Health
This Early Symptom is One You Should Watch for With Omicron Infections Rising

|
|
This Early Symptom is One You Should Watch for With Omicron Infections Rising
If you’ve been exposed to someone with COVID and are watching for symptoms, what are some of the first signs you might be infected?
If you’ve been exposed to someone with COVID and are watching for symptoms, what are some of the first signs you might be infected?
It’s a question many are asking as omicron cases surge across the country and as the Centers for Disease Control and Prevention update their quarantine and isolation guidelines, which now differ depending on whether or not you have a symptomatic infection.
Here’s what we know so far.
What are some of the first symptoms with omicron?
Sore throat continues to be a symptom reported, particularly in mild breakthrough infections, Chicago Department of Public Health Commissioner Dr. Allison Arwady said during a Facebook Live Tuesday.
“Especially in people who we’re seeing these more mild breakthrough infections, we are definitely seeing sore throat be a predictor in that group,” Arwady said.
She repeated earlier calls for people who have any flu- or cold-like symptoms to assume they have COVID “until proven otherwise.”
“Even if it’s a sore throat, no matter what it is,” she said. “I’ve told my own staff this, it’s what I do myself… if you are sick, even a little bit sick, stay home. More true than ever right now because sick, even a little bit sick, until proven otherwise with a test – that’s COVID. That’s how we treat it, that’s how you should treat it.”
What are the other symptoms to watch for after COVID exposure?
With some omicron cases, particularly breakthrough infections in those who are boosted and vaccinated, remaining mild, many are wondering how to tell if it’s a cold, the flu or COVID-19.
Arwady said that now, those who are fully vaccinated aren’t necessarily getting “seriously ill and having fevers for days and difficult breathing,” but are instead experiencing a more mild illness.
“They may only feel like they have a cold,” she said. “That’s good because they’re not getting seriously sick, they’re not threatening the healthcare system, but it’s certainly of some concern because they do have the potential to transmit to others.”
Those who are unvaccinated, however, are experiencing similar symptoms to early on in the pandemic, Arwady said.
Arwady’s comments echo those of other medical experts who are watching omicron cases.
Dr. Katherine Poehling, an infectious disease specialist and member of the Advisory Committee on Immunization Practices, told NBC News last week that a cough, congestion, runny nose and fatigue appear to be prominent symptoms with the omicron variant. But unlike delta, many patients are not losing their taste or smell.
The evidence so far, according to Poehling, is anecdotal and not based on scientific research. She noted also that these symptoms may only reflect certain populations.
Still, CDC data showed the most common symptoms so far are cough, fatigue, congestion and a runny nose.
Overall, the symptoms for COVID reported by the CDC include:
- Fever or chills
- Cough
- Shortness of breath or difficulty breathing
- Fatigue
- Muscle or body aches
- Headache
- New loss of taste or smell
- Sore throat
- Congestion or runny nose
- Nausea or vomiting
- Diarrhea
The CDC also has what it calls a “coronavirus self checker” that allows people to answer a series of questions to determine if they should seek medical care.
“The Coronavirus Self-Checker is an interactive clinical assessment tool that will assist individuals ages 13 and older, and parents and caregivers of children ages 2 to 12 on deciding when to seek testing or medical care if they suspect they or someone they know has contracted COVID-19 or has come into close contact with someone who has COVID-19,” the CDC’s website reads.
How soon might COVID symptoms appear?
According to earlier CDC guidance, COVID symptoms can appear anywhere from two to 14 days after someone is exposed to the virus.
Anyone exhibiting symptoms should get tested for COVID-19.
Some people may never experience symptoms, though they can still spread the virus.
A person is also considered contagious before symptoms appear.
When are people with COVID most contagious?
The CDC says that its guidelines were updated to reflect growing evidence that suggests transmission of COVID-19 often occurs one to two days before the onset of symptoms and during the two to three days afterward.
“This has to do with data from the CDC that really showed after seven days there’s virtually no risk of transmission at this point,” Arwady said. “And in that five-to-seven-day window, you know, there’s some depending on whether people have been vaccinated, underlying conditions, etc., but the risk drops a lot and the feeling is that in the general population, combined with masking, etc. the risk really is very low.”
