complex.
The genome of influenza A virus, for instance, consists of eight separate, single-stranded RNA segments. Each segment folds on itself in a bespoke combination of stems and loops dictated by the sequence of their building blocks, called nucleotides. Viral protein butlers then collaborate to tidily tuck one of each of the eight segments into an outer shell, much the way parents fit a college-bound child’s belongings into the back of the car. The new viral particle is then ready for its maiden voyage to continue the cycle of infection. Other viruses have other packing requirements. But once a successful blueprint has been committed to memory, it is unlikely to be jettisoned, and it is shared among family members like a favorite recipe.
The researchers used a type of analysis called SHAPE and computational modeling to identify a segment of RNA called PSL2 with a predicted three-dimensional structure that is nearly 100% identical among various seasonal and pandemic influenza A strains. When they mutated the sequence of PSL2, the virus was unable to infect cells grown in the laboratory — confirming the importance of the region to viral replication.
Hagey and her colleagues then designed several short stretches of single-stranded DNA that would recognize and bind to matching sequences on PSL2 — latching onto and interfering with its ability to contort itself into the precisely defined shape necessary for successful packing. They designed the DNA pieces to resist degradation and last longer in the body using a technique called locked nucleic acids, or LNAs.
Nowhere to go
The researchers found that treating the laboratory-grown cells with certain LNAs either before or after infection with an influenza strain called H1N1, or swine flu, dramatically reduced the ability of the virus to make new infectious particles. Additionally, they saw no signs of the virus mutating to escape the effects of the LNA even after several generations. In contrast, when they treated the cells with Tamiflu, the virus quickly altered its genome to sidestep the anti-influenza drug, which inhibits the activity of a viral protein that facilitates the release of new viral particles from an infected cell.
“We found that if we design drugs against these highly conserved structures necessary for viral genome packaging, there are very few ways the virus can escape,” Glenn said. “This structure is shared in every known isolate of influenza A, including bird flu and swine flu. So, if we are able to translate these findings into humans, it’s possible we could see universal protection with just one dose.”
The researchers then tested whether laboratory mice would be protected against influenza infection by the most effective LNA. They found that a single dose of the antiviral administered in the animals’ noses one week before exposure to a lethal dose of the virus protected 100% of the treated animals from death. In contrast, the control animals became severely ill and were all humanely sacrificed by day six. They then increased the dose of the LNA and administered it two weeks before virus exposure. Again, none of the mice died, and most were only mildly ill.
Finally, the researchers explored whether the low-level viral replication experienced by the mice in the first series of experiments could protect them from future infection. Sixty-five days after their initial infection, the researchers exposed the same mice again, but with 10 times the normal lethal dose.
“They didn’t bat an eye,” Glenn said. “They didn’t lose weight or appear sick at all. This indicates their initial exposure led to enough residual viral replication to stimulate a broad immune response that remains protective months later.”
A check on COVID-19
The researchers conducted a similar series of experiments with the SARS-CoV-2 virus. As with influenza, they found that LNAs targeting highly conserved structured regions important in the viral genome inhibited the replication of the virus in human cells grown in the laboratory. Even a highly mutated version of the SARS-CoV-2 virus isolated from a chronically infected cancer patient was unable to replicate in the presence of the antiviral.
The protective effect extended to Syrian hamsters, an animal commonly used to study SARS-CoV-2 infection. Hamsters given two single daily sniffs of the LNA before romping with infected peers remained healthy and, after four days, had dramatically less virus in their lungs than control animals.
The researchers are now testing the approach in pigs, using the same dose and intra-nasal applicators they hope to one day use in humans. They foresee a time during the next pandemic when strategically designed LNAs, which they term programmable antivirals, could be used to treat already infected people, to protect people during the lag between vaccination and the development of protective immunity, or to provide prophylactic protection if there is no available vaccine.
“COVID-19 caught us with our pants down,” Glenn said. “But what really keeps me up at night is the likelihood of a highly pathogenic virus like the 1918 influenza pandemic or a new, weaponized version of influenza. Today we have nothing to stop its spread, and a virus like that could kill hundreds of millions of people. But our approach could be enacted ahead of time and provide protection against a wide range of viruses.”
Researchers from the University of North Carolina at Chapel Hill; Utah State University; the University of Cincinnati College of Medicine; the University of Texas Medical Branch; the National Institute of Allergy and Infectious Diseases; the Chan Zuckerberg Biohub; and the Veterans Administration Medical Center, Palo Alto, also contributed to the study.
The study was supported by the National Institutes of Health (grants 5T32AI007328-24, 5T32DK007056, R56A1111460, U19A1109662, RO1AI132191 and U19AI171421), the Department of Defense, an influenza Harrington Scholar Innovator grant, a COVID-19 Harrington Scholar Innovator grant, a Mona M. Burgess Stanford Bio-X Interdisciplinary graduate fellowship, Fastgrants and the Dr. Tri Cao Nguyen Fund for Pandemic Preparedness.
Stanford Medicine integrates research, medical education and health care at its three institutions – Stanford School of Medicine, Stanford Health Care, and Stanford Children’s Health. For more information, please visit the Office of Communications website at http://mednews.stanford.edu.
Health
Cancer Awareness Month – Métis Nation of Alberta


