Viral fragments of bird flu have been identified in samples of milk taken from grocery store shelves in the United States, a finding that does not necessarily suggest a threat to human health but indicates the avian flu virus is more widespread among dairy herds than previously thought, according to two public health officials and a public health expert who was briefed on the issue.
Health
Ottawa Public Health to host monkeypox vaccine clinics – CBC.ca
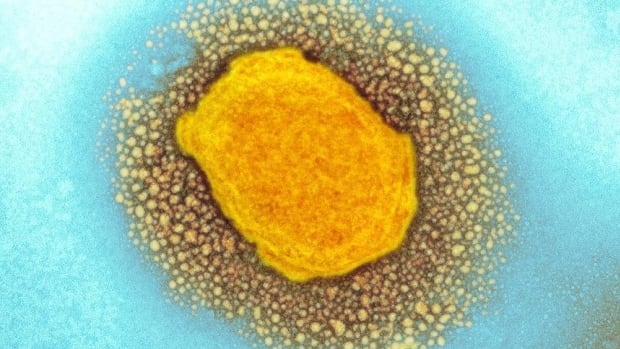
Ottawa Public Health (OPH) is planning vaccine clinics for monkeypox and has begun offering shots to residents who are “highest risk.”
Dr. Vera Etches, Ottawa’s medical officer of health, said the province provided roughly 100 doses over the weekend, which was enough to meet the immediate demand.
However, during Monday’s board of health meeting Etches said she expects interest in getting the vaccine could rise as more people learn it’s available. That’s where the clinics, which have also been held in Toronto and Montreal, would come in.
“In addition to access through our sexual health centre, we’re also planning additional clinics with partners who can best connect with communities at higher risk,” Etches said.
Public health reported the first positive case of monkeypox in Ottawa on June 10.
That person has since recovered and OPH followed up with close contacts about post-exposure vaccination, Etches said. The risk to the general public remains “very low,” she added.
Following guidance from the Ministry of Health, OPH administered the Imvamune vaccine to high-risk contacts of the confirmed case.
A Public Health Ontario summary about monkeypox states that as of June 16 one confirmed and two suspected cases of the infectious disease have been reported in Ottawa. Thirty confirmed cases have been recorded across the province.
Deep, ‘painful’ pustules
Virologist Earl Brown said monkeypox comes with a key feature — large lesions that usually start on the head and hands but can spread to other parts of the body.
“They are very uncomfortable apparently and painful,” the University of Ottawa professor emeritus explained.
“They’ve very deep pustules, they’re right into your skin and they’re little volcanoes since they’re full of clear fluid.”
We will begin offering vaccination this weekend to the highest priority individuals based on the latest provincial eligibility criteria. Those who are eligible will be contacted directly. (5/7)
—@OttawaHealth
Those sores dry and then drop off “loaded with virus,” Brown said. That’s one way the virus can spread, but the infection can pass through close contact as well as exposed skin, the respiratory tract or mucous membranes around a person’s eyes, mouth and nose.
The rare disease comes from the same family of viruses that cause smallpox, which the World Health Organization declared eradicated in 1980, but it’s “much milder,” said Brown.
Information session Thursday
Infectious disease specialists say the LGBTQ community, particularly men who have sex with men, are at disproportionate risk of infection in this outbreak. Health-care workers or lab workers who work directly with orthopoxviruses could also be at risk.
The AIDS Committee of Ottawa is set to host an information session about monkeypox on Thursday where Dr. Paul MacPherson will be on hand to answer questions from 6 p.m. to 8 p.m.
Cory Wong, manager of support services for the committee, said there’s a “sense of urgency” among those who use its services and he’s already fielded a lot of questions about when the vaccine will be available.
“It’s very relevant to people who we work with, including men who have sex with men, racialized community members and people who live with HIV with compromised immune systems,” Wong explained, adding there are concerns in the community about stigma.
ACO has been keeping a close eye on how Monkey Pox is progressing and we have invited Dr. Paul MacPherson to provide community partners and service workers with an educational zoom workshop and update on the status of Monkey Pox. <a href=”https://t.co/RO0d3WrFRN”>pic.twitter.com/RO0d3WrFRN</a>
—@ACOttawa
Brown was quick to point out that monkeypox is not a sexually transmitted disease, but that sex puts people in close contact. Those who are at high-risk should keep an eye out for symptoms and have any unusual rashes checked out by a health professional.
Right now, officials are taking a targeted approach to vaccination, said the virologist.
As for the rest of Ontarians, they can rely on lessons learned during the pandemic.
“We’re quite sensitive with COVID-19 still ongoing here,” said Brown. “Distancing and hand washing will go a long way to stopping the spread of monkeypox as well.”
Health
Bird flu virus found in grocery milk as officials say supply still safe – The Washington Post

