Health
Neurological problems no higher after vaccination; depression, anxiety risk tied to COVID severity
|
|
The following is a summary of some recent studies on COVID-19. They include research that warrants further study to corroborate the findings and that has yet to be certified by peer review.
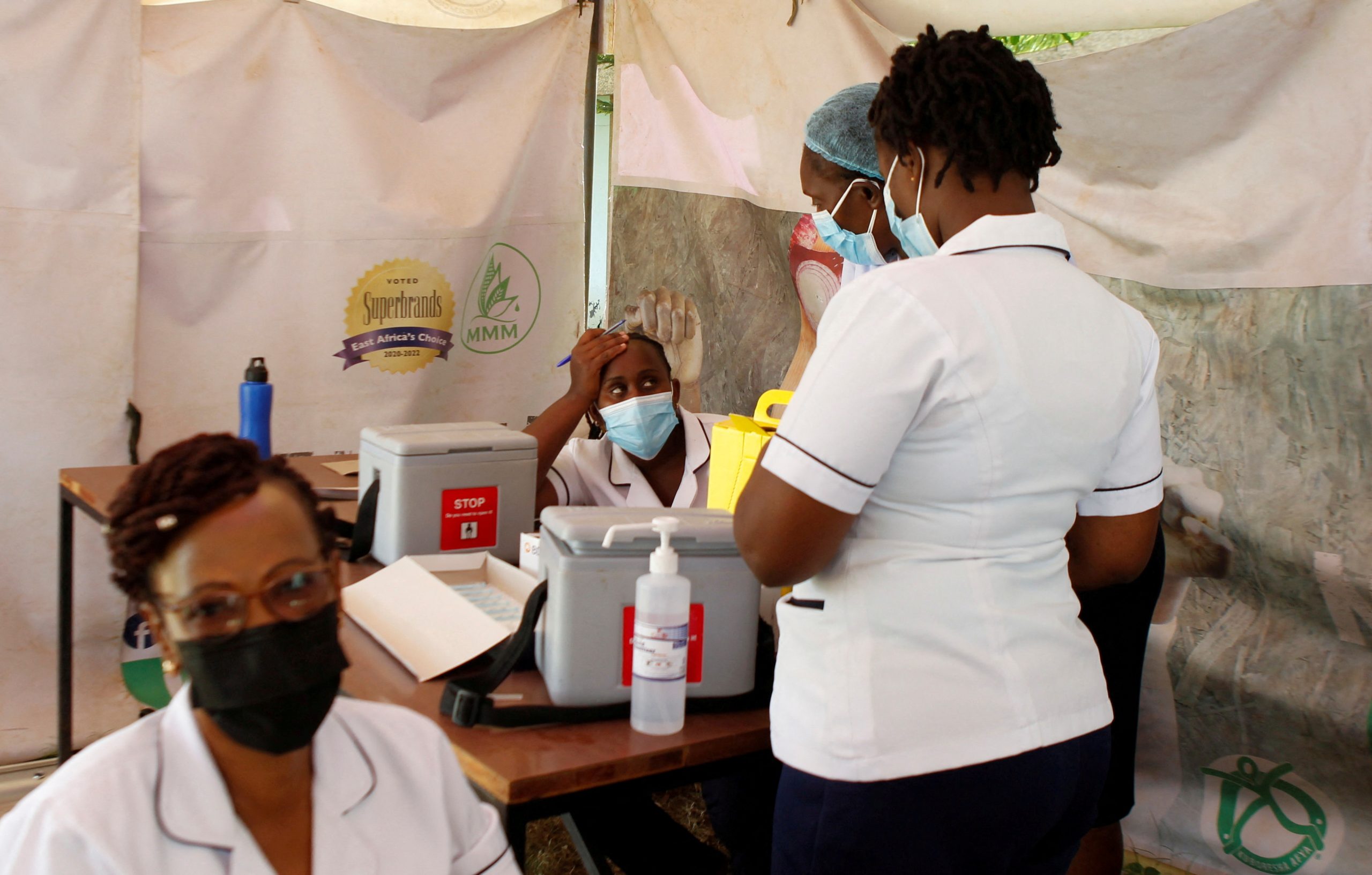
Neurological risks not higher after COVID-19 vaccines
COVID-19 vaccination did not increase risks for rare neurological conditions among more than 8 million people who had received at least one dose of a vaccine from AstraZeneca, Pfizer/BioNTech, Moderna or Johnson & Johnson, according to researchers.
