Health
More Canadians could face late-stage cancer tied to diagnosis delays during COVID pandemic – CBC News

It all started with a stomach bug.
That’s what Cheryl-Anne Labrador-Summers thought, anyway. It was October 2020, not long after she’d moved to the tranquil lakeside Ontario community of Georgina, and instead of relaxing with her family like she’d planned, the mother of three was struggling to figure out why she kept experiencing strange, unexplained stomach cramps.
Labrador-Summers tried to visit her family physician, but the office was shuttered because of the COVID-19 pandemic. So she searched for another clinic — only to be offered a phone appointment rather than an in-person assessment. She wound up being told that her grumbling digestive system was likely caused by a mild gastrointestinal illness.
By January, the 58-year-old had a distended stomach, looking — in her own words — “about nine months pregnant.” Again, she reached out to a physician, went for some tests, then headed to the nearest emergency department.
After finally seeing a doctor face to face for the first time in months, she learned the real cause of her discomfort: an intestinal blockage caused by cancer.
“It ended up being a nine-centimetre tumour, and it had completely blocked off my lower bowel,” she said.
An emergency surgery left Labrador-Summers with 55 staples along her torso and a months-long recovery before she could begin oral chemotherapy. Her question now is unanswerable but painful to consider: Could that ordeal have been prevented, or at least minimized, by an earlier diagnosis?
“Had I maybe been able to see the doctors earlier, I would not be in Stage 3,” she said. “I might have been a Stage 2.”
951,000 fewer cancer screenings in Ontario
More Canadians could experience late-stage cancer diagnoses in the years ahead, medical experts warn, forecasting a looming crisis tied to the ongoing COVID-19 pandemic.
“We expect to see more advanced stages of presentation over the next couple of years, as well as impacts on cancer treatments,” said oncologist Dr. Timothy Hanna, a clinician scientist at the Cancer Research Institute at Queen’s University in Kingston, Ont.
“We know that time is of the essence for people with cancer. And when people are waiting for a diagnosis or for treatment, this has been associated with increased risks of advanced stage and worse survival.”
One review of Ontario’s breast, lung, colon, and cervical cancer screening programs showed that in 2020 there were 41 per cent — or more than 951,000 — fewer screening tests conducted compared with the year before.
Screening volumes rebounded after May 2020, but were still 20 per cent lower compared to pre-pandemic levels.
WATCH | Late-stage cancer being diagnosed in Canadian ERs:
Hospital emergency rooms are seeing a wave of patients being diagnosed with late-stage cancer after the COVID-19 pandemic forced many doctors’ offices to close or pivot to virtual appointments, leading to fewer cancer screenings.
That drop in screenings translates into fewer invasive cancer diagnoses, including roughly 1,400 to 1,500 fewer breast cancers, wrote Dr. Anna N. Wilkinson, an assistant professor in the department of family medicine at the University of Ottawa, in a May commentary piece for the journal Canadian Family Physician.
“The impact of COVID-19 on cancer is far-reaching: screening backlogs, delayed workup of symptomatic patients and abnormal screening results, and delays in cancer treatment and research, all exacerbated by patient apprehension to be seen in person,” she wrote.
“It is clear that there is not only a lost cohort of screened patients but also a subset of missed cancer diagnoses due to delays in patient presentation and assessment,” leading to those cancers being diagnosed at a more advanced stage.
Tough accessing care in a ‘timely way’
The slowdown in colonoscopies may already be leading to more serious cases of colorectal cancer in Ontario, for instance, suggests a paper published in the Journal of the Canadian Association of Gastroenterology.
“Patients who were treated after the COVID-19 pandemic began were significantly more likely to present emergently to hospital. This means that they were more likely to present with bowel perforation, or severe bowel obstruction, requiring immediate life-saving surgery,” said the study’s lead author, Dr. Catherine Forse, in a call with CBC News.
“In addition, we found that patients were more likely to have large tumours.”


