Health
Should deer farming be abolished to halt chronic wasting disease? – CBC.ca
Despite ongoing calls from an Ontario hunting group to phase out deer farms — an industry that has contributed to the spread of chronic wasting disease (CWD) — some experts are doubtful it will curb the problem.
The Ontario Federation of Anglers and Hunters has been lobbying since the late 1990s for eliminating the farms, said Keith Munro, a biologist with the organization who specializes in white-tailed deer.
However, a CWD outbreak late last year on a farm in Grenville-sur-la-Rouge, Que., has only exacerbated the federation’s concerns.
“Rather than trying to fix all the little problems, the real effective solution is to phase out the industry,” Munro recently told Radio-Canada.
“CWD is one of the greatest threats to wildlife health that we have right now. It’s an incurable, 100 per cent fatal disease that affects all members of the deer family.”
An imperfect solution
The OFAH has proposed to phase out farms over a five-year period, with farmers receiving financial compensation.
While that could reduce the potential for the “movement of infectious agents,” it wouldn’t help eliminate CWD in areas where it’s already appeared in the wild population, said biologist Bryan Richards.
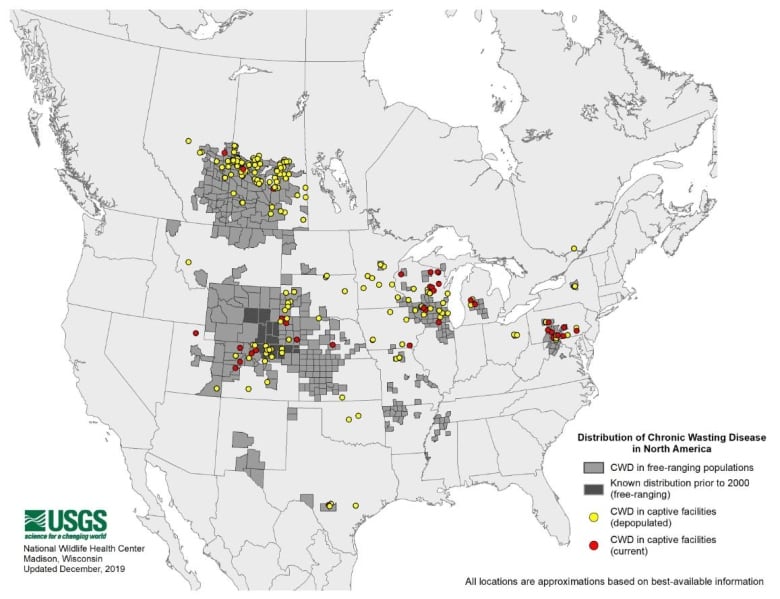
“The abolition of farms would have no impact where CWD exists today,” said Richards, who works with the USGS National Wildlife Health Center, the U.S. government agency that tracks outbreaks in North America.
I’m not sure at this point that phasing out the farms in areas where CWD is already present is going to help.– Debbie McKenzie
Debbie McKenzie, an associate professor of biology at the University of Alberta, has studied CWD for almost 17 years and agrees with her American colleague.
McKenzie said there are many cases where farmed and wild deer are in “close contact,” and fences won’t prevent the spread of the disease.
“I’m not sure at this point that phasing out the farms in areas where CWD is already present is going to help,” McKenzie said.
After CWD was discovered in Grenville-sur-la-Rouge, only 15 kilometres from the Ontario border, the Ministry of Natural Resources stepped up surveillance efforts and urged hunters to drop off samples of wild deer they’d shot and killed for analysis.
Munro said that out of roughly 13,000 wild deer submitted by hunters, however, none have tested positive for CWD.


The nearly invisible disease
CWD has been found in three Canadian provinces — Alberta, Saskatchewan, and Quebec — as well as 26 U.S. states, South Korea, Norway, Sweden and Finland.
On top of it being a fatal disease that attacks all species of deer, it’s also virtually undetectable in a live animal — until it’s too late.
“An animal that gets sick today would not show any symptoms for perhaps 18 months,” Richards said.
Long before symptoms show up, an animal infected with CWD can still spread it within three months after contracting the disease, Richards said.
The only way to detect CWD beyond a doubt is to kill a deer and test brain tissue or lymph nodes.