Cancer Awareness Month
Posted on: Apr 18, 2024
April is Cancer Awareness Month
As we recognize Cancer Awareness Month, we stand together to raise awareness, support those affected, advocate for prevention, early detection, and continued research towards a cure. Cancer is the leading cause of death for Métis women and the second leading cause of death for Métis men. The Otipemisiwak Métis Government of the Métis Nation Within Alberta is working hard to ensure that available supports for Métis Citizens battling cancer are culturally appropriate, comprehensive, and accessible by Métis Albertans at all stages of their cancer journey.
Receiving a cancer diagnosis, whether for yourself or a loved one, can feel overwhelming, leaving you unsure of where to turn for support. In June, our government will be launching the Cancer Supports and Navigation Program which will further support Métis Albertans and their families experiencing cancer by connecting them to OMG-specific cancer resources, external resources, and providing navigation support through the health care system. This program will also include Métis-specific peer support groups for those affected by cancer.
With funding from the Canadian Partnership Against Cancer (CPAC) we have also developed the Métis Cancer Care Course to ensure that Métis Albertans have access to culturally safe and appropriate cancer services. This course is available to cancer care professionals across the country and provides an overview of who Métis people are, our culture, our approaches to health and wellbeing, our experiences with cancer care, and our cancer journey.
Together, we can make a difference in the fight against cancer and ensure equitable access to culturally safe and appropriate care for all Métis Albertans. Please click on the links below to learn more about the supports available for Métis Albertans, including our Compassionate Care: Cancer Transportation program.
I wish you all good health and happiness!
Bobbi Paul-Alook
Secretary of Health & Seniors
Health
Type 2 diabetes is not one-size-fits-all: Subtypes affect complications and treatment options – The Conversation


