Health
Today’s coronavirus news: Heavy police presence expected across Quebec as 8 p.m. curfew kicks off; Canada’s first case of South Africa COVID-19 variant found in Alberta – Toronto Star
/https://www.thestar.com/content/dam/thestar/news/canada/2021/01/09/todays-coronavirus-news-coronavirus-updates-covid-19-canada-ontario-ontario-gta-jan-9-2021/coronavirus_toronto.jpg)
/https://www.thestar.com/content/dam/thestar/news/canada/2021/01/09/todays-coronavirus-news-coronavirus-updates-covid-19-canada-ontario-ontario-gta-jan-9-2021/coronavirus_toronto.jpg)
The latest coronavirus news from Canada and around the world Saturday. This file will be updated throughout the day. Web links to longer stories if available.
8:11 a.m.: The few hours it took to give the first coronavirus vaccine shots to 14 residents of the John XXIII nursing home — named after a pope and not far from the birthplace in eastern France of vaccine pioneer Louis Pasteur — took weeks of preparation.
The home’s director, Samuel Robbe, first had to chew his way through a dense 61-page vaccination protocol, one of several hefty guides from the French government that exhaustively detail how to proceed, down to the number of times (10) that each flask of vaccine should be turned upside down to mix its contents.
“Delicately,” the booklet stipulates. “Do not shake.”
As France tries to figure out why its vaccination campaign launched so slowly, the answer lies partly in forests of red tape and the decision to prioritize vulnerable older people in nursing homes. They are perhaps the toughest group to start with, because of the need for informed consent and difficulties explaining the complex science of fast-tracked vaccines.
Claude Fouet, still full of vim and good humour at age 89 but with memory problems, was among the first in his Paris care home to agree to a vaccination. But in conversation, it quickly becomes apparent that his understanding of the pandemic is spotty. Eve Guillaume, the home’s director, had to remind Fouet that in April he survived his own brush with the virus that has killed more than 66,000 people in France.
“I was in hospital,” Fouet slowly recalled, “with a dead person next to me.”
Guillaume says that getting consent from her 64 residents — or their guardians and families when they are not fit enough to agree themselves — is proving to be the most labour-intensive part of her preparations to start inoculations later this month. Some families have said no, and some want to wait a few months to see how vaccinations unfold before deciding.
“You can’t count on medicalized care homes to go quickly,” she says. “It means, each time, starting a conversation with families, talking with guardians, taking collegial steps to reach the right decision. And that takes time.”
At the John XXIII home, between the fortified town of Besancon and Pasteur’s birthplace in Dole, Robbe has had a similar experience.
After the European Union green-lighted use of the BioNTech-Pfizer vaccine in December, Robbe says it took two weeks to put together all the pieces to this week vaccinate 14 residents, just a fraction of his total of more than 100.
Getting consent was the biggest hurdle for a doctor and a psychologist who went from room to room to discuss vaccinations, he says. The families of residents were given a week over the December holidays to approve or refuse, a decision that had to be unanimous from immediate family members.
When one woman’s daughter said yes but her son said no, a shot wasn’t given because “they can turn against us and say, ‘I never agreed to that,’” Robbe explained. “No consensus, we don’t vaccinate.”
Only by cutting corners and perfunctorily getting residents to agree could the process go quicker, he says.
“My friends are saying, ‘What is this circus? The Germans have already vaccinated 80,000 people and we’ve vaccinated no one,'” he says. “But we don’t share the same histories. When you propose a vaccine to Germans, they all want to get inoculated. In France, there is a lot of reticence about the history of vaccinations. People are more skeptical. They need to understand. They need explications and to be reassured.”
France prioritized nursing homes because they have seen nearly one-third of its deaths. But its first vaccination on Dec. 27, of a 78-year-old woman in a long-term care facility, quickly proved to have been only the symbolic launch of a rollout that the government never intended to get properly underway before this week.
Only on Monday, as scheduled, did authorities launch an online platform where health workers must log all vaccinations and show that those inoculated got an obligatory consultation with a doctor, adding to the red tape.
In some countries that are moving faster than France, the bureaucracy is leaner. In Britain, where nearly 1.5 million have been inoculated and plans are to offer jabs to all nursing home residents by the end of January, those capable of consenting need only sign a one-page form that gives basic information about the benefits and possible side effects.