Strict supervision necessary
While there’s no consensus on whether farms should be eliminated, specialists agree it’s essential to properly supervise the transport of deer.
Munro said it’s better to focus protection efforts on the wild herd, given the economic weight of the hunting industry in Ontario, where there are more than 600 moose and deer hunting businesses.
Unlike the OFAH, the Fédération québécoise des chasseurs et pêcheurs is not opposed to deer farming, even though the disease was first detected in the Outaouais.
In Quebec, deer farmers are subject to many strict regulations on the importation, identification, monitoring and testing of their animals — areas where the OFAH would like to see reforms in Ontario.
The province has recently developed a surveillance and response plan that includes “restrictions on the export of certain animals from jurisdictions where [CWD] has been detected,” according to a news release from the Ministry of Natural Resources.
Abolishing the farms is not the only solution put forward by the OFAH: Munro also advocates for better public education and testing of all farmed animals sent for slaughter in Ontario.
Health
RCMP warn about benzodiazepine-laced fentanyl tied to overdose in Alberta – Edmonton Journal


Article content
Grande Prairie RCMP issued a warning Friday after it was revealed fentanyl linked to a deadly overdose was mixed with a chemical that doesn’t respond to naloxone treatment.
The drugs were initially seized on Feb. 28 after a fatal overdose, and this week, Health Canada reported back to Mounties that the fentanyl had been mixed with Bromazolam, which is a benzodiazepine.
Article content
Mounties say this is the first recorded instance of Bromazolam in Alberta. The drug has previously been linked to nine fatal overdoses in New Brunswick in 2022.
The pills seized in Alberta were oval-shaped and stamped with “20” and “SS,” though Mounties say it can come in other forms.
Naloxone treatment, given in many cases of opioid toxicity, is not effective in reversing the effects of Bromazalam, Mounties said, and therefore, any fentanyl mixed with the benzodiazepine “would see a reduced effectiveness of naloxone, requiring the use of additional doses and may still result in a fatality.”
From January to November of last year, there were 1,706 opioid-related deaths in Alberta, and 57 linked to benzodiazepine, up from 1,375 and 43, respectively, in 2022.
Mounties say officers responded to about 1,100 opioid-related calls for service, last year with a third of those proving fatal. RCMP officers also used naloxone 67 times while in the field, a jump of nearly a third over the previous year.
Recommended from Editorial
Share this article in your social network
Health
CFIA continues surveillance for HPAI in cattle, while sticking with original name for disease – RealAgriculture