You may have heard of Ozempic, the “miracle drug” for weight loss, but did you know that it was actually designed as a new treatment to manage diabetes? In Canada, diabetes affects approximately 10 per cent of the general population. Of those cases, 90 per cent have Type 2 diabetes.
This metabolic disorder is characterized by persistent high blood sugar levels, which can be accompanied by secondary health challenges, including a higher risk of stroke and kidney disease.
Locks and keys
In Type 2 diabetes, the body struggles to maintain blood sugar levels in an acceptable range. Every cell in the body needs sugar as an energy source, but too much sugar can be toxic to cells. This equilibrium needs to be tightly controlled and is regulated by a lock and key system.
In the body’s attempt to manage blood sugar levels and ensure that cells receive the right amount of energy, the pancreatic hormone, insulin, functions like a key. Cells cover themselves with locks that respond perfectly to insulin keys to facilitate the entry of sugar into cells.
Unfortunately, this lock and key system doesn’t always perform as expected. The body can encounter difficulties producing an adequate number of insulin keys, and/or the locks can become stubborn and unresponsive to insulin.
All forms of diabetes share the challenge of high blood sugar levels; however, diabetes is not a singular condition; it exists as a spectrum. Although diabetes is broadly categorized into two main types, Type 1 and Type 2, each presents a diversity of subtypes, especially Type 2 diabetes.
These subtypes carry their own characteristics and risks, and do not respond uniformly to the same treatments.
To better serve people living with Type 2 diabetes, and to move away from a “one size fits all” approach, it is beneficial to understand which subtype of Type 2 diabetes a person lives with. When someone needs a blood transfusion, the medical team needs to know the patient’s blood type. It should be the same for diabetes so a tailored and effective game plan can be implemented.
This article explores four unique subtypes of Type 2 diabetes, shedding light on their causes, complications and some of their specific treatment avenues.
Severe insulin-deficient diabetes: We’re missing keys!
(Lili Grieco-St-Pierre, Jennifer Bruin/Created with BioRender.com)
Insulin is produced by beta cells, which are found in the pancreas. In the severe insulin-deficient diabetes (SIDD) subtype, the key factories — the beta cells — are on strike. Ultimately, there are fewer keys in the body to unlock the cells and allow entry of sugar from the blood.
SIDD primarily affects younger, leaner individuals, and unfortunately, increases the risk of eye disease and blindness, among other complications. Why the beta cells go on strike remains largely unknown, but since there is an insulin deficiency, treatment often involves insulin injections.
Severe insulin-resistant diabetes: But it’s always locked!
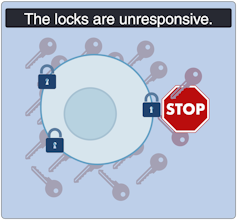
(Lili Grieco-St-Pierre, Jennifer Bruin/Created with BioRender.com)
In the severe insulin-resistant diabetes (SIRD) subtype, the locks are overstimulated and start ignoring the keys. As a result, the beta cells produce even more keys to compensate. This can be measured as high levels of insulin in the blood, also known as hyperinsulinemia.
This resistance to insulin is particularly prominent in individuals with higher body weight. Patients with SIRD have an increased risk of complications such as fatty liver disease. There are many treatment avenues for these patients but no consensus about the optimal approach; patients often require high doses of insulin.
Mild obesity-related diabetes: The locks are sticky!

