Health
Hirji worried Niagara is abandoning COVID-19 prevention – NiagaraFallsReview.ca

He has fretted about it for weeks, and recent behaviour by Niagara residents taking advantage of warm weather and the economic reopening has done little to ease the fears of Dr. Mustafa Hirji.
Over the weekend, as the temperature rose above 30 C and businesses everywhere reopened, people who have been in pandemic lockdown for months gathered on patios and beaches.
But photos of some of those places, including some Niagara beaches, bespoke a lack of concern for infection control. Physical distancing and masks appear to be the exception rather than the rule in some locations. And given how COVID-19 has spread easily among big gatherings in the United States, Hirji worries about the increased spread of the novel coronavirus in Niagara.
“I worry about this a lot,” said Hirji. “It does seem that some people are taking the reopening as a sign that this is over, and they can, you know, return to their previous behaviours. But that is not the case. The pandemic is not over.”
Hirji said Stage 2 of the reopening is not written in stone. If cases spike, the region can be forced back into lockdown. And even if the reopening doesn’t collapse, Niagara is a long way from a pre-pandemic normal.
“It is a slow, phased-in approach. We have to get through Phase 2 without having to reimpose those measures and then go onto Phase 3,” he said. “Beyond that is going to be the new normal that will have to persist until we have a vaccine.”
That said, Hirji said Niagara is not Florida, where beachgoers helped fuel viral spread, and the risk here is lower than it is in the Sunshine State. Where Florida never got control of the virus spread before reopening Niagara sees a low daily case count.
On Thursday, for instance, Niagara had three new confirmed COVID-19 cases. Two were connected to a previous case and the other is an essential worker who is employed on the American side of the border.
In Florida, the daily case count is presently in the thousands.
Despite his concerns, however, Hirji remains disinclined to follow the actions of his Guelph counterpart or his colleagues in Alberta in calling for mandatory masking in public.
In Guelph, the medical officer of health issued an order making masks mandatory in businesses for customers and staff. And in Alberta, every medical officer of health in the province has urged the provincial government to make masks mandatory in public after a rise in cases in some jurisdictions.
Hirji said nothing in the past week has changed his previous view that it is not the place of the public health department to issue such a sweeping order that should come from elected officials.
Moreover, he said while masks are useful, they are not the fool-proof anti-virus shield some people appear to believe they are.
“Masks are your second line of defence,” Hirji said. “Why would you make your second line of defence mandatory but not your first and best line of defence, which is physical distancing?”
He said people have become “enamoured” with masks, but points out their recommended use is as an extra layer of protection when physical distancing is not possible. They are not meant to take the place of physical distancing.
Get more from the Niagara Falls Review in your inbox
Never miss the latest news from the Niagara Falls Review. Sign up for our email newsletters to get the day’s top stories, your favourite columnists, and much more in your inbox.
Hirji said as the reopening of the economy heads into its first full week, the health department has been receiving calls about businesses or other locations where infection control measures — including distancing and masking — are not being followed.
“If you see that happening, our recommendation is that first, you raise it with the business owner or manager and if you want to take a step further, you should bring it to the attention of your municipality’s bylaw office and they will handle it,” Hirji said.
Health
Pregnant women in the Black Country urged to get whooping cough vaccine – BBC.com


Pregnant women urged to get whooping cough vaccine
Pregnant women in the Black Country are being urged to get vaccinated against whooping cough after a rise in cases.
The bacterial infection of the lungs spreads very easily and can cause serious problems, especially in babies and young children.
The Black Country Integrated Care Board (ICB) is advising pregnant women between 16 and 32 weeks to contact their GP to get the vaccine so their baby has protection from birth.
The UK Health Security Agency warned earlier this year of a steady decline in uptake of the vaccine in pregnant women and children.
Symptoms of the infection, also known as “100-day cough”, are similar to a cold, with a runny nose and sore throat.
Sally Roberts, chief nursing officer for the ICB, which covers Wolverhampton, Dudley, Walsall and Sandwell, said anyone could catch it, but it was more serious for young children and babies.
“Getting vaccinated while you’re pregnant is highly effective in protecting your baby from developing whooping cough in the first few weeks of their life – ideally from 16 weeks up to 32 weeks of pregnancy,” she said.
“If for any reason you miss having the vaccine, you can still have it up until you go into labour.”
Follow BBC West Midlands on Facebook, X and Instagram. Send your story ideas to: newsonline.westmidlands@bbc.co.uk
Health
Measles cases stabilize in Montreal – CityNews Montreal
The number of measles cases has stabilized, according to the Montreal Public Health.
Since March 25, there have been no contaminations reported within the community.
“Our teams have identified all contact cases of measles,” said media relations advisor Geneviève Paradis. “It’s a laborious task: each measles case produces hundreds of contacts.”
All community transmission cases since February 2024 have been caused by returning travelers who were either unvaccinated or partially vaccinated.
Currently, there are 18 measles cases in Montreal – with 46 total in Quebec. This according to the April 18 figures from the provincial government.
“With the summer vacations approaching, if you’re travelling, it is essential to check if you are protected against measles,” explained Paradis.
According to Montreal Public Health, a person needs to have received two doses after the age of 12 months to be immunized against the virus.
They’ve launched a vaccination campaign throughout the region, and currently, 11,341 people have been vaccinated against measles in Montreal between March 19 and April 15.
Vaccination is also being provided in schools and at local service points.
“The vaccination operation is under the responsibility of the five CIUSSS of the territory,” concluded Paradis.
Health
Risk of bird flu spreading to humans is ‘enormous concern’, says WHO – The Guardian