In some cases — like Labrador-Summers’s situation — Canadians learned alarming news about their health in hospital emergency departments after struggling to receive in-patient care through other avenues.
Shuttered family physician offices, a shift to telemedicine, and some patients’ fears surrounding COVID-19 may all have played a role.
“It became harder for patients to access care and to access it in a timely way,” Hanna said.
“At the same time, there were real risks — and there are real risks for leaving home to go anywhere, particularly to go to an outpatient clinic or a hospital in order to get checked out.”
Dr. Lisa Salamon, an emergency physician with the Scarborough Health Network in Toronto, said she’s now diagnosing more patients with serious cancers, including several just in the last few months.
“So previously, it may have been localized or something small, but now we’re actually seeing metastatic cancer that we’re diagnosing,” she explained.
Lessons for future pandemics
Health policy expert Laura Greer is dealing with Stage four, metastatic breast cancer herself after waiting more than five months for a routine mammogram she was initially due for in the spring of 2021 — a precautionary measure given that her mother had breast cancer as well.
Unlike an early-stage diagnosis, Greer’s cancer is only treatable, not curable.
“It was an example of what happens when you don’t have the regular screening, or those wellness visits,” said the Toronto resident and mother of two.
“I most likely would have had earlier-stage cancer if it had been sooner.”


Pausing access to care and screenings for other health conditions can have dire impacts on patients, according to Greer, offering lessons for how policy-makers tackle future pandemics.
“We need to make sure that we’ve got enough capacity in our health system to be able to flex, and that’s what we really didn’t have going into this,” she said.
For Labrador-Summers, it’s hard to forget the moment her life changed while she was alone in an emergency department, learning a terrifying diagnosis from a physician she’d just met. Her mind raced with questions about the future and concerns for her family.


“My older son had just told us they were expecting a child, and I just wanted to be there for them. And I didn’t know what next steps were. And we had lost my mom to cancer a few years back — to us, cancer was always terminal,” she recalled.
“So again, I’m alone, trying to process all of this.”
A screening following Labrador-Summers’ surgery and chemotherapy treatment wound up finding more cancer.
“It’s now life-threatening,” she said.
Health
Cancer Awareness Month – Métis Nation of Alberta


Cancer Awareness Month
Posted on: Apr 18, 2024
April is Cancer Awareness Month
As we recognize Cancer Awareness Month, we stand together to raise awareness, support those affected, advocate for prevention, early detection, and continued research towards a cure. Cancer is the leading cause of death for Métis women and the second leading cause of death for Métis men. The Otipemisiwak Métis Government of the Métis Nation Within Alberta is working hard to ensure that available supports for Métis Citizens battling cancer are culturally appropriate, comprehensive, and accessible by Métis Albertans at all stages of their cancer journey.
Receiving a cancer diagnosis, whether for yourself or a loved one, can feel overwhelming, leaving you unsure of where to turn for support. In June, our government will be launching the Cancer Supports and Navigation Program which will further support Métis Albertans and their families experiencing cancer by connecting them to OMG-specific cancer resources, external resources, and providing navigation support through the health care system. This program will also include Métis-specific peer support groups for those affected by cancer.
With funding from the Canadian Partnership Against Cancer (CPAC) we have also developed the Métis Cancer Care Course to ensure that Métis Albertans have access to culturally safe and appropriate cancer services. This course is available to cancer care professionals across the country and provides an overview of who Métis people are, our culture, our approaches to health and wellbeing, our experiences with cancer care, and our cancer journey.
Together, we can make a difference in the fight against cancer and ensure equitable access to culturally safe and appropriate care for all Métis Albertans. Please click on the links below to learn more about the supports available for Métis Albertans, including our Compassionate Care: Cancer Transportation program.
I wish you all good health and happiness!
Bobbi Paul-Alook
Secretary of Health & Seniors
Health
Type 2 diabetes is not one-size-fits-all: Subtypes affect complications and treatment options – The Conversation