The Food and Drug Administration said Tuesday that it had been testing milk samples throughout the dairy production process and confirmed the detection of viral particles “in some of the samples,” but it declined to provide details.
The presence of genetic fragments of the virus in milk is not unexpected. Pasteurization typically works to inactivate pathogens, said Jennifer Nuzzo, director of the Pandemic Center at the Brown University School of Public Health. It generally does not remove genetic material, Nuzzo said, but typically renders pathogens unable to cause harm to people.
The greater concern, however, “is that it’s showing up in a lot more samples, meaning the infection is more widespread in dairy herds than we thought,” said one public health official, who spoke on the condition of anonymity to share information not yet made public.
In a four-page statement, the FDA said some of the samples collected have “indicated the presence” of the bird flu virus based on testing that detects viral particles but does not distinguish whether they are active or dead. The finding of virus “does not mean that the sample contains an intact, infectious pathogen,” the agency’s statement said.
Additional laboratory testing is underway to grow the virus in cells and in fertilized eggs, the latter being the “gold standard” for sensitive detection of active, infectious virus, the FDA said. “Importantly, additional testing is required to determine whether intact pathogen is still present and if it remains infectious, which determines whether there is any risk of illness associated with consuming the product,” the FDA statement said.
FDA officials said results are expected in the next few days to weeks.
“To date, we have seen nothing that would change our assessment that the commercial milk supply is safe,” the agency said in its statement.
Officials and experts did not have additional details about the number of milk samples that were positive for particles of bird flu or where the samples originated.
Although this strain of avian flu has been circulating for more than 20 years, its leap into cows is of substantial concern, surprising even longtime observers of the virus. More than two dozen livestock herds in at least eight states have been infected with avian flu since March 25, prompting investigations by federal and state officials.
For weeks, key federal agencies have expressed confidence in the safety of the commercial milk supply, including pasteurized products sold at grocery stores. The FDA has highlighted data showing pasteurization inactivates other viruses and pointed to studies showing that the pasteurization process for eggs — which occurs at a lower temperature than what is used for milk — deactivates the highly pathogenic avian influenza.
The International Dairy Foods Association, which represents the nation’s dairy manufacturing and marketing industry, said that viral fragments are “nothing more than evidence that the virus is dead.”
“Milk and milk products produced and processed in the United States are among the safest in the world,” spokesman Matt Herrick wrote in an email, adding that “viral fragments are simply indicative of pasteurization doing its job effectively and protecting our commercial milk supply.”
In recent weeks, multiple experts expressed confidence that the pasteurization process ensures there is no threat to the safety of the nation’s milk supply but said the federal government should still perform tests to confirm that is the case.
Flu is a “fairly wimpy virus,” meaning it is “fairly readily inactivated,” said Richard J. Webby, a virologist at St Jude Children’s Research Hospital. “But that’s something that has to be tested.”
One case of avian flu has been reported in a Texas farmworker in recent weeks, only the second human case ever of bird flu in the United States.
So far, the virus has not acquired the ability to spread efficiently in people.
But as it is able to jump from animal to animal, prospects increase for it mutating to cause sustained person-to-person transmission — a development that could fuel a pandemic.
State health officials have tested 23 people with flu-like symptoms, but only the dairy worker in Texas has tested positive during the current outbreak. Ongoing surveillance of emergency department visits and flu tests in regions where bird flu has been detected has not flagged unusual trends in flu-like illnesses, or eye inflammation, the only symptom experienced by the dairy worker, according to officials at the Centers for Disease Control and Prevention, who say the risk to the general public of bird flu remains low.
The lack of more human cases is a good sign, health officials say.
The key to containing the outbreak resides in livestock herds. Testing of cows is voluntary. U.S. Department of Agriculture protocols restrict testing to cows with specific symptoms and limits the number of tests per farm.
Health
Avian influenza spread: WHO gives public health warning as FDA calms food safety concerns – Food Ingredients First


23 April 2024 — The World Health Organization (WHO) has warned that the ongoing spread of avian influenza poses a “significant public health concern” and urged health authorities, especially in the US, to closely monitor infections in cows. However, the US FDA maintains that the virus is not currently a concern to consumer health and downplayed its impact on commercial milk production.
Earlier this month, the largest producer of fresh eggs in the US halted production at a Texas plant after bird flu was detected in its chickens. Cal-Maine Foods said that about 3.6% of its total flock was destroyed after the infection.
However, the virus, also known as H5N1, has now been found in at least 26 dairy herds across eight US states, marking the first time this strain of bird flu has been detected in cattle, according to officials.
At least 21 states have restricted cattle importations from states where the virus is known to have infected dairy cows.
The US Department of Agriculture’s Animal and Plant Health Inspection Service strongly recommends minimizing the movement of cattle, but has not issued federal quarantine orders.
Public health threat
The US Centers for Disease Control and Prevention (CDC) confirmed this month that a dairy worker in Texas, who reportedly had exposure to dairy cattle presumed to have had avian influenza, contracted the virus and is now recovering.
“This infection does not change the H5N1 bird flu human health risk assessment for the US general public, which CDC considers to be low,” the agency said in a press release, while acknowledging that people who come into more frequent contact with possibly infected birds or other mammals have a higher risk.
Meanwhile, WHO’s chief scientist, Dr. Jeremy Farrar, told reporters recently in Geneva, Switzerland, that H5N1 has had an “extremely high” mortality rate among the several hundred people known to have been infected with it to date.