The World Health Organization has raised concerns about the spread of H5N1 bird flu, which has an “extraordinarily high” mortality rate in humans.
An outbreak that began in 2020 has led to the deaths or killing of tens of millions of poultry. Most recently, the spread of the virus within several mammal species, including in domestic cattle in the US, has increased the risk of spillover to humans, the WHO said.
“This remains I think an enormous concern,” the UN health agency’s chief scientist, Jeremy Farrar, told reporters in Geneva.
Cows and goats joined the list of species affected last month – a surprising development for experts because they were not thought susceptible to this type of influenza. US authorities reported this month that a person in Texas was recovering from bird flu after being exposed to dairy cattle, with 16 herds across six states infected apparently after exposure to wild birds.
The A(H5N1) variant has become “a global zoonotic animal pandemic”, Farrar said.
“The great concern of course is that in … infecting ducks and chickens and then increasingly mammals, that virus now evolves and develops the ability to infect humans and then critically the ability to go from human to human,” he added.
So far, there is no evidence that H5N1 is spreading between humans. But in the hundreds of cases where humans have been infected through contact with animals over the past 20 years, “the mortality rate is extraordinarily high”, Farrar said, because humans have no natural immunity to the virus.
From 2003 to 2024, 889 cases and 463 deaths caused by H5N1 have been reported worldwide from 23 countries, according to the WHO, putting the case fatality rate at 52%.
The recent US case of human infection after contact with an infected mammal highlights the increased risk. When “you come into the mammalian population, then you’re getting closer to humans”, Farrar said, warning that “this virus is just looking for new, novel hosts”.
Farrar called for increased monitoring, saying it was “very important understanding how many human infections are happening … because that’s where adaptation [of the virus] will happen”.
“It’s a tragic thing to say, but if I get infected with H5N1 and I die, that’s the end of it,” he said. “If I go around the community and I spread it to somebody else then you start the cycle.”
He said efforts were under way towards the development of vaccines and therapeutics for H5N1, and stressed the need to ensure that regional and national health authorities around the world had the capacity to diagnose the virus.
This was being done so that “if H5N1 did come across to humans, with human-to-human transmission”, the world would be “in a position to immediately respond”, Farrar said, calling for equitable access to vaccines, therapeutics and diagnostics.
-



 Tech18 hours ago
Tech18 hours agoCytiva Showcases Single-Use Mixing System at INTERPHEX 2024 – BioPharm International
-



 Science24 hours ago
Science24 hours agoNasa confirms metal chunk that crashed into Florida home was space junk
-
News20 hours ago
Tim Hortons says 'technical errors' falsely told people they won $55K boat in Roll Up To Win promo – CBC.ca
-



 Investment24 hours ago
Investment24 hours agoBill Morneau slams Freeland’s budget as a threat to investment, economic growth
-



 Health14 hours ago
Health14 hours agoSupervised consumption sites urgently needed, says study – Sudbury.com
-


 Science23 hours ago
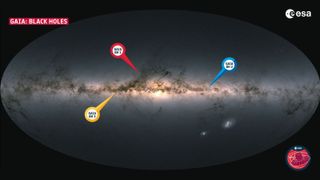
Science23 hours agoRecord breaker! Milky Way's most monstrous stellar-mass black hole is sleeping giant lurking close to Earth (Video) – Space.com
-



 Politics23 hours ago
Politics23 hours agoFlorida's Bob Graham dead at 87: A leader who looked beyond politics, served ordinary folks – Toronto Star
-



 Tech20 hours ago
Tech20 hours agoAaron Sluchinski adds Kyle Doering to lineup for next season – Sportsnet.ca