You may have heard of Ozempic, the “miracle drug” for weight loss, but did you know that it was actually designed as a new treatment to manage diabetes? In Canada, diabetes affects approximately 10 per cent of the general population. Of those cases, 90 per cent have Type 2 diabetes.
This metabolic disorder is characterized by persistent high blood sugar levels, which can be accompanied by secondary health challenges, including a higher risk of stroke and kidney disease.
Locks and keys
In Type 2 diabetes, the body struggles to maintain blood sugar levels in an acceptable range. Every cell in the body needs sugar as an energy source, but too much sugar can be toxic to cells. This equilibrium needs to be tightly controlled and is regulated by a lock and key system.
In the body’s attempt to manage blood sugar levels and ensure that cells receive the right amount of energy, the pancreatic hormone, insulin, functions like a key. Cells cover themselves with locks that respond perfectly to insulin keys to facilitate the entry of sugar into cells.
Unfortunately, this lock and key system doesn’t always perform as expected. The body can encounter difficulties producing an adequate number of insulin keys, and/or the locks can become stubborn and unresponsive to insulin.
All forms of diabetes share the challenge of high blood sugar levels; however, diabetes is not a singular condition; it exists as a spectrum. Although diabetes is broadly categorized into two main types, Type 1 and Type 2, each presents a diversity of subtypes, especially Type 2 diabetes.
These subtypes carry their own characteristics and risks, and do not respond uniformly to the same treatments.
To better serve people living with Type 2 diabetes, and to move away from a “one size fits all” approach, it is beneficial to understand which subtype of Type 2 diabetes a person lives with. When someone needs a blood transfusion, the medical team needs to know the patient’s blood type. It should be the same for diabetes so a tailored and effective game plan can be implemented.
This article explores four unique subtypes of Type 2 diabetes, shedding light on their causes, complications and some of their specific treatment avenues.
Severe insulin-deficient diabetes: We’re missing keys!
(Lili Grieco-St-Pierre, Jennifer Bruin/Created with BioRender.com)
Insulin is produced by beta cells, which are found in the pancreas. In the severe insulin-deficient diabetes (SIDD) subtype, the key factories — the beta cells — are on strike. Ultimately, there are fewer keys in the body to unlock the cells and allow entry of sugar from the blood.
SIDD primarily affects younger, leaner individuals, and unfortunately, increases the risk of eye disease and blindness, among other complications. Why the beta cells go on strike remains largely unknown, but since there is an insulin deficiency, treatment often involves insulin injections.
Severe insulin-resistant diabetes: But it’s always locked!
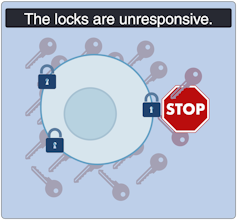
(Lili Grieco-St-Pierre, Jennifer Bruin/Created with BioRender.com)
In the severe insulin-resistant diabetes (SIRD) subtype, the locks are overstimulated and start ignoring the keys. As a result, the beta cells produce even more keys to compensate. This can be measured as high levels of insulin in the blood, also known as hyperinsulinemia.
This resistance to insulin is particularly prominent in individuals with higher body weight. Patients with SIRD have an increased risk of complications such as fatty liver disease. There are many treatment avenues for these patients but no consensus about the optimal approach; patients often require high doses of insulin.
Mild obesity-related diabetes: The locks are sticky!