For those without symptoms, CDC guidance states they are considered contagious at least two days before their positive test.
When should you call a doctor?
The CDC urges those who have or may have COVID-19 to watch for emergency warning signs and seek medical care immediately if they experience symptoms including:
- Trouble breathing
- Persistent pain or pressure in the chest
- New confusion
- Inability to wake or stay awake
- Pale, gray, or blue-colored skin, lips, or nail beds, depending on skin tone
“This list is not all possible symptoms,” the CDC states. “Please call your medical provider for any other symptoms that are severe or concerning to you.”
You can also notify the operator that you believe you or someone you are caring for has COVID.
How long after COVID exposure could you test positive?
According to the CDC, the incubation period for COVID is between two and 14 days, though the newest guidance from the agency suggests a quarantine of five days for those who are not boosted, but eligible or unvaccinated. Those looking to get tested after exposure should do so five days after the exposure or if they begin experiencing, the CDC recommends.
Those who are boosted and vaccinated, or those who are fully vaccinated and not yet eligible for a booster shot, do not need to quarantine, but should wear masks for 10 days and also get tested five days after the exposure, unless they are experiencing symptoms.
Still, for those who are vaccinated and boosted but are still looking to be cautious, Chicago Department of Public Health Commissioner Dr. Allison Arwady said an additional test at seven days could help.
“If you’re taking multiple at home tests, you know, the recommendation is five days later take a test. But if you have taken one at five and it’s negative and you’re feeling good, chances are very good that you’re not going to have any more issues there,” she said. “I think if you’re being extra careful there, if you wanted to test again, you know, at seven even, sometimes people look at three to get an earlier sense of things. But if you’re gonna do it once do it in five and I feel good about that.”
Arwady said testing is likely not necessary after seven days following exposure for those who are vaccinated and boosted.
“If you had an exposure, you’re vaccinated and boosted, I don’t think that there is any need to be testing, frankly, past about seven days,” she said. “If you want to be extra careful, you can do it at 10, but just with what we’re seeing, I would consider you really in the clear. If you’re not vaccinated or boosted, I certainly have a much higher concern that you could get infected. Definitely, ideally, you’d be seeking out that test at five and I would do it again, you know, at the seven, potentially at that 10.”
When is the best time to get tested after exposure?
The CDC states that anyone who may have been exposed to someone with COVID should test five days after their exposure, or as soon as symptoms occur.
“If symptoms occur, individuals should immediately quarantine until a negative test confirms symptoms are not attributable to COVID-19,” the guidance states.
Illinois Department of Public Health Director Dr. Ngozi Ezike said that incubation times could be changing, but those who test early should continue testing even if they get negative results.
“We might be learning that the time of incubation might be a little shorter. So maybe you’d be testing at two days,” Ezike said. “Obviously if you’re symptomatic, you test right away. But you know, if you want to test at two days, but that negative test… the two days should not make you think, ‘Oh good, I’m clear,’ you know? You might want to test again and of course symptoms you cannot ignore – scratchy throat, headaches, all kinds of symptoms – anything new can be a symptom of this new illness.”
How long should you quarantine or isolate?
First things first, those who believe they have been in contact with someone who has COVID and are unvaccinated should quarantine. Those who test positive, regardless of vaccination status, must isolate, according to the Centers for Disease Control and Prevention.
Here’s the difference between the two:
Quarantine
Those who have been within six feet of someone with COVID for a cumulative total of at least 15 minutes over a 24-hour period should quarantine for five days if unvaccinated, or if they are more than six months out from their second vaccine dose, according to updated CDC guidance issued Monday.
Once that period ends, they should partake in strict mask use for an additional five days.
Previously, the CDC said people who were not fully vaccinated and who came in close contact with an infected person should stay home for at least 10 days.
Prior to Monday, people who were fully vaccinated — which the CDC has defined as having two doses of the Pfizer or Moderna vaccines, or one dose of the Johnson & Johnson vaccine — could be exempt from quarantine.
Those who are both fully vaccinated and boosted do not need to quarantine if they are a close contact of someone with COVID, but should wear a mask for at least 10 days after exposure. The same goes for those who are fully vaccinated and not yet eligible for their booster shot.
