Health
Doctors suggest new names for low-grade prostate cancer | Loop Cayman Islands – Loop News Cayman
A cancer diagnosis is scary. Some doctors say it’s time to rename low-grade prostate cancer to eliminate the alarming C-word.
Cancer cells develop in nearly all prostates as men age, and most prostate cancers are harmless. About 34,000 Americans die from prostate cancer annually, but treating the disease can lead to sexual dysfunction and incontinence.
Changing the name could lead more low-risk patients to skip unnecessary surgery and radiation.
“This is the least aggressive, wimpiest form of prostate cancer that is literally incapable of causing symptoms or spreading to other parts of the body,” said University of Chicago Medicine’s Dr Scott Eggener, who is reviving a debate about how to explain the threat to worried patients.
The words “You have cancer” have a profound effect on patients, Eggener wrote Monday in the Journal of Clinical Oncology.
He and his co-authors say fear of the disease can cause some patients to overreact and opt for unneeded surgery or radiation.
Others agree.
“If you reduce anxiety, you’ll reduce overtreatment,” said Dr David Penson of Vanderbilt University. “The word ‘cancer’ puts an idea in their head: ‘I have to have this treated.'”
Diagnosis sometimes starts with a PSA blood test, which looks for high levels of a protein that may mean cancer but can also be caused by less serious prostate problems or even vigorous exercise.
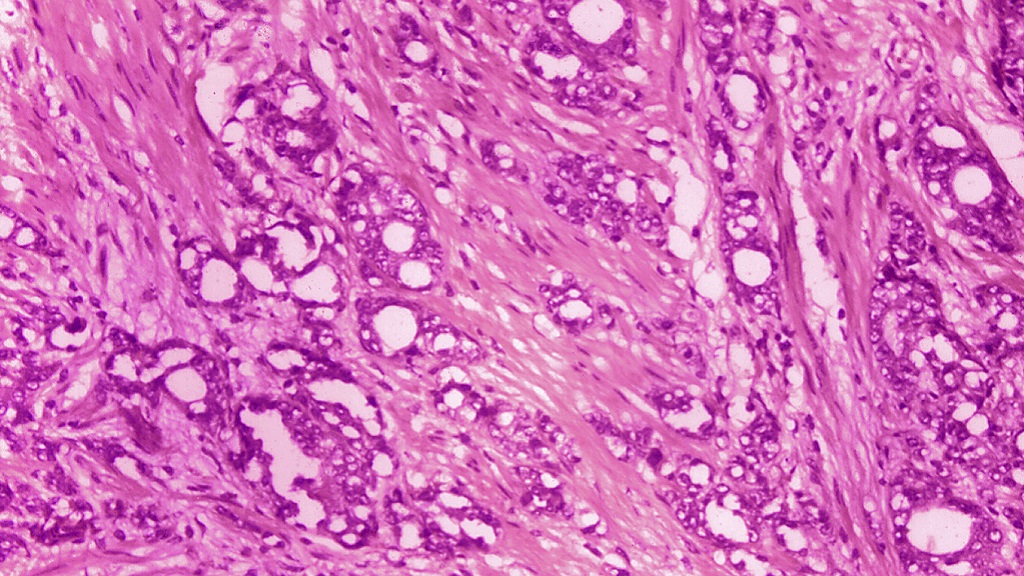
When a patient has a suspicious test result, a doctor might recommend a biopsy, which involves taking samples of tissue from the prostate gland. Next, a pathologist looks under a microscope and scores the samples for how abnormal the cells look.
Often, doctors offer patients with the lowest score — Gleason 6 — a way to avoid surgery and radiation: active surveillance, which involves close monitoring but no immediate treatment.
In the US, about 60 per cent of low-risk patients choose active surveillance. But they might still worry.
“I would be over the moon if people came up with a new name for Gleason 6 disease,” Penson said. “It will allow a lot of men to sleep better at night.”
But Dr Joel Nelson of the University of Pittsburgh School of Medicine said dropping the word “cancer” would “misinform patients by telling them there’s nothing wrong. There’s nothing wrong today, but that doesn’t mean we don’t have to keep track of what we’ve discovered.”
Name changes have happened previously in low-risk cancers of the bladder, cervix and thyroid. In breast cancer, there’s an ongoing debate about dropping “carcinoma” from DCIS or ductal carcinoma in situ.
In prostate cancer, the 1960s-era Gleason ranking system has evolved, which is how 6 became the lowest score. Patients may assume it’s a medium score on a scale of 1 to 10. In fact, it’s the lowest on a scale of 6 to 10.
What to call it instead of cancer? Proposals include IDLE for indolent lesion of epithelial origin or INERRT for indolent neoplasm rarely requiring treatment.
“I don’t really give a hoot what it’s called as long as it’s not called cancer,” Eggener said.
Steve Rienks, a 72-year-old civil engineer in Naperville, Illinois, was diagnosed with Gleason 6 prostate cancer in 2014. He chose active surveillance, and follow-up biopsies in 2017 and 2021 found no evidence of cancer.
Calling it something else would help patients make informed choices, Rienks said, but that’s not enough: Patients need to ask questions until they feel confident.
“It’s about understanding risk,” Rienks said. “I would encourage my fellow males to educate themselves and get additional medical opinions.”
___
By CARLA K JOHNSON
AP Medical Writer
Health
New technology to advance women’s cancer care at Southlake