(Lili Grieco-St-Pierre, Jennifer Bruin/Created with BioRender.com)
Mild obesity-related (MOD) diabetes represents a nuanced aspect of Type 2 diabetes, often observed in individuals with higher body weight. Unlike more severe subtypes, MOD is characterized by a more measured response to insulin. The locks are “sticky,” so it is challenging for the key to click in place and open the lock. While MOD is connected to body weight, the comparatively less severe nature of MOD distinguishes it from other diabetes subtypes.
To minimize complications, treatment should include maintaining a healthy diet, managing body weight, and incorporating as much aerobic exercise as possible. This is where drugs like Ozempic can be prescribed to control the evolution of the disease, in part by managing body weight.
Mild age-related diabetes: I’m tired of controlling blood sugar!
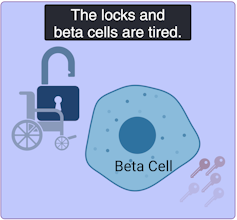
(Lili Grieco-St-Pierre, Jennifer Bruin/Created with BioRender.com)
Mild age-related diabetes (MARD) happens more often in older people and typically starts later in life. With time, the key factory is not as productive, and the locks become stubborn. People with MARD find it tricky to manage their blood sugar, but it usually doesn’t lead to severe complications.
Among the different subtypes of diabetes, MARD is the most common.
Unique locks, varied keys
While efforts have been made to classify diabetes subtypes, new subtypes are still being identified, making proper clinical assessment and treatment plans challenging.
In Canada, unique cases of Type 2 diabetes were identified in Indigenous children from Northern Manitoba and Northwestern Ontario by Dr. Heather Dean and colleagues in the 1980s and 90s. Despite initial skepticism from the scientific community, which typically associated Type 2 diabetes with adults rather than children, clinical teams persisted in identifying this as a distinct subtype of Type 2 diabetes, called childhood-onset Type 2 diabetes.
Read more:
Indigenous community research partnerships can help address health inequities
Childhood-onset Type 2 diabetes is on the rise across Canada, but disproportionately affects Indigenous youth. It is undoubtedly linked to the intergenerational trauma associated with colonization in these communities. While many factors are likely involved, recent studies have discovered that exposure of a fetus to Type 2 diabetes during pregnancy increases the risk that the baby will develop diabetes later in life.
Acknowledging this distinct subtype of Type 2 diabetes in First Nations communities has led to the implementation of a community-based health action plan aimed at addressing the unique challenges faced by Indigenous Peoples. It is hoped that partnered research between communities and researchers will continue to help us understand childhood-onset Type 2 diabetes and how to effectively prevent and treat it.
A mosaic of conditions
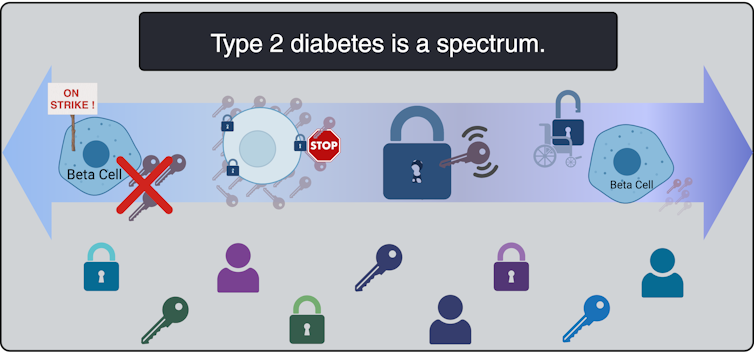
(Lili Grieco-St-Pierre, Jennifer Bruin/Created with BioRender.com)
Type 2 diabetes is not uniform; it’s a mosaic of conditions, each with its own characteristics. Since diabetes presents so uniquely in every patient, even categorizing into subtypes does not guarantee how the disease will evolve. However, understanding these subtypes is a good starting point to help doctors create personalized plans for people living with the condition.
While Indigenous communities, lower-income households and individuals living with obesity already face a higher risk of developing Type 2 diabetes than the general population, tailored solutions may offer hope for better management. This emphasizes the urgent need for more precise assessments of diabetes subtypes to help customize therapeutic strategies and management strategies. This will improve care for all patients, including those from vulnerable and understudied populations.
Health
Quebec successfully pushes back against rise in measles cases – CBC.ca
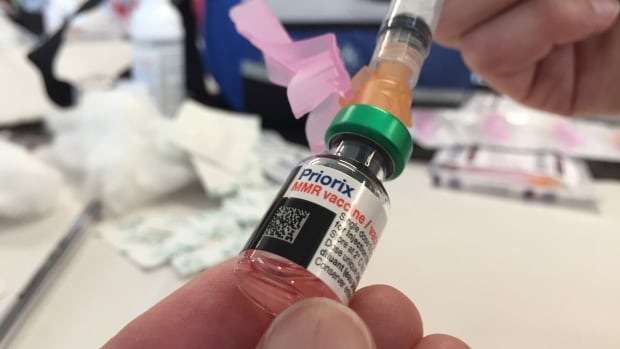