No doctor interviews are needed in Spain. It started vaccinating the same day as France but administered 82,000 doses in the first nine days, whereas France managed just a couple of thousand.
Germany, like France, also mandates a meeting with a doctor and is prioritizing shots for care home residents, but it is getting to them quicker, using mobile teams. At its current rate of nearly 30,000 vaccinations per day, Germany would need at least six years to inoculate its 69 million adults. But while the German government is facing criticism for the perceived slow rollout, France made an even more leisurely start, at least in numerical terms, but has pledged to reach 1 million people by the end of January.
Other countries have racked up bigger numbers by offering shots to broader cross-sections of people who are easier to reach and can get themselves to appointments. The large majority of the more than 400,000 doses administered in Italy have gone to health-care workers.
Lucile Grillon, who manages three nursing homes in eastern France, says the many hours invested to prepare vaccinations for 50 residents and staff who got jabs on Friday was time well spent. She worked through the holidays to get ready.
“We can’t wait until we have the doses in our fridge to realize that we’re not ready to vaccinate and then have to throw doses away and say, ‘Rats! I didn’t think of that,’” she adds. “The doses are too precious.”
“It takes us two months to prepare for flu shots. Here, we have been asked to set records, to vaccinate against COVID in under 15 days,” she says. “I don’t see how we could have gone any quicker.”
7:45 a.m.: Dramatic changes will be needed in Canada’s COVID-19 vaccine supply and distribution if there is any hope of meeting the federal government’s goal of vaccinating most Canadians by the end of the year.
A Star analysis shows that the current average speed of vaccinations – about 23,400 per day, according to the latest figures – needs to be about 6.5 times faster to get 70 per cent of Canada’s population fully inoculated by Dec. 31.
That assumes everyone who is vaccinated will need two shots and that a small portion of the population, about four million, will either choose not to receive the vaccine or will be unable to. The calculation also takes into account that children are currently not approved to receive any COVID-19 vaccine.
Read the full story here: COVID-19 vaccination rate needs to ramp up dramatically to meet Trudeau’s September goal
4:01 a.m.: Quebecers out in the street after 8 p.m. tonight can expect to be questioned by police as a month-long curfew comes into effect to control the spread of COVID-19.
The province announced earlier this week that the curfew will be in place from 8 p.m. to 5 a.m., except for those who fall into certain exempted categories, such as essential workers.
Deputy Premier Genevieve Guilbault said earlier this week that the measure is designed to make it easier to catch people who are intent on gathering, in violation of current health orders.
She said in a tweet that the province will send out an emergency alert this afternoon to remind Quebecers of the curfew, and that police will be more visible on the streets over the weekend.
The curfew comes as Quebec’s COVID-19 cases and deaths continue to rise and hospitals say they’re filling up and risk becoming overwhelmed.
It will last at least four weeks, until Feb. 8, and violators could face fines ranging from $1,000 to $6,000.
Some public health experts have said they believe the curfew will help to reduce people’s contacts and send a message about the seriousness of the pandemic.
But others have questioned whether the measure will be effective, and have expressed concerns it will lead to excessive ticketing of people who are vulnerable or homeless.
Public health director Dr. Horacio Arruda said this week that while he can’t provide proof the curfew will work, it’s part of a series of measures aimed at reducing the possibility of gatherings and of contact between people. “There’s no science that can tell you what measure will have what percentage effect,” he told reporters.
Under the rules, grocery stores and convenience stores will have to close at 7:30 p.m. in order to allow workers and customers to get home. Stores connected to gas stations can stay open to serve essential workers.
The province has also shut down places of worship for all but small funerals, tightened mask-wearing rules for schools, and has extended the closure of non-essential businesses until at least Feb. 8.
Saturday 4:01 a.m.: The latest numbers on COVID-19 in Canada
The latest numbers of confirmed COVID-19 cases in Canada as of 4:00 a.m. ET on Saturday, Jan. 9, 2021.
There are 644,348 confirmed cases in Canada.
_ Canada: 644,348 confirmed cases (81,670 active, 545,971 resolved, 16,707 deaths).The total case count includes 13 confirmed cases among repatriated travellers.