“H5N1 is an influenza infection, predominantly started in poultry and ducks and has spread effectively over the course of the last one or two years to become a global zoonotic — animal — pandemic,” said Farrar.
“The great concern, of course, is that in doing so and infecting ducks and chickens — but now increasingly mammals — the virus now evolves and develops the ability to infect humans.
“And then critically, the ability to go from human-to-human transmission.”
Concerns with cattle
US health officials have stressed that bird flu’s risk to the public is low, and the country’s food supply remains safe and stable.
“At this time, there continues to be no concern that this circumstance poses a risk to consumer health or that it affects the safety of the interstate commercial milk supply,” the FDA said in a statement.
According to officials, farmers are being urged to test cows that show symptoms of infection and separate them from the herd, where they usually recover within two weeks.
US producers are not permitted to sell milk from sick cows, while milk sold across state lines must be pasteurized or heat-treated to kill viruses, including influenza.

“We firmly believe that pasteurization provides a safe milk supply,” Tracey Forfa, director of the FDA’s Center for Veterinary Medicine, told a webinar audience last week.
However, WHO’s Farrar has urged further caution by public health authorities “because it [the virus] may evolve into transmitting in different ways.”
“Do the milking structures of cows create aerosols? Is it the environment which they’re living in? Is it the transport system that is spreading this around the country?” he said.
“This is a huge concern, and I think we have to…make sure that if H5N1 did come across to humans with human-to-human transmission that we were in a position to immediately respond with access equitably to vaccines, therapeutics and diagnostics.”
According to a new European Food Safety Authority report, outbreaks of avian influenza continue to spread in the EU and beyond.
By Joshua Poole
To contact our editorial team please email us at
editorial@cnsmedia.com
If you found this article valuable, you may wish to receive our newsletters.
Subscribe now to receive the latest news directly into your inbox.
Health
York Region urges you to get up to date on vaccinations – NewmarketToday.ca

York Region Public Health is reminding residents to keep up to date on their vaccinations as National Immunization Awareness Week begins.
The regional municipality said it is important to stay up to date on recommended vaccinations to ensure protection from contagious diseases. That includes updated COVID-19 vaccinations for vulnerable populations, recommended as part of a spring vaccination campaign.
“We know vaccines are safe and the best way to stay protected against vaccine-preventable disease,” the region said in a news release.
National Immunization Awareness Week runs from April 22 to 30, with this year’s theme being “Protect your future, get immunized.”
This spring, the region is still doing COVID-19 vaccinations. While walk-ins are no longer available as of April 2, you can book an appointment to visit a York Region clinic.
The spring COVID-19 vaccination campaign is aimed at more vulnerable groups who have received a COVID-19 vaccine before. Those include seniors, those living in seniors living facilities like long-term care homes, immunocompromised individuals and those in Indigenous households who are 55 or older. Public health also recommends the COVID-19 vaccine for those who have not yet received one.
York Region Public Health is also reminding residents of the need for other vaccines.
Measles cases have sprung up in Ontario and York Region recently. The region is recommending that people ensure they previously raised two valid doses of the measles vaccine. The region will also start providing measles vaccines April 29 for those overdue and for who do not have access to the vaccine through a health-care provider.
School-aged vaccinations are also available for free for children in junior kindergarten to Grade 12.
You can access immunization information at york.ca/immunziations or by contacting Access York at 1-877-464-9675.
“Vaccination helps protect everyone in our families, communities and schools,” the region said. “ By continuing to stay up to date on your immunizations, you help protect infants who are too young to be vaccinated and those not able to get vaccinated due to medical conditions.”
-



 Science22 hours ago
Science22 hours agoOsoyoos commuters invited to celebrate Earth Day with the Leg Day challenge – Oliver/Osoyoos News – Castanet.net
-



 Politics22 hours ago
Politics22 hours agoHaberman on why David Pecker testifying is ‘fundamentally different’ – CNN
-
News23 hours ago
Freeland defends budget measures, as premiers push back on federal involvement – CBC News
-
Economy23 hours ago
The Fed's Forecasting Method Looks Increasingly Outdated as Bernanke Pitches an Alternative – Bloomberg
-



 Health21 hours ago
Health21 hours agoIt's possible to rely on plant proteins without sacrificing training gains, new studies say – The Globe and Mail
-
Business22 hours ago
Gildan replacing five directors ahead of AGM, will back two Browning West nominees – Yahoo Canada Finance
-



 Tech21 hours ago
Tech21 hours agoMeta Expands VR Operating System to Third-Party Hardware Makers – MacRumors
-



 Tech23 hours ago
Tech23 hours agoWe tried these three beauty products this week. Here are our thoughts – Vancouver Sun