Quebec appears to be winning its battle against the rising tide of measles after 45 cases were confirmed province-wide this year.
“We’ve had no locally transmitted measles cases since March 25, so that’s good news,” said Dr. Paul Le Guerrier, responsible for immunization for Montreal Public Health.
There are 17 patients with measles in Quebec currently, and the most recent case is somebody who was infected while abroad, he said.
But it was no small task to get to this point.
Le Guerrier said once local transmission was detected, news was spread fast among health centres to ensure proper protocols were followed — such as not letting potentially infected people sit in waiting rooms for hours on end.
Then about 90 staffers were put to work, tracking down those who were in contact with positive cases and are not properly vaccinated. They were given post-exposure prophylaxis, which prevents disease, said Le Guerrier.
From there, a vaccination campaign was launched, especially in daycares, schools and neighbourhoods with low inoculation rates. There was an effort to convince parents to get their children vaccinated.
Vaccination in schools boosted
Some schools, mostly in Montreal, had vaccination rates as low as 30 or 40 per cent.
“Vaccination was well accepted and parents responded well,” said Le Guerrier. “Some schools went from very low to as high as 85 to 90 per cent vaccination coverage.”
But it’s not only children who aren’t properly vaccinated. Le Guerrier said people need two doses after age one to be fully inoculated, and he encouraged people to check their status.
There are all kinds of reasons why people aren’t vaccinated, but it’s only about five per cent who are against immunization, he said. So far, some 10,000 people have been vaccinated against measles province-wide during this campaign, Le Guerrier said.
The next step is to continue pushing for further vaccination, but he said, small outbreaks are likely in the future as measles is spreading abroad and travellers are likely to bring it back with them.
Need to improve vaccination rate, expert says
Dr. Donald Vinh, an infectious diseases specialist from the McGill University Health Centre, said it’s not time to rest on our laurels, but this is a good indication that public health is able to take action quickly and that people are willing to listen to health recommendations.
“We are not seeing new cases or at least the new cases are not exceeding the number of cases that we can handle,” said Vinh.
“So these are all reassuring signs, but I don’t think it’s a sign that we need to become complacent.”
Vinh said there are also signs that the public is lagging in vaccine coverage and it’s important to respond to this with improved education and access. Otherwise, microbes capitalize on our weaknesses, he said.
Getting vaccination coverage up to an adequate level is necessary, Vinh said, or more small outbreaks like this will continue to happen.
“And it’s very possible that we may not be able to get one under control if we don’t react quickly enough,” he said.
-



 Science8 hours ago
Science8 hours agoJeremy Hansen – The Canadian Encyclopedia
-



 Tech7 hours ago
Tech7 hours agoSave $700 Off This 4K Projector at Amazon While You Still Can – CNET
-



 Investment8 hours ago
Investment8 hours agoUK Mulls New Curbs on Outbound Investment Over Security Risks – BNN Bloomberg
-



 Tech6 hours ago
Tech6 hours ago'Kingdom Come: Deliverance II' Revealed In Epic New Trailer And It Looks Incredible – Forbes
-



 Sports6 hours ago
Sports6 hours agoAuston Matthews denied 70th goal as depleted Leafs lose last regular-season game – Toronto Sun
-



 Health22 hours ago
Health22 hours agoSupervised consumption sites urgently needed, says study – Sudbury.com
-
Real eState7 hours ago
Sick of Your Blue State? These Real Estate Agents Have Just the Place for You. – The New York Times
-
News21 hours ago
Canada's 2024 budget announces 'halal mortgages'. Here's what to know – National Post