There were 8,765 new cases Friday from 1,090,196 completed tests, for a positivity rate of 0.80 per cent. The rate of active cases is 217.27 per 100,000 people. Over the past seven days, there have been a total of 55,408 new cases. The seven-day rolling average of new cases is 7,915.
There were 129 new reported deaths Friday. Over the past seven days there have been a total of 966 new reported deaths. The seven-day rolling average of new reported deaths is 138. The seven-day rolling average of the death rate is 0.37 per 100,000 people. The overall death rate is 44.45 per 100,000 people.
There have been 15,420,760 tests completed.
_ Newfoundland and Labrador: 392 confirmed cases (12 active, 376 resolved, four deaths).
There were zero new cases Friday from 177 completed tests, for a positivity rate of 0.0 per cent. The rate of active cases is 2.3 per 100,000 people. Over the past seven days, there have been a total of two new cases. The seven-day rolling average of new cases is zero.
There have been no deaths reported over the past week. The overall death rate is 0.77 per 100,000 people.
There have been 74,281 tests completed.
_ Prince Edward Island: 102 confirmed cases (eight active, 94 resolved, zero deaths).
There were zero new cases Friday from 539 completed tests, for a positivity rate of 0.0 per cent. The rate of active cases is 5.1 per 100,000 people. Over the past seven days, there have been a total of six new cases. The seven-day rolling average of new cases is one.
There have been no deaths reported over the past week. The overall death rate is zero per 100,000 people.
There have been 82,541 tests completed.
_ Nova Scotia: 1,526 confirmed cases (29 active, 1,432 resolved, 65 deaths).
There were two new cases Friday from 926 completed tests, for a positivity rate of 0.22 per cent. The rate of active cases is 2.99 per 100,000 people. Over the past seven days, there have been a total of 29 new cases. The seven-day rolling average of new cases is four.
There have been no deaths reported over the past week. The overall death rate is 6.69 per 100,000 people.
There have been 185,396 tests completed.
_ New Brunswick: 735 confirmed cases (144 active, 582 resolved, nine deaths).
There were 18 new cases Friday from 985 completed tests, for a positivity rate of 1.8 per cent. The rate of active cases is 18.54 per 100,000 people. Over the past seven days, there have been a total of 134 new cases. The seven-day rolling average of new cases is 19.
There have been no deaths reported over the past week. The overall death rate is 1.16 per 100,000 people.
There have been 119,375 tests completed.
_ Quebec: 223,106 confirmed cases (24,563 active, 189,937 resolved, 8,606 deaths).
There were 2,588 new cases Friday from 1,009,991 completed tests, for a positivity rate of 0.26 per cent. The rate of active cases is 289.49 per 100,000 people. Over the past seven days, there have been a total of 17,657 new cases. The seven-day rolling average of new cases is 2,522.
There were 45 new reported deaths Friday. Over the past seven days there have been a total of 295 new reported deaths. The seven-day rolling average of new reported deaths is 42. The seven-day rolling average of the death rate is 0.5 per 100,000 people. The overall death rate is 101.43 per 100,000 people.
There have been 3,575,548 tests completed.
_ Ontario: 208,394 confirmed cases (28,203 active, 175,309 resolved, 4,882 deaths).
There were 3,799 new cases Friday from 69,144 completed tests, for a positivity rate of 5.5 per cent. The rate of active cases is 193.61 per 100,000 people. Over the past seven days, there have been a total of 23,759 new cases. The seven-day rolling average of new cases is 3,394.
There were 26 new reported deaths Friday. Over the past seven days there have been a total of 301 new reported deaths. The seven-day rolling average of new reported deaths is 43. The seven-day rolling average of the death rate is 0.3 per 100,000 people. The overall death rate is 33.52 per 100,000 people.
There have been 8,092,822 tests completed.
_ Manitoba: 25,963 confirmed cases (4,582 active, 20,655 resolved, 726 deaths).
There were 222 new cases Friday from 2,279 completed tests, for a positivity rate of 9.7 per cent. The rate of active cases is 334.58 per 100,000 people. Over the past seven days, there have been a total of 1,263 new cases. The seven-day rolling average of new cases is 180.