|
|
NEWS RELEASE
SOUTHLAKE REGIONAL HEALTH CENTRE
**************************
This Cancer Awareness Month, Southlake is adding advanced technologies to detect and treat breast cancer and other women’s cancers thanks to generous community donor support, most recently through the HERE is Where Cancer Meets its Match campaign. New cancer care technology, including new mammography machines, the MyoSure System and the MOLLI 2® System will make a measurable impact in diagnosing and treating women’s cancers in the communities Southlake serves.
Southlake is installing three new mammography machines to expand its breast cancer screening program to 1,500 more women each year. Two of these machines have new biopsy capabilities that will reduce the number of cancelled exams due to equipment failure, ensuring timely care for women. Women ages 40 to 49 years old will be able to self-refer for publicly funded mammograms through the Ontario Breast Screening Program starting this fall.
“Early detection is critical when treating breast cancer and other women’s cancers,” said Lorrie Reynolds, Director, Regional Cancer Program at Southlake. “We treat more than 1,700 breast cancer patients at Southlake every year. By adding advanced technology, like the new mammography machines, we’re ensuring women have the best experience at Southlake.”
Southlake is also introducing the MyoSure System, an innovative technology that can help detect female reproductive cancers. Damaged tissue in a woman’s uterus such as fibroids and polyps can now be removed in a precise, minimally invasive procedure that leaves the rest of the uterus intact. This will improve the overall patient experience by supporting faster recovery, reducing the risk of infection and giving more women the option to have children. An estimated 200 women per year will benefit from the MyoSure System.
The new mammography machines and the MyoSure System build on Southlake’s recent investment in the MOLLI 2® System, a made-in-Canada wire-free breast localization technology. This technology is considerably less invasive and more accurate when compared to wire-guided localization, resulting in a better patient experience and improved cosmetic outcomes. More than 200 women each year will benefit from this innovative medical device as they are treated for breast cancer at Southlake.
“As a clinician caring for women with cancer in our community, I’m incredibly proud of the work Southlake is doing to advance women’s health and improve patient experiences,” said Sara Temple, MD, Surgical Oncologist and Chief of Surgery at Southlake. “Women who visit Southlake can be confident that they are receiving leading edge care, close to home when they need it most.”
The World Health Organization anticipates a 77 per cent increase in cancer diagnoses by 2050. Southlake serves some of the fastest growing communities in Canada and anticipates that the number of patients requiring cancer care will grow. By investing in new technology, Southlake is ensuring that women in the communities it serves have access to leading edge cancer care. All of these investments were funded with support from community donors who generously gave to Southlake to support investments into women’s health at the hospital.
“The generosity of our donor community and the impact they have made for women receiving cancer diagnosis and treatment at Southlake is something we can all take great pride in,” said Jennifer Ritter, President and CEO of Southlake Foundation. “From our Women’s Health Initiative donors supporting new mammography machines, to the Ladies in Philanthropy for Southlake funding the MOLLI 2 System, to our long-standing partners The Edge Benefits and Pheasant Run Golf Club enabling the introduction of MyoSure System through their joint annual charity golf tournament, we are incredibly lucky to share a vision of access to exceptional care for everyone who depends on Southlake when they need us most. Thank you, to every donor who contributed to these important upgrades to care for women.”
Southlake Foundation’s HERE is Where Cancer Meets its Match campaign supports the Stronach Regional Cancer Centre at Southlake. For more information or to make a donation, visit: southlake.ca/HERE.