The Canada Food Inspection Agency will continue to refer to highly pathogenic avian influenza in cattle as HPAI in cattle, and not refer to it as bovine influenza A virus (BIAV), as suggested by the American Association of Bovine Practitioners earlier this month.
Dr. Martin Appelt, senior director for the Canadian Food Inspection Agency, in the interview below, says at this time Canada will stick with “HPAI in cattle” when referencing the disease that’s been confirmed in dairy cattle in multiple states in the U.S.
The CFIA’s naming policy is consistent with the agency’s U.S. counterparts’, as the U.S. Animal and Plant Health Inspection Service has also said it will continue referring to it as HPAI or H5N1.
Appelt explains how the CFIA is learning from the U.S. experience to-date, and how it is working with veterinarians across Canada to stay vigilant for signs of the disease in dairy and beef cattle.
As of April 19, there has not been a confirmed case of HPAI in cattle in Canada. Appelt says it’s too soon to say if an eventual positive case will significantly restrict animal movement, as is the case with positive poultry cases.
This is a major concern for the cattle industry, as beef cattle especially move north and south across the U.S. border by the thousands. Appelt says that CFIA will address an infection in each species differently in conjunction with how the disease is spread and the threat to neighbouring farms or livestock.
Currently, provincial dairy organizations have advised producers to postpone any non-essential tours of dairy barns, as a precaution, in addition to other biosecurity measures to reduce the risk of cattle contracting HPAI.
Subscribe: Apple Podcasts | Spotify | RSS | All Podcasts
jQuery(document).ready(function($) {
$(“#homesub”).validate(
rules:
first_name:
required: true,
minlength: 2
,
last_name:
required: true,
minlength: 2
,
email:
required: true,
email: true,
minlength: 2
,
state:
required: true,
,
role:
required: true,
,
“listid[]”:
required: true,
minlength: 1
,
messages:
first_name: “Your first name is required.”,
last_name: “Your last name is required.”,
email: “Please verify your email is correct.”,
state: “Your state/province is required.”,
role: “Your role is required.”,
“listid[]”: “Select at least one list is required.”
,
submitHandler: function()
$.ajax(
type: “POST”,
url: “https://www.realagriculture.com/wp-admin/admin-ajax.php”,
data:
action: “realag_cc_process_subscribe_onclick”,
form: “homesub”,
data: $(“#homesub”).serialize(),
,
dataType: “html”,
timeout: 30000,
error: function(response)
console.log(response);
,
success: function(response)
$(“#homesub”).html(response);
,
);
);
});
Health
Toronto reports 2 more measles cases. Use our tool to check the spread in Canada – Toronto Star
/* OOVVUU Targeting */
const path = ‘/news/canada’;
const siteName = ‘thestar.com’;
let domain = ‘thestar.com’;
if (siteName === ‘thestar.com’)
domain = ‘thestar.com’;
else if (siteName === ‘niagarafallsreview.ca’)
domain = ‘niagara_falls_review’;
else if (siteName === ‘stcatharinesstandard.ca’)
domain = ‘st_catharines_standard’;
else if (siteName === ‘thepeterboroughexaminer.com’)
domain = ‘the_peterborough_examiner’;
else if (siteName === ‘therecord.com’)
domain = ‘the_record’;
else if (siteName === ‘thespec.com’)
domain = ‘the_spec’;
else if (siteName === ‘wellandtribune.ca’)
domain = ‘welland_tribune’;
else if (siteName === ‘bramptonguardian.com’)
domain = ‘brampton_guardian’;
else if (siteName === ‘caledonenterprise.com’)
domain = ‘caledon_enterprise’;
else if (siteName === ‘cambridgetimes.ca’)
domain = ‘cambridge_times’;
else if (siteName === ‘durhamregion.com’)
domain = ‘durham_region’;
else if (siteName === ‘guelphmercury.com’)
domain = ‘guelph_mercury’;
else if (siteName === ‘insidehalton.com’)
domain = ‘inside_halton’;
else if (siteName === ‘insideottawavalley.com’)
domain = ‘inside_ottawa_valley’;
else if (siteName === ‘mississauga.com’)
domain = ‘mississauga’;
else if (siteName === ‘muskokaregion.com’)
domain = ‘muskoka_region’;
else if (siteName === ‘newhamburgindependent.ca’)
domain = ‘new_hamburg_independent’;
else if (siteName === ‘niagarathisweek.com’)
domain = ‘niagara_this_week’;
else if (siteName === ‘northbaynipissing.com’)
domain = ‘north_bay_nipissing’;
else if (siteName === ‘northumberlandnews.com’)
domain = ‘northumberland_news’;
else if (siteName === ‘orangeville.com’)
domain = ‘orangeville’;
else if (siteName === ‘ourwindsor.ca’)
domain = ‘our_windsor’;
else if (siteName === ‘parrysound.com’)
domain = ‘parrysound’;