(Lili Grieco-St-Pierre, Jennifer Bruin/Created with BioRender.com)
Mild obesity-related (MOD) diabetes represents a nuanced aspect of Type 2 diabetes, often observed in individuals with higher body weight. Unlike more severe subtypes, MOD is characterized by a more measured response to insulin. The locks are “sticky,” so it is challenging for the key to click in place and open the lock. While MOD is connected to body weight, the comparatively less severe nature of MOD distinguishes it from other diabetes subtypes.
To minimize complications, treatment should include maintaining a healthy diet, managing body weight, and incorporating as much aerobic exercise as possible. This is where drugs like Ozempic can be prescribed to control the evolution of the disease, in part by managing body weight.
Mild age-related diabetes: I’m tired of controlling blood sugar!
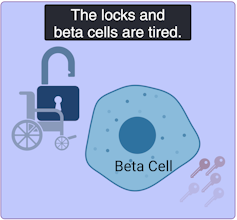
(Lili Grieco-St-Pierre, Jennifer Bruin/Created with BioRender.com)
Mild age-related diabetes (MARD) happens more often in older people and typically starts later in life. With time, the key factory is not as productive, and the locks become stubborn. People with MARD find it tricky to manage their blood sugar, but it usually doesn’t lead to severe complications.
Among the different subtypes of diabetes, MARD is the most common.
Unique locks, varied keys
While efforts have been made to classify diabetes subtypes, new subtypes are still being identified, making proper clinical assessment and treatment plans challenging.
In Canada, unique cases of Type 2 diabetes were identified in Indigenous children from Northern Manitoba and Northwestern Ontario by Dr. Heather Dean and colleagues in the 1980s and 90s. Despite initial skepticism from the scientific community, which typically associated Type 2 diabetes with adults rather than children, clinical teams persisted in identifying this as a distinct subtype of Type 2 diabetes, called childhood-onset Type 2 diabetes.
Read more:
Indigenous community research partnerships can help address health inequities
Childhood-onset Type 2 diabetes is on the rise across Canada, but disproportionately affects Indigenous youth. It is undoubtedly linked to the intergenerational trauma associated with colonization in these communities. While many factors are likely involved, recent studies have discovered that exposure of a fetus to Type 2 diabetes during pregnancy increases the risk that the baby will develop diabetes later in life.
Acknowledging this distinct subtype of Type 2 diabetes in First Nations communities has led to the implementation of a community-based health action plan aimed at addressing the unique challenges faced by Indigenous Peoples. It is hoped that partnered research between communities and researchers will continue to help us understand childhood-onset Type 2 diabetes and how to effectively prevent and treat it.
A mosaic of conditions
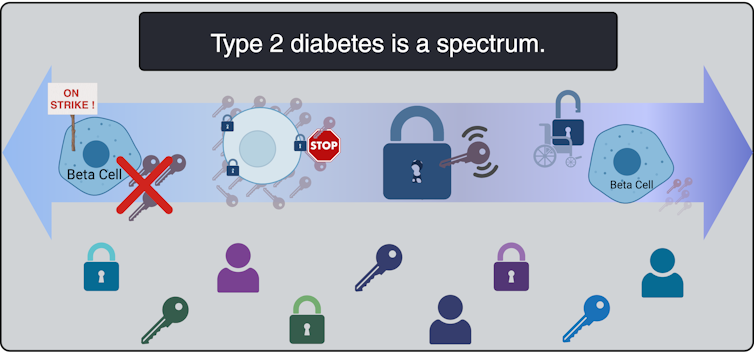
(Lili Grieco-St-Pierre, Jennifer Bruin/Created with BioRender.com)
Type 2 diabetes is not uniform; it’s a mosaic of conditions, each with its own characteristics. Since diabetes presents so uniquely in every patient, even categorizing into subtypes does not guarantee how the disease will evolve. However, understanding these subtypes is a good starting point to help doctors create personalized plans for people living with the condition.
While Indigenous communities, lower-income households and individuals living with obesity already face a higher risk of developing Type 2 diabetes than the general population, tailored solutions may offer hope for better management. This emphasizes the urgent need for more precise assessments of diabetes subtypes to help customize therapeutic strategies and management strategies. This will improve care for all patients, including those from vulnerable and understudied populations.
Health
Quebec successfully pushes back against rise in measles cases – CBC.ca
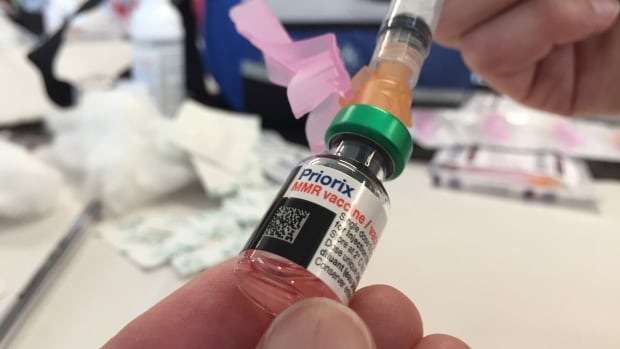
