Health
Monkeypox vaccine clinic to be held at Windsor Pride event – Windsor Star


Article content
A pop-up clinic offering vaccination against monkeypox has been arranged to take place at a Windsor Pride event this weekend.
Article content
The clinic — provided by the Windsor-Essex County Health Unit in collaboration with Windsor-Essex Pride Fest — will operate during Pride Day festivities at Lanspeary Park (Langlois Avenue at Ottawa Street) on Sunday from 11 a.m. to 4 p.m.
“I think it’s a good thing. We’re being pro-active,” said David Lenz, director of community development with Windsor-Essex Pride Fest.
“There are those who have voiced their concerns (about monkeypox). They want to get the vaccine.”
Dr. Shanker Nesathurai, the region’s acting medical officer of health, said the vaccine clinic is meant as a “pre-exposure prophylaxis” measure against monkeypox and will be the first of its kind in Windsor-Essex.
Asked why a Pride event was chosen for the region’s first distribution of monkeypox vaccine, Nesathurai was frank: “Monkeypox is a significant challenge, and it is disproportionately affecting members of our community where men are having sex with men,” he said.
“We want to distribute the vaccine in the most effective way to minimize the chance of illness among members of our community,” said Nesathurai.
Article content
“We always want to offer public health services in a way that reaches the target community.”
Felicia Lawal, the local health unit’s director of health protection, noted that the provincewide supply of the monkeypox vaccine is limited. The clinic at Lanspeary Park will be able to administer about 100 doses.
“We do have vaccine, but it is a limited quantity,” Lawal said. “It will be on a first-come, first-serve basis.”
Asked if a monkeypox vaccine clinic at a Pride event might fuel a negative perception of the LGBTQ+ community and perpetuate misconceptions about monkeypox, Nesathurai said the health unit always tries to provide services in a way “that is without judgment and stigma.
“But we also recognize … that some populations of individuals are at higher risk for certain diseases at certain times.”
Article content
-
Health unit confirms first Windsor-Essex case of monkeypox
-
WHO declares monkeypox outbreak a global health emergency
-

Toronto organizes monkeypox vaccine clinics targeting ‘high-risk’ communities
“In the context of monkeypox in Ontario, men having sex with men are at the highest risk of contracting monkeypox right now.”
As of Thursday, there were 449 confirmed cases of monkeypox in Ontario — 347 of them in the Toronto area.
Of those Ontario cases, 447 of them — 99.6 per cent — are male.
Nesathurai acknowledged that there are other places in the world where monkeypox has had more widespread transmission. “But we have to contextualize or make judgments based on what we know today. It’s no different than anything else in medicine.”

Lenz said Windsor Pride has been working closely with the health unit for months, and organizers are glad to have secured monkeypox vaccine availability for the festival.
“Not only that, but it’s an opportunity to distribute accurate information about the disease,” Lenz said.
The health unit announced on July 20 that Windsor-Essex had its first confirmed case of monkeypox.
Health
Quebec successfully pushes back against rise in measles cases – CBC.ca
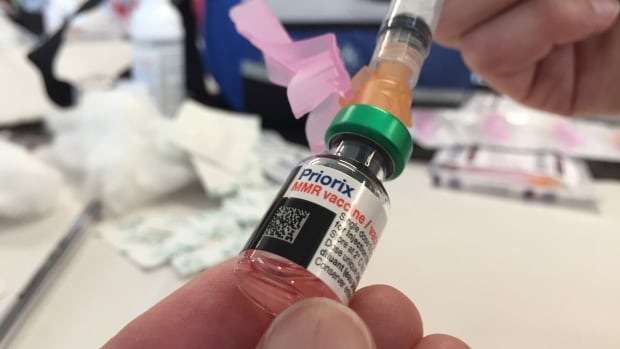
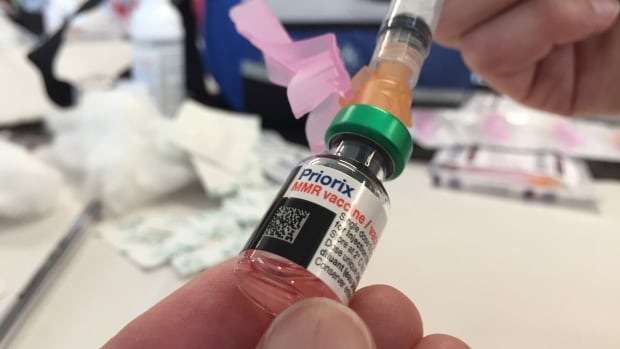
Quebec appears to be winning its battle against the rising tide of measles after 45 cases were confirmed province-wide this year.
“We’ve had no locally transmitted measles cases since March 25, so that’s good news,” said Dr. Paul Le Guerrier, responsible for immunization for Montreal Public Health.
There are 17 patients with measles in Quebec currently, and the most recent case is somebody who was infected while abroad, he said.
But it was no small task to get to this point.
Le Guerrier said once local transmission was detected, news was spread fast among health centres to ensure proper protocols were followed — such as not letting potentially infected people sit in waiting rooms for hours on end.
Then about 90 staffers were put to work, tracking down those who were in contact with positive cases and are not properly vaccinated. They were given post-exposure prophylaxis, which prevents disease, said Le Guerrier.
From there, a vaccination campaign was launched, especially in daycares, schools and neighbourhoods with low inoculation rates. There was an effort to convince parents to get their children vaccinated.
Vaccination in schools boosted
Some schools, mostly in Montreal, had vaccination rates as low as 30 or 40 per cent.
“Vaccination was well accepted and parents responded well,” said Le Guerrier. “Some schools went from very low to as high as 85 to 90 per cent vaccination coverage.”
But it’s not only children who aren’t properly vaccinated. Le Guerrier said people need two doses after age one to be fully inoculated, and he encouraged people to check their status.
There are all kinds of reasons why people aren’t vaccinated, but it’s only about five per cent who are against immunization, he said. So far, some 10,000 people have been vaccinated against measles province-wide during this campaign, Le Guerrier said.
The next step is to continue pushing for further vaccination, but he said, small outbreaks are likely in the future as measles is spreading abroad and travellers are likely to bring it back with them.
Need to improve vaccination rate, expert says
Dr. Donald Vinh, an infectious diseases specialist from the McGill University Health Centre, said it’s not time to rest on our laurels, but this is a good indication that public health is able to take action quickly and that people are willing to listen to health recommendations.
“We are not seeing new cases or at least the new cases are not exceeding the number of cases that we can handle,” said Vinh.
“So these are all reassuring signs, but I don’t think it’s a sign that we need to become complacent.”
Vinh said there are also signs that the public is lagging in vaccine coverage and it’s important to respond to this with improved education and access. Otherwise, microbes capitalize on our weaknesses, he said.
Getting vaccination coverage up to an adequate level is necessary, Vinh said, or more small outbreaks like this will continue to happen.
“And it’s very possible that we may not be able to get one under control if we don’t react quickly enough,” he said.
Health
Pregnant women in the Black Country urged to get whooping cough vaccine – BBC.com