Health
Pasteurized milk includes remnants of H5N1 bird flu, U.S. officials say


|
|
The U.S. Food and Drug Administration says that samples of pasteurized milk have tested positive for remnants of the bird flu virus that has infected dairy cows.
The agency stressed that the material is inactivated and that the findings “do not represent actual virus that may be a risk to consumers.” Officials added that they’re continuing to study the issue.
“To date, we have seen nothing that would change our assessment that the commercial milk supply is safe,” the FDA said in a statement on Tuesday.
The announcement comes nearly a month after an avian influenza virus that has sickened millions of wild and commercial birds in recent years was detected in dairy cows in at least eight states. The Agriculture Department (USDA) says 33 herds have been affected to date.
FDA officials didn’t indicate how many samples they tested or where they were obtained. The agency has been evaluating milk during processing and from grocery stores, officials said. Results of additional tests are expected in “the next few days to weeks.”
WATCH | Bird flu spread in U.S. cows:
For the first time ever, avian influenza, or H5N1 bird flu, was detected in roughly a dozen dairy cow herds across the U.S. About That producer Lauren Bird explores why scientists and public health officials are concerned about the cross-species transmission and whether humans are now at higher risk.
The polymerase chain reaction (PCR) lab test the FDA used would have detected viral genetic material even after live virus was killed by pasteurization, or heat treatment, said Lee-Ann Jaykus, an emeritus food microbiologist and virologist at North Carolina State University
“There is no evidence to date that this is infectious virus, and the FDA is following up on that,” Jaykus said.
Officials with the FDA and the USDA had previously said milk from affected cattle did not enter the commercial supply. Milk from sick animals is supposed to be diverted and destroyed. Federal regulations require milk that enters interstate commerce to be pasteurized.
Tests for viable virus underway, agency says
Because the detection of the bird flu virus known as Type A H5N1 in dairy cattle is new and the situation is evolving, no studies on the effects of pasteurization on the virus have been completed, FDA officials said. But past research shows that pasteurization is “very likely” to inactivate heat-sensitive viruses like H5N1, the agency added.
The agency said it has been evaluating milk from affected animals, in the processing system and on the shelves. It said it is completing a large, representative national sample to understand the extent of the findings.
Matt Herrick, a spokesperson for the International Dairy Foods Association, said that time and temperature regulations for pasteurization ensure that the commercial U.S. milk supply is safe. Remnants of the virus “have zero impact on human health,” he wrote in an email.
Scientists confirmed the H5N1 virus in dairy cows in March after weeks of reports that cows in Texas were suffering from a mysterious malady. The cows were lethargic and saw a dramatic reduction in milk production. Although the H5N1 virus is lethal to commercial poultry, most infected cattle seem to recover within two weeks, experts said.
To date, two people in the U.S. have been infected with bird flu. A Texas dairy worker who was in close contact with an infected cow recently developed a mild eye infection and has recovered. In 2022, a prison inmate in a work program caught it while killing infected birds at a Colorado poultry farm. His only symptom was fatigue, and he recovered.





Health
Remnants of bird flu virus found in pasteurized milk, FDA says


|
|
The U.S. Food and Drug Administration said Tuesday that samples of pasteurized milk had tested positive for remnants of the bird flu virus that has infected dairy cows.
The agency stressed that the material is inactivated and that the findings “do not represent actual virus that may be a risk to consumers.” Officials added that they’re continuing to study the issue.





-



 Health18 hours ago
Health18 hours agoRemnants of bird flu virus found in pasteurized milk, FDA says
-



 Health23 hours ago
Health23 hours agoBird flu virus found in grocery milk as officials say supply still safe
-
News15 hours ago
Amid concerns over ‘collateral damage’ Trudeau, Freeland defend capital gains tax change
-
Art19 hours ago
Random: We’re In Awe of Metaphor: ReFantazio’s Box Art
-



 Investment23 hours ago
Investment23 hours agoTaxes should not wag the tail of the investment dog, but that’s what Trudeau wants
-
News23 hours ago
Peel police chief met Sri Lankan officer a court says ‘participated’ in torture – Global News
-
Art12 hours ago
The unmissable events taking place during London’s Digital Art Week
-
Media18 hours ago
Vaughn Palmer: B.C. premier gives social media giants another chance