else if (siteName === ‘simcoe.com’)
domain = ‘simcoe’;
else if (siteName === ‘theifp.ca’)
domain = ‘the_ifp’;
else if (siteName === ‘waterloochronicle.ca’)
domain = ‘waterloo_chronicle’;
else if (siteName === ‘yorkregion.com’)
domain = ‘york_region’;
let sectionTag = ”;
try
if (domain === ‘thestar.com’ && path.indexOf(‘wires/’) = 0)
sectionTag = ‘/business’;
else if (path.indexOf(‘/autos’) >= 0)
sectionTag = ‘/autos’;
else if (path.indexOf(‘/entertainment’) >= 0)
sectionTag = ‘/entertainment’;
else if (path.indexOf(‘/life’) >= 0)
sectionTag = ‘/life’;
else if (path.indexOf(‘/news’) >= 0)
sectionTag = ‘/news’;
else if (path.indexOf(‘/politics’) >= 0)
sectionTag = ‘/politics’;
else if (path.indexOf(‘/sports’) >= 0)
sectionTag = ‘/sports’;
else if (path.indexOf(‘/opinion’) >= 0)
sectionTag = ‘/opinion’;
} catch (ex)
const descriptionUrl = ‘window.location.href’;
const vid = ‘mediainfo.reference_id’;
const cmsId = ‘2665777’;
let url = `https://pubads.g.doubleclick.net/gampad/ads?iu=/58580620/$domain/video/oovvuu$sectionTag&description_url=$descriptionUrl&vid=$vid&cmsid=$cmsId&tfcd=0&npa=0&sz=640×480&ad_rule=0&gdfp_req=1&output=vast&unviewed_position_start=1&env=vp&impl=s&correlator=`;
url = url.split(‘ ‘).join(”);
window.oovvuuReplacementAdServerURL = url;
Canada has seen a concerning rise in measles cases in the first months of 2024.
By the third week of March, the country had already recorded more than three times the number of cases as all of last year. Canada had just 12 cases of measles in 2023, up from three in 2022.
function buildUserSwitchAccountsForm()
var form = document.getElementById(‘user-local-logout-form-switch-accounts’);
if (form) return;
// build form with javascript since having a form element here breaks the payment modal.
var switchForm = document.createElement(‘form’);
switchForm.setAttribute(‘id’,’user-local-logout-form-switch-accounts’);
switchForm.setAttribute(‘method’,’post’);
switchForm.setAttribute(‘action’,’https://www.thestar.com/tncms/auth/logout/?return=https://www.thestar.com/users/login/?referer_url=https%3A%2F%2Fwww.thestar.com%2Fnews%2Fcanada%2Ftoronto-reports-2-more-measles-cases-use-our-tool-to-check-the-spread-in-canada%2Farticle_20aa7df4-e88f-11ee-8fad-8f8368d7ff53.html’);
switchForm.setAttribute(‘style’,’display:none;’);
var refUrl = document.createElement(‘input’); //input element, text
refUrl.setAttribute(‘type’,’hidden’);
refUrl.setAttribute(‘name’,’referer_url’);
refUrl.setAttribute(‘value’,’https://www.thestar.com/news/canada/toronto-reports-2-more-measles-cases-use-our-tool-to-check-the-spread-in-canada/article_20aa7df4-e88f-11ee-8fad-8f8368d7ff53.html’);
var submit = document.createElement(‘input’);
submit.setAttribute(‘type’,’submit’);
submit.setAttribute(‘name’,’logout’);
submit.setAttribute(‘value’,’Logout’);
switchForm.appendChild(refUrl);
switchForm.appendChild(submit);
document.getElementsByTagName(‘body’)[0].appendChild(switchForm);
function handleUserSwitchAccounts()
window.sessionStorage.removeItem(‘bd-viafoura-oidc’); // clear viafoura JWT token
// logout user before sending them to login page via return url
document.getElementById(‘user-local-logout-form-switch-accounts’).submit();
return false;
buildUserSwitchAccountsForm();
#ont-map-iframepadding:0;width:100%;border:0;overflow:hidden;
#ontario-cases-iframepadding:0;width:100%;border:0;overflow:hidden;
#province-table-iframepadding:0;width:100%;border:0;overflow:hidden;
console.log(‘=====> bRemoveLastParagraph: ‘,0);
-
Real eState17 hours ago
Botched home sale costs Winnipeg man his right to sell real estate in Manitoba – CBC.ca
-
News24 hours ago
Canada Child Benefit payment on Friday | CTV News – CTV News Toronto
-
Business17 hours ago
Dow Jones Rises But S&P, Nasdaq Fall; Nvidia, SMCI Flash Sell Signals As Bitcoin's Fourth Halving Arrives – Investor's Business Daily
-



 Science15 hours ago
Science15 hours agoDragonfly: NASA greenlights most important mission of the century – Earth.com
-



 Science22 hours ago
Science22 hours agoMarine plankton could act as alert in mass extinction event: UVic researcher – Langley Advance Times
-
Art16 hours ago
Art and Ephemera Once Owned by Pioneering Artist Mary Beth Edelson Discarded on the Street in SoHo – artnet News
-


 Tech22 hours ago
Tech22 hours agoNothing Ear And Nothing Ear (a) Earbuds Are 1st With ChatGPT Integration – Forbes
-



 Investment22 hours ago
Investment22 hours agoJohn Ivison: The blowback to Trudeau's investment tax hike could be bigger than he thinks – National Post