Pregnant women urged to get whooping cough vaccine
Pregnant women in the Black Country are being urged to get vaccinated against whooping cough after a rise in cases.
The bacterial infection of the lungs spreads very easily and can cause serious problems, especially in babies and young children.
The Black Country Integrated Care Board (ICB) is advising pregnant women between 16 and 32 weeks to contact their GP to get the vaccine so their baby has protection from birth.
The UK Health Security Agency warned earlier this year of a steady decline in uptake of the vaccine in pregnant women and children.
Symptoms of the infection, also known as “100-day cough”, are similar to a cold, with a runny nose and sore throat.
Sally Roberts, chief nursing officer for the ICB, which covers Wolverhampton, Dudley, Walsall and Sandwell, said anyone could catch it, but it was more serious for young children and babies.
“Getting vaccinated while you’re pregnant is highly effective in protecting your baby from developing whooping cough in the first few weeks of their life – ideally from 16 weeks up to 32 weeks of pregnancy,” she said.
“If for any reason you miss having the vaccine, you can still have it up until you go into labour.”
Follow BBC West Midlands on Facebook, X and Instagram. Send your story ideas to: newsonline.westmidlands@bbc.co.uk
Health
Measles cases stabilize in Montreal – CityNews Montreal
The number of measles cases has stabilized, according to the Montreal Public Health.
Since March 25, there have been no contaminations reported within the community.
“Our teams have identified all contact cases of measles,” said media relations advisor Geneviève Paradis. “It’s a laborious task: each measles case produces hundreds of contacts.”
All community transmission cases since February 2024 have been caused by returning travelers who were either unvaccinated or partially vaccinated.
Currently, there are 18 measles cases in Montreal – with 46 total in Quebec. This according to the April 18 figures from the provincial government.
“With the summer vacations approaching, if you’re travelling, it is essential to check if you are protected against measles,” explained Paradis.
According to Montreal Public Health, a person needs to have received two doses after the age of 12 months to be immunized against the virus.
They’ve launched a vaccination campaign throughout the region, and currently, 11,341 people have been vaccinated against measles in Montreal between March 19 and April 15.
Vaccination is also being provided in schools and at local service points.
“The vaccination operation is under the responsibility of the five CIUSSS of the territory,” concluded Paradis.
-



 Tech21 hours ago
Tech21 hours agoCytiva Showcases Single-Use Mixing System at INTERPHEX 2024 – BioPharm International
-



 Health17 hours ago
Health17 hours agoSupervised consumption sites urgently needed, says study – Sudbury.com
-
News23 hours ago
Tim Hortons says 'technical errors' falsely told people they won $55K boat in Roll Up To Win promo – CBC.ca
-



 Tech23 hours ago
Tech23 hours agoAaron Sluchinski adds Kyle Doering to lineup for next season – Sportsnet.ca
-



 Politics24 hours ago
Politics24 hours agoTrump faces political risks as trial begins – NBC News
-
Tech22 hours ago
Nintendo Indie World Showcase April 2024 – Every Announcement, Game Reveal & Trailer – Nintendo Life
-
News16 hours ago
2024 federal budget's key takeaways: Housing and carbon rebates, students and sin taxes – CBC News
-
Business23 hours ago
GTA gas prices to jump 14 cents a litre – Toronto Sun