Their study also included 735,870 unvaccinated individuals who had tested positive for the coronavirus, as well as older data on an additional 14.3 million people from the general population for a baseline estimate of rates of the neurological conditions before the pandemic. Researchers looked for four neurological disorders involving the immune system. Three of them – Bell’s palsy (facial weakness), encephalomyelitis (inflammation of the brain and spinal cord), and Guillain-Barré syndrome (a nerve condition) – were no more common in the vaccine recipients than in the general population, the researchers reported on Wednesday in The BMJ https://www.bmj.com/content/376/bmj-2021-068373. The fourth – transverse myelitis (inflammation of the spinal cord) – occurred too rarely for analysis (fewer than 5 cases in 8.3 million vaccinated people). The researchers did see increased rates of Bell’s palsy, encephalomyelitis and Guillain-Barré syndrome in COVID-19 survivors, however.
More research is needed to look for longer term adverse events of vaccination and SARS-CoV-2 infection and to study the effects of vaccines on different age groups, the researchers said. But it appears that COVID-19 vaccines are “a highly unlikely reason” for most neurological problems, they concluded.
Risk of depression, anxiety tied to COVID-19 severity
People who have been bedridden for seven days or more with COVID-19 are at increased risk of anxiety and depression, an international study found.
Researchers analyzed data from Denmark, Estonia, Iceland, Norway, Sweden and the UK collected between March 2020 and August 2021 on more than 247,000 people, including 9,979 who were diagnosed with COVID-19. Those who had COVID and were bedridden for at least a week had a 61% higher risk for symptoms of depression and a 43% higher risk for anxiety, for up to 16 months after their diagnosis compared to those who were never infected.
By contrast, patients who had COVID-19 but were never bedridden actually had significantly lower rates of depression than people who had never contracted the virus, researchers found. “This group may experience a relief after recovery from the relatively benign infection and are able to return to somewhat normal lives as compared to those not yet diagnosed with COVID-19, perhaps still fearing infection and therefore still limiting social contact,” said Dr. Anna Valdimarsdottir of the University of Iceland, whose team reported the findings in The Lancet Public Health https://www.thelancet.com/journals/lanpub/article/PIIS2468-2667(22)00042-1/fulltext. The results should alert clinicians to the possibility of long-term mental health symptoms in their patients who suffered severe acute illness from the virus, she added.
Pfizer/BioNTech vaccine safe after heart inflammation
People who have had an inflamed heart muscle in the past can safety receive the COVID-19 mRNA vaccine from Pfizer and BioNTech without causing the problem to recur, a small study suggests.
The inflammatory condition, called myocarditis, is a common complication of COVID and other viral infections and has been a rare side effect associated with some COVID-19 vaccines, primarily in young males. But among 55 patients who had recovered from myocarditis within the past five years and who later received a COVID-19 mRNA vaccine, no one suffered a repeat episode of myocarditis, researchers reported on Friday at the European heart meeting ESC Acute CardioVascular Care 2022 https://www.escardio.org/Congresses-&-Events/Acute-Cardiovascular-Care. Of the 55 subjects, 43 had received both doses of the vaccine and 12 just the first dose. Nearly all had received the Pfizer/BioNTech vaccine, so the findings may not apply to other shots, the researchers said.
Still, the results “provide reassuring data that may encourage patients with a history of myocarditis to get vaccinated against SARS-CoV-2,” study author Dr. Iyad Abou Saleh of Hospices Civils de Lyon, France, said in a statement.
Click for a Reuters graphic https://tmsnrt.rs/3c7R3Bl on vaccines in development.
(Reporting by Nancy Lapid and Linda Carroll; Editing by Bill Berkrot)
Health
April 22nd to 30th is Immunization Awareness Week – Oldies 107.7


<!–
isIE8 = true;
Date.now = Date.now || function() return +new Date; ;
Health
AHS confirms case of measles in Edmonton – CityNews Edmonton


Alberta Health Services (AHS) has confirmed a case of measles in Edmonton, and is advising the public that the individual was out in public while infectious.
Measles is an extremely contagious disease that is spread easily through the air, and can only be prevented through immunization.
AHS says individuals who were in the following locations during the specified dates and times, may have been exposed to measles.