Local health authorities can also make the final determination about how long a quarantine should last, however, and testing can play a role.
Illinois’ health department said it will adopt the CDC revised guidelines on isolation and quarantine for COVID.
In Chicago, those who travel to or from certain parts of the country and are unvaccinated must quarantine upon arrival to the city, but the length of time they should do so for depends on whether they get tested for COVID.
The city has not yet said if the new CDC guidance will change its travel advisory guidelines.
As of Tuesday, the city’s travel advisory recommends those who travel from designated warning states should:
- Get tested with a viral test 3-5 days after travel AND stay home and self-quarantine for a full 7 days.
- Even if you test negative, stay home and self-quarantine for the full 7 days.
- If your test is positive, isolate yourself to protect others from getting infected.
- If you don’t get tested, stay home and self-quarantine for 10 days after travel.
Isolation
People who are positive for COVID should stay home for five days, the CDC said Monday, changing guidance from the previously recommended 10 days.
At the end of the period, if you have no symptoms, you can return to normal activities but must wear a mask everywhere — even at home around others — for at least five more days.
If you still have symptoms after isolating for five days, stay home until you feel better and then start your five days of wearing a mask at all times.
So how do you calculate your isolation period?
According to the CDC, “day 0 is your first day of symptoms.” That means that Day 1 is the first full day after your symptoms developed.
For those who test positive for COVID but have no symptoms, day 0 is the day of the positive test. Those who develop symptoms after testing positive must start their calculations over, however, with day 0 then becoming the first day of symptoms.
Do you need to test out of isolation or quarantine?
Isolation
For those who test positive for COVID and isolate for the required five-day period without symptoms, there is not currently a requirement to test before you see people again, according to the most recent CDC guidance.
“If an individual has access to a test and wants to test, the best approach is to use an antigen test towards the end of the five-day isolation period,” the CDC guidance states. “If your test result is positive, you should continue to isolate until day 10. If your test result is negative, you can end isolation, but continue to wear a well-fitting mask around others at home and in public until day 10.”
The advice for those who tested positive and experienced symptoms also does not indicate a testing requirement, but rather, the person must remain “fever-free for 24 hours without the use of fever-reducing medication” and other symptoms should have improved before they end their isolation, which must last a minimum of five days.
Both symptomatic and asymptomatic people should continue wearing masks around others for an additional five days, the guidance states.
Quarantine
For those in quarantine, however, the guidance is different.
According to the CDC, those exposed to COVID who develop symptoms should test immediately and enter isolation protocols until they receive their results and if they positive.
Those who do not develop symptoms should get tested at least five days after their exposure and, if negative, can leave their home but should continue masking until the 10-day mark.
Why don’t you need to test out of isolation?
The CDC notes that tests “are best used early in the course of illness to diagnose COVID-19 and are not authorized by the U.S. Food and Drug Administration to evaluate duration of infectiousness.”
“While a positive antigen test likely means a person has residual transmissible virus and can potentially infect others, a negative antigen test does not necessarily indicate the absence of transmissible virus,” the CDC’s website reads. “As such, regardless of the test result, wearing a well-fitting mask is still recommended.”
The CDC’s most recent guidance came as many experts expected a testing requirement to be added, but it also comes at a time when testing shortages are being reported nationwide.
“I do not think that the clarification helped at all and I actually think that it made things worse,” emergency physician Dr. Leanna Wen, the former health commissioner of Baltimore, said in an interview with CNN. “I think they should be upfront and say they can’t do this because they don’t have enough tests.”
Chicago’s top doctor, however, said the reason behind the CDC’s decision to not add a testing requirement could be related to changes brought by recent variants.
“You don’t need to have a negative test to come out of isolation, particularly if you’re vaccinated or boosted, because we see lower rates, overall, of infection, shorter times of transmission,” Chicago Department of Public Health Commissioner Dr. Allison Arwady said.
Testing demand continues to soar across the country and state and some experts say the omicron variant has “sped up” timing for what many have come to know with COVID.
“With delta and and with omicron, everything’s been speeding up. That incubation period is shorter, the time that someone is infectious is shorter and therefore the quarantine period, as long as people have recovered, can be shortened,” Arwady said. “Really, after seven days, especially if your symptoms are better, there’s like no evidence that you’re still a transmitting COVID.”