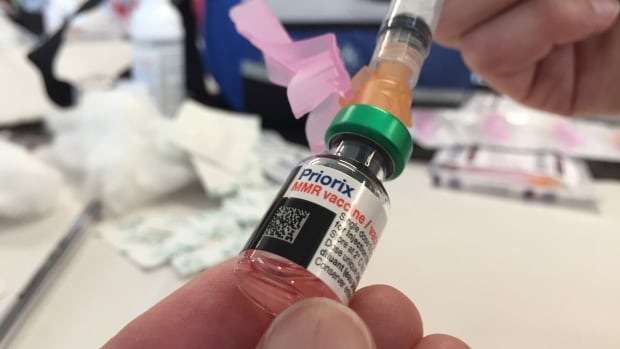
Quebec appears to be winning its battle against the rising tide of measles after 45 cases were confirmed province-wide this year.
“We’ve had no locally transmitted measles cases since March 25, so that’s good news,” said Dr. Paul Le Guerrier, responsible for immunization for Montreal Public Health.
There are 17 patients with measles in Quebec currently, and the most recent case is somebody who was infected while abroad, he said.
But it was no small task to get to this point.
Le Guerrier said once local transmission was detected, news was spread fast among health centres to ensure proper protocols were followed — such as not letting potentially infected people sit in waiting rooms for hours on end.
Then about 90 staffers were put to work, tracking down those who were in contact with positive cases and are not properly vaccinated. They were given post-exposure prophylaxis, which prevents disease, said Le Guerrier.
From there, a vaccination campaign was launched, especially in daycares, schools and neighbourhoods with low inoculation rates. There was an effort to convince parents to get their children vaccinated.
Vaccination in schools boosted
Some schools, mostly in Montreal, had vaccination rates as low as 30 or 40 per cent.
“Vaccination was well accepted and parents responded well,” said Le Guerrier. “Some schools went from very low to as high as 85 to 90 per cent vaccination coverage.”
But it’s not only children who aren’t properly vaccinated. Le Guerrier said people need two doses after age one to be fully inoculated, and he encouraged people to check their status.
There are all kinds of reasons why people aren’t vaccinated, but it’s only about five per cent who are against immunization, he said. So far, some 10,000 people have been vaccinated against measles province-wide during this campaign, Le Guerrier said.
The next step is to continue pushing for further vaccination, but he said, small outbreaks are likely in the future as measles is spreading abroad and travellers are likely to bring it back with them.
Need to improve vaccination rate, expert says
Dr. Donald Vinh, an infectious diseases specialist from the McGill University Health Centre, said it’s not time to rest on our laurels, but this is a good indication that public health is able to take action quickly and that people are willing to listen to health recommendations.
“We are not seeing new cases or at least the new cases are not exceeding the number of cases that we can handle,” said Vinh.
“So these are all reassuring signs, but I don’t think it’s a sign that we need to become complacent.”
Vinh said there are also signs that the public is lagging in vaccine coverage and it’s important to respond to this with improved education and access. Otherwise, microbes capitalize on our weaknesses, he said.
Getting vaccination coverage up to an adequate level is necessary, Vinh said, or more small outbreaks like this will continue to happen.
“And it’s very possible that we may not be able to get one under control if we don’t react quickly enough,” he said.
-



 Science10 hours ago
Science10 hours agoJeremy Hansen – The Canadian Encyclopedia
-



 Investment10 hours ago
Investment10 hours agoUK Mulls New Curbs on Outbound Investment Over Security Risks – BNN Bloomberg
-



 Tech9 hours ago
Tech9 hours agoSave $700 Off This 4K Projector at Amazon While You Still Can – CNET
-



 Tech8 hours ago
Tech8 hours ago'Kingdom Come: Deliverance II' Revealed In Epic New Trailer And It Looks Incredible – Forbes
-



 Sports8 hours ago
Sports8 hours agoAuston Matthews denied 70th goal as depleted Leafs lose last regular-season game – Toronto Sun
-
Real eState9 hours ago
Sick of Your Blue State? These Real Estate Agents Have Just the Place for You. – The New York Times
-



 Health24 hours ago
Health24 hours agoSupervised consumption sites urgently needed, says study – Sudbury.com
-
News23 hours ago
Canada's 2024 budget announces 'halal mortgages'. Here's what to know – National Post