- April 16
- Edmonton International Airport, international arrivals and baggage claim area — between 3:20 p.m. and 6 p.m.
- April 20
- Stollery Children’s Hospital Emergency Department — between 5 a.m. to 3 p.m.
- April 22
- 66th Medical Clinic (13635 66 St NW Edmonton) — between 12:15 p.m. to 3:30 p.m.
- Pharmacy 66 (13637 66 St NW Edmonton) — between 12:15 p.m. to 3:30 p.m.
- April 23
- Stollery Children’s Hospital Emergency Department — between 4:40 a.m. to 9:33 a.m.
AHS says anyone who attended those locations during those times is at risk of developing measles if they’ve not had two documented doses of measles-containing vaccine.
Those who have not had two doses, who are pregnant, under one year of age, or have a weakened immune system are at greatest risk of getting measles and should contact Health Link at 1-877-720-0707.
Symptoms
Symptoms of measles include a fever of 38.3° C or higher, cough, runny nose, and/or red eyes, a red blotchy rash that appears three to seven days after fever starts, beginning behind the ears and on the face and spreading down the body and then to the arms and legs.
If you have any of these symptoms stay home and call Health Link.
In Alberta, measles vaccine is offered, free of charge, through Alberta’s publicly funded immunization program. Children in Alberta typically receive their first dose of measles vaccine at 12 months of age, and their second dose at 18 months of age.
Health
U.S. tightens rules for dairy cows a day after bird flu virus fragments found in pasteurized milk samples – Toronto Star


/* OOVVUU Targeting */
const path = ‘/news/canada’;
const siteName = ‘thestar.com’;
let domain = ‘thestar.com’;
if (siteName === ‘thestar.com’)
domain = ‘thestar.com’;
else if (siteName === ‘niagarafallsreview.ca’)
domain = ‘niagara_falls_review’;
else if (siteName === ‘stcatharinesstandard.ca’)
domain = ‘st_catharines_standard’;
else if (siteName === ‘thepeterboroughexaminer.com’)
domain = ‘the_peterborough_examiner’;
else if (siteName === ‘therecord.com’)
domain = ‘the_record’;
else if (siteName === ‘thespec.com’)
domain = ‘the_spec’;
else if (siteName === ‘wellandtribune.ca’)
domain = ‘welland_tribune’;
else if (siteName === ‘bramptonguardian.com’)
domain = ‘brampton_guardian’;
else if (siteName === ‘caledonenterprise.com’)
domain = ‘caledon_enterprise’;
else if (siteName === ‘cambridgetimes.ca’)
domain = ‘cambridge_times’;
else if (siteName === ‘durhamregion.com’)
domain = ‘durham_region’;
else if (siteName === ‘guelphmercury.com’)
domain = ‘guelph_mercury’;
else if (siteName === ‘insidehalton.com’)
domain = ‘inside_halton’;
else if (siteName === ‘insideottawavalley.com’)
domain = ‘inside_ottawa_valley’;
else if (siteName === ‘mississauga.com’)
domain = ‘mississauga’;
else if (siteName === ‘muskokaregion.com’)
domain = ‘muskoka_region’;
else if (siteName === ‘newhamburgindependent.ca’)
domain = ‘new_hamburg_independent’;
else if (siteName === ‘niagarathisweek.com’)
domain = ‘niagara_this_week’;
else if (siteName === ‘northbaynipissing.com’)
domain = ‘north_bay_nipissing’;
else if (siteName === ‘northumberlandnews.com’)
domain = ‘northumberland_news’;
else if (siteName === ‘orangeville.com’)
domain = ‘orangeville’;
else if (siteName === ‘ourwindsor.ca’)
domain = ‘our_windsor’;
else if (siteName === ‘parrysound.com’)
domain = ‘parrysound’;
else if (siteName === ‘simcoe.com’)
domain = ‘simcoe’;
else if (siteName === ‘theifp.ca’)
domain = ‘the_ifp’;
else if (siteName === ‘waterloochronicle.ca’)
domain = ‘waterloo_chronicle’;
else if (siteName === ‘yorkregion.com’)
domain = ‘york_region’;
let sectionTag = ”;
try
if (domain === ‘thestar.com’ && path.indexOf(‘wires/’) = 0)
sectionTag = ‘/business’;
else if (path.indexOf(‘/autos’) >= 0)