What kind of test should you use if you do want to test before leaving isolation?
The CDC recommends antigen testing for those looking to test before leaving isolation.
Arwady said that guidance is likely related to determining whether or not someone has an “active” virus.
“If you did want to get a test on please don’t get a PCR. Use it rapid antigen test,” she said. “Why? Because the rapid antigen test is the one that will look to see…do you have a high enough COVID level that you are potentially infectious? Now, a PCR test, remember, can pick up up sort of traces of the virus for a long time, even if that virus is bad and even if it’s not potentially transmitting. We sometimes see PCR tests stay positive for weeks even after someone has been infected. But… that is not live COVID that you can grow on a plate that is spreading.”
Health
Quebec successfully pushes back against rise in measles cases – CBC.ca
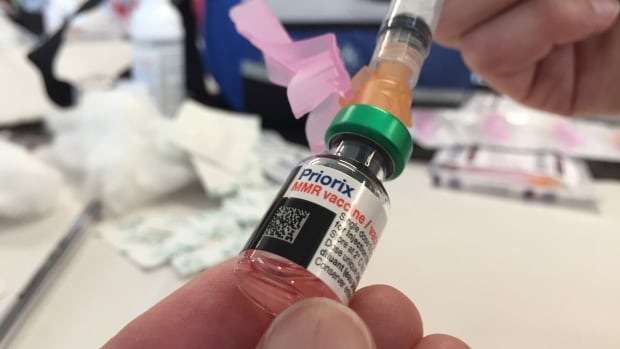
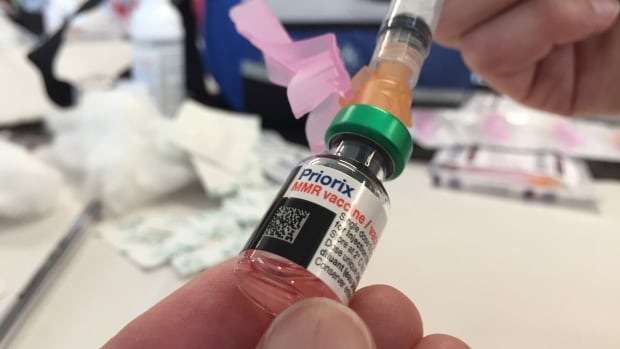
Quebec appears to be winning its battle against the rising tide of measles after 45 cases were confirmed province-wide this year.
“We’ve had no locally transmitted measles cases since March 25, so that’s good news,” said Dr. Paul Le Guerrier, responsible for immunization for Montreal Public Health.
There are 17 patients with measles in Quebec currently, and the most recent case is somebody who was infected while abroad, he said.
But it was no small task to get to this point.
Le Guerrier said once local transmission was detected, news was spread fast among health centres to ensure proper protocols were followed — such as not letting potentially infected people sit in waiting rooms for hours on end.
Then about 90 staffers were put to work, tracking down those who were in contact with positive cases and are not properly vaccinated. They were given post-exposure prophylaxis, which prevents disease, said Le Guerrier.
From there, a vaccination campaign was launched, especially in daycares, schools and neighbourhoods with low inoculation rates. There was an effort to convince parents to get their children vaccinated.
Vaccination in schools boosted
Some schools, mostly in Montreal, had vaccination rates as low as 30 or 40 per cent.
“Vaccination was well accepted and parents responded well,” said Le Guerrier. “Some schools went from very low to as high as 85 to 90 per cent vaccination coverage.”
But it’s not only children who aren’t properly vaccinated. Le Guerrier said people need two doses after age one to be fully inoculated, and he encouraged people to check their status.
There are all kinds of reasons why people aren’t vaccinated, but it’s only about five per cent who are against immunization, he said. So far, some 10,000 people have been vaccinated against measles province-wide during this campaign, Le Guerrier said.
The next step is to continue pushing for further vaccination, but he said, small outbreaks are likely in the future as measles is spreading abroad and travellers are likely to bring it back with them.