There were nine new reported deaths Friday. Over the past seven days there have been a total of 59 new reported deaths. The seven-day rolling average of new reported deaths is eight. The seven-day rolling average of the death rate is 0.62 per 100,000 people. The overall death rate is 53.01 per 100,000 people.
There have been 424,107 tests completed.
_ Saskatchewan: 17,474 confirmed cases (3,053 active, 14,237 resolved, 184 deaths).
There were 336 new cases Friday from 1,417 completed tests, for a positivity rate of 24 per cent. The rate of active cases is 259.95 per 100,000 people. Over the past seven days, there have been a total of 1,839 new cases. The seven-day rolling average of new cases is 263.
Loading…
Loading…Loading…Loading…Loading…Loading…
There were seven new reported deaths Friday. Over the past seven days there have been a total of 29 new reported deaths. The seven-day rolling average of new reported deaths is four. The seven-day rolling average of the death rate is 0.35 per 100,000 people. The overall death rate is 15.67 per 100,000 people.
There have been 310,516 tests completed.
_ Alberta: 109,652 confirmed cases (13,628 active, 94,783 resolved, 1,241 deaths).
There were 1,183 new cases Friday. The rate of active cases is 311.76 per 100,000 people. Over the past seven days, there have been a total of 6,637 new cases. The seven-day rolling average of new cases is 948.
There were 24 new reported deaths Friday. Over the past seven days there have been a total of 195 new reported deaths. The seven-day rolling average of new reported deaths is 28. The seven-day rolling average of the death rate is 0.64 per 100,000 people. The overall death rate is 28.39 per 100,000 people.
There have been 1,547,298 tests completed.
_ British Columbia: 56,632 confirmed cases (7,439 active, 48,205 resolved, 988 deaths).
There were 617 new cases Friday from 4,488 completed tests, for a positivity rate of 14 per cent. The rate of active cases is 146.69 per 100,000 people. Over the past seven days, there have been a total of 4,077 new cases. The seven-day rolling average of new cases is 582.
There were 18 new reported deaths Friday. Over the past seven days there have been a total of 87 new reported deaths. The seven-day rolling average of new reported deaths is 12. The seven-day rolling average of the death rate is 0.25 per 100,000 people. The overall death rate is 19.48 per 100,000 people.
There have been 988,684 tests completed.
_ Yukon: 69 confirmed cases (nine active, 59 resolved, one deaths).
There were zero new cases Friday from 22 completed tests, for a positivity rate of 0.0 per cent. The rate of active cases is 22.03 per 100,000 people. Over the past seven days, there have been a total of five new cases. The seven-day rolling average of new cases is one.
There have been no deaths reported over the past week. The overall death rate is 2.45 per 100,000 people.
There have been 6,079 tests completed.
_ Northwest Territories: 24 confirmed cases (zero active, 24 resolved, zero deaths).
There were zero new cases Friday from 23 completed tests, for a positivity rate of 0.0 per cent. Over the past seven days, there have been a total of zero new cases. The seven-day rolling average of new cases is zero.
There have been no deaths reported over the past week. The overall death rate is zero per 100,000 people.
There have been 8,083 tests completed.
_ Nunavut: 266 confirmed cases (zero active, 265 resolved, one deaths).
There were zero new cases Friday from 205 completed tests, for a positivity rate of 0.0 per cent. Over the past seven days, there have been a total of zero new cases. The seven-day rolling average of new cases is zero.
There have been no deaths reported over the past week. The overall death rate is 2.58 per 100,000 people.
There have been 5,954 tests completed.
This report was automatically generated by The Canadian Press Digital Data Desk and was first published Jan. 9, 2021.
Friday 11:55 p.m.: Canada’s first case of a new, more infectious variant of COVID-19 that surfaced in South Africa was found in Alberta on Friday, the same day two Atlantic provinces tightened their boundaries and Ontario warned tough new measures may be on the way if surging infection rates aren’t reined in.
Alberta’s chief medical health officer made the announcement about the new variant in a tweet late Friday afternoon. Dr. Deena Hinshaw said the person is believed to have contracted the illness while travelling and is in quarantine.
“There’s no evidence at this time that the virus has spread to others,” Hinshaw said.
“I know any new case is concerning, but we are actively monitoring for these variants and working to protect the public’s health.”