sectionTag = ‘/autos’;
else if (path.indexOf(‘/entertainment’) >= 0)
sectionTag = ‘/entertainment’;
else if (path.indexOf(‘/life’) >= 0)
sectionTag = ‘/life’;
else if (path.indexOf(‘/news’) >= 0)
sectionTag = ‘/news’;
else if (path.indexOf(‘/politics’) >= 0)
sectionTag = ‘/politics’;
else if (path.indexOf(‘/sports’) >= 0)
sectionTag = ‘/sports’;
else if (path.indexOf(‘/opinion’) >= 0)
sectionTag = ‘/opinion’;
} catch (ex)
const descriptionUrl = ‘window.location.href’;
const vid = ‘mediainfo.reference_id’;
const cmsId = ‘2665777’;
let url = `https://pubads.g.doubleclick.net/gampad/ads?iu=/58580620/$domain/video/oovvuu$sectionTag&description_url=$descriptionUrl&vid=$vid&cmsid=$cmsId&tfcd=0&npa=0&sz=640×480&ad_rule=0&gdfp_req=1&output=vast&unviewed_position_start=1&env=vp&impl=s&correlator=`;
url = url.split(‘ ‘).join(”);
window.oovvuuReplacementAdServerURL = url;
Infected cows were already prohibited from being transported out of state, but that was based on the physical characteristics of the milk, which looks curdled when a cow is infected, or a cow has decreased lactation or low appetite, both symptoms of infection.
function buildUserSwitchAccountsForm()
var form = document.getElementById(‘user-local-logout-form-switch-accounts’);
if (form) return;
// build form with javascript since having a form element here breaks the payment modal.
var switchForm = document.createElement(‘form’);
switchForm.setAttribute(‘id’,’user-local-logout-form-switch-accounts’);
switchForm.setAttribute(‘method’,’post’);
switchForm.setAttribute(‘action’,’https://www.thestar.com/tncms/auth/logout/?return=https://www.thestar.com/users/login/?referer_url=https%3A%2F%2Fwww.thestar.com%2Fnews%2Fcanada%2Fu-s-tightens-rules-for-dairy-cows-a-day-after-bird-flu-virus-fragments-found%2Farticle_985b0bac-0252-11ef-abc6-eb884d6a1f0c.html’);
switchForm.setAttribute(‘style’,’display:none;’);
var refUrl = document.createElement(‘input’); //input element, text
refUrl.setAttribute(‘type’,’hidden’);
refUrl.setAttribute(‘name’,’referer_url’);
refUrl.setAttribute(‘value’,’https://www.thestar.com/news/canada/u-s-tightens-rules-for-dairy-cows-a-day-after-bird-flu-virus-fragments-found/article_985b0bac-0252-11ef-abc6-eb884d6a1f0c.html’);
var submit = document.createElement(‘input’);
submit.setAttribute(‘type’,’submit’);
submit.setAttribute(‘name’,’logout’);
submit.setAttribute(‘value’,’Logout’);
switchForm.appendChild(refUrl);
switchForm.appendChild(submit);
document.getElementsByTagName(‘body’)[0].appendChild(switchForm);
function handleUserSwitchAccounts()
window.sessionStorage.removeItem(‘bd-viafoura-oidc’); // clear viafoura JWT token
// logout user before sending them to login page via return url
document.getElementById(‘user-local-logout-form-switch-accounts’).submit();
return false;
buildUserSwitchAccountsForm();
console.log(‘=====> bRemoveLastParagraph: ‘,0);
-
News23 hours ago
Amid concerns over ‘collateral damage’ Trudeau, Freeland defend capital gains tax change
-
Art20 hours ago
The unmissable events taking place during London’s Digital Art Week
-
News24 hours ago
U.K. tabloids abuzz with Canadian’s ‘Loch Ness monster’ photo
-



 Politics24 hours ago
Politics24 hours agoPolitics Briefing: Saskatchewan residents to get carbon rebates despite province’s opposition to pricing program
-
News22 hours ago
What is a halal mortgage? How interest-free home financing works in Canada
-



 Politics15 hours ago
Politics15 hours agoOpinion: Fear the politicization of pensions, no matter the politician
-
Economy21 hours ago
German Business Outlook Hits One-Year High as Economy Heals
-
Media14 hours ago
B.C. puts online harms bill on hold after agreement with social media companies