Need to improve vaccination rate, expert says
Dr. Donald Vinh, an infectious diseases specialist from the McGill University Health Centre, said it’s not time to rest on our laurels, but this is a good indication that public health is able to take action quickly and that people are willing to listen to health recommendations.
“We are not seeing new cases or at least the new cases are not exceeding the number of cases that we can handle,” said Vinh.
“So these are all reassuring signs, but I don’t think it’s a sign that we need to become complacent.”
Vinh said there are also signs that the public is lagging in vaccine coverage and it’s important to respond to this with improved education and access. Otherwise, microbes capitalize on our weaknesses, he said.
Getting vaccination coverage up to an adequate level is necessary, Vinh said, or more small outbreaks like this will continue to happen.
“And it’s very possible that we may not be able to get one under control if we don’t react quickly enough,” he said.
Health
Pregnant women in the Black Country urged to get whooping cough vaccine – BBC.com


Pregnant women urged to get whooping cough vaccine
Pregnant women in the Black Country are being urged to get vaccinated against whooping cough after a rise in cases.
The bacterial infection of the lungs spreads very easily and can cause serious problems, especially in babies and young children.
The Black Country Integrated Care Board (ICB) is advising pregnant women between 16 and 32 weeks to contact their GP to get the vaccine so their baby has protection from birth.
The UK Health Security Agency warned earlier this year of a steady decline in uptake of the vaccine in pregnant women and children.
Symptoms of the infection, also known as “100-day cough”, are similar to a cold, with a runny nose and sore throat.
Sally Roberts, chief nursing officer for the ICB, which covers Wolverhampton, Dudley, Walsall and Sandwell, said anyone could catch it, but it was more serious for young children and babies.
“Getting vaccinated while you’re pregnant is highly effective in protecting your baby from developing whooping cough in the first few weeks of their life – ideally from 16 weeks up to 32 weeks of pregnancy,” she said.
“If for any reason you miss having the vaccine, you can still have it up until you go into labour.”
Follow BBC West Midlands on Facebook, X and Instagram. Send your story ideas to: newsonline.westmidlands@bbc.co.uk
Health
Measles cases stabilize in Montreal – CityNews Montreal
The number of measles cases has stabilized, according to the Montreal Public Health.
Since March 25, there have been no contaminations reported within the community.
“Our teams have identified all contact cases of measles,” said media relations advisor Geneviève Paradis. “It’s a laborious task: each measles case produces hundreds of contacts.”
All community transmission cases since February 2024 have been caused by returning travelers who were either unvaccinated or partially vaccinated.
Currently, there are 18 measles cases in Montreal – with 46 total in Quebec. This according to the April 18 figures from the provincial government.
“With the summer vacations approaching, if you’re travelling, it is essential to check if you are protected against measles,” explained Paradis.
According to Montreal Public Health, a person needs to have received two doses after the age of 12 months to be immunized against the virus.
They’ve launched a vaccination campaign throughout the region, and currently, 11,341 people have been vaccinated against measles in Montreal between March 19 and April 15.
Vaccination is also being provided in schools and at local service points.
“The vaccination operation is under the responsibility of the five CIUSSS of the territory,” concluded Paradis.
-



 Tech21 hours ago
Tech21 hours agoCytiva Showcases Single-Use Mixing System at INTERPHEX 2024 – BioPharm International
-



 Health17 hours ago
Health17 hours agoSupervised consumption sites urgently needed, says study – Sudbury.com
-
News23 hours ago
Tim Hortons says 'technical errors' falsely told people they won $55K boat in Roll Up To Win promo – CBC.ca
-



 Tech23 hours ago
Tech23 hours agoAaron Sluchinski adds Kyle Doering to lineup for next season – Sportsnet.ca
-



 Politics23 hours ago
Politics23 hours agoTrump faces political risks as trial begins – NBC News
-
Tech22 hours ago
Nintendo Indie World Showcase April 2024 – Every Announcement, Game Reveal & Trailer – Nintendo Life
-
News15 hours ago
2024 federal budget's key takeaways: Housing and carbon rebates, students and sin taxes – CBC News
-
News16 hours ago
Canada's 2024 budget announces 'halal mortgages'. Here's what to know – National Post