Late Friday, the Public Health Agency of Canada said that it had been in contact with Alberta and the province had confirmed “the first reported case of the South African variant in Canada.”
Federal officials said earlier in the day that the new variant had yet to be detected in the country.
The South African variant, 501. V2, is more infectious than the original COVID-19 virus and has rapidly become dominant in that country’s coastal areas. There have also been concerns among experts in the United Kingdom that vaccines may not be effective against it.
Fourteen cases of a more contagious COVD-19 variant that first surfaced in the U.K. have already been detected in Canada. Six of those were in Ontario, four were in Alberta, three were in British Columbia and one was in Quebec.
The news came as it was announced that, starting Saturday at 8 a.m., people entering Nova Scotia from New Brunswick will be required to isolate for two weeks.
“What we’re saying here is, ‘Do not go to New Brunswick, and New Brunswickers, do not come here, unless it is for essential purposes,'” said Nova Scotia Premier Stephen McNeil.
New Brunswick announced it would prohibit all non-essential travel into the province.
“It’s that constant movement of people between cities, provinces, countries that has enabled COVID-19 to spread to every corner of the globe,” said chief medical officer of health Dr. Jennifer Russell.
Nova Scotia reported two new cases, while New Brunswick had 18.
Meanwhile, the Manitoba government extended its COVID-19 restrictions, which were to expire Friday at midnight, for another two weeks to keep the demand on hospitals in check.
Since mid-November, restaurants and bars have been limited to takeout and delivery, and non-essential stores have shuttered except for curbside pickup. Public gatherings have been limited to five people and most social gatherings inside homes are forbidden.
The Prairie province reported 221 new COVID-19 cases Friday and nine additional deaths.
B.C. reported 617 new cases and 18 more deaths, bringing the total number of COVID-19 fatalities in the province to 988.
Ontario reported 4,249 new cases, still a record-breaking figure factoring in 450 earlier infections which were delayed in the tally. The province had 26 more deaths.
“If these basic measures continue to be ignored, the consequences will be more dire,” Premier Doug Ford warned. “The shutdown won’t end at the end of January. And we will have to look at more extreme measures.”
He did not provide further details on the nature or timing of any added restrictions.
Ford has warned in recent days that the province is going to run out of vaccine if it does not receive another shipment soon. Federal Conservative health critic Michelle Rempel Garner said in a statement that the Liberal government has had months to take a leadership role.
But Prime Minister Justin Trudeau expressed confidence that Canada will have enough vaccine by the fall for everyone who wishes to be inoculated.
Trudeau said he and Canada’s premiers discussed the vaccine rollout Thursday during a conference call.
“We agreed that it is vital that we work together as Team Canada to get vaccines delivered, distributed and administered as quickly and efficiently as possible.”
Trudeau said more than 124,000 doses of the Pfizer-BioNTech vaccine were delivered to 68 sites across the country this week, and 208,000 more are to be delivered weekly for the rest of this month.
And, by the end of next week, more than 171,000 Moderna vaccine doses are expected to be delivered to provinces and territories.
In all, Trudeau said, Ottawa is on track to deliver about 1.3 million doses of both vaccines by the end of January, with quantities scaling up in February.
Those in charge of Canada’s vaccine portfolio and the delivery schedule are confident that vaccines will be offered to all Canadians by September, he said.
“That will be significant in terms of getting through this pandemic and making sure that next winter looks very different from this one.”
Read about Friday’s updates here.
Health
Outdated cancer screening guidelines jeopardizing early detection, doctors say – Winnipeg Free Press
A group of doctors say Canadian cancer screening guidelines set by a national task force are out-of-date and putting people at risk because their cancers aren’t detected early enough.
“I’m faced with treating too many patients dying of prostate cancer on a daily basis due to delayed diagnosis,” Dr. Fred Saad, a urological oncologist and director of prostate cancer research at the Montreal Cancer Institute, said at a news conference in Ottawa on Monday.
The Canadian Task Force on Preventive Health Care, established by the Public Health Agency of Canada, sets clinical guidelines to help family doctors and nurse practitioners decide whether and when to recommend screening and other prevention and early detection health-care measures to their patients.
Its members include primary-care physicians and nurse practitioners, as well as specialists, a spokesperson for the task force said in an email Monday.
But Saad and other doctors associated with the Coalition for Responsible Healthcare Guidelines, which organized the news conference, said the task force’s screening guidelines for breast, prostate, lung and cervical cancer are largely based on older research and conflict with the opinions of specialists in those areas.
For example, the task force recommends against wide use of the prostate specific antigen test, commonly known as a PSA test, for men who haven’t already had prostate cancer. Saad called that advice, which dates back to 2014, “outdated” and “overly simplistic.”
The task force’s recommendation is based on the harms of getting false positive results that lead to unnecessary biopsies and treatment, he said.
But that reasoning falsely assumes that everyone who gets a positive PSA test will automatically get a biopsy, Saad said.
“We are way beyond the era of every abnormal screening test leading to a biopsy and every biopsy leading to treatment,” he said, noting that MRIs can be used to avoid some biopsies.
“Canadian men deserve (to) have the right to decide what is important to them, and family physicians need to stop being confused by recommendations that go against logic and evidence.”
Dr. Martin Yaffe, co-director of the Imaging Research Program at the Ontario Institute for Cancer Research, raised similar concerns about the task force’s breast cancer screening guideline, which doesn’t endorse mammograms for women younger than 50.
That’s despite the fact that the U.S. task force says women 40 and older may decide to get one after discussing the risks and benefits with their primary-care provider.
The Canadian task force is due to update its guidance on breast cancer screening in the coming months, but Yaffe said he’s still concerned.
“The task force leadership demonstrates a strong bias against earlier detection of disease,” he said.
Like Saad, Yaffe believes it puts too much emphasis on the potential harm of false positive results.
“It’s very hard for us and for patients to balance this idea of being called back and being anxious transiently for a few days while things are sorted out, compared to the chance of having cancer go undetected and you end up either dying from it or being treated for very advanced disease.”
But Dr. Eddy Lang, a member of the task force, said the harms of false positives should not be underestimated.
“We’ve certainly recommended in favour of screening when the benefits clearly outweigh the harms,” said Lang, who is an emergency physician and a professor at the University of Calgary’s medical school.
“But we’re cautious and balanced and want to make sure that we consider all perspectives.”
For example, some men get prostate cancer that doesn’t progress, Lang said, but if they undergo treatments they face risks including possible urinary incontinence and erectile dysfunction.
Lang also said the task force monitors research “all the time for important studies that will change our recommendations.”
“And if one of them comes along, we prioritize the updating of that particular guideline,” he said.
The Canadian Cancer Society pulled its endorsement from the task force’s website in December 2022, saying it hadn’t acted quickly enough to review and update its breast cancer screening guidelines to consider including women between 40 and 50.
“(The Canadian Cancer Society) believes there is an obligation to ensure guidelines are keeping pace with the changing environment and new research findings to ensure people in Canada are supported with preventative health care,” it said in an emailed statement Monday evening.
Some provinces have implemented more proactive early detection programs, including screening for breast cancer at younger ages, using human papillomavirus (HPV) testing to screen for cervical cancer and implementing CT scanning to screen for lung cancer, doctors with the Coalition for Responsible Healthcare Guidelines said.
But that leads to “piecemeal” screening systems and unequal access across the country, said Dr. Shushiela Appavoo, a radiologist with the University of Alberta.
Plus, many primary-care providers rely on the national task force guidelines in their discussions with patients, she said.
“The strongest association … with a woman actually going for her breast cancer screen is whether or not her doctor recommends it to her. So if her doctor is not recommending it to her, it doesn’t matter what the provincial guideline allows,” Appavoo said.
In addition to updating its guideline for breast cancer screening this spring, the task force is due to review its guidelines for cervical cancer screening in 2025 and for lung cancer and prostate cancer screening in 2026, according to its website.
This report by The Canadian Press was first published April 16, 2024.
Canadian Press health coverage receives support through a partnership with the Canadian Medical Association. CP is solely responsible for this content.
Health
Canada's opioid deaths double in 2 years, men in their 20s, 30s hit hardest – Surrey Now Leader

Opioid-related deaths doubled in Canada between 2019 and the end of 2021, with Manitoba, Saskatchewan and Alberta experiencing a dramatic jump, mostly among men in their 20s and 30s, says a new study that calls for targeted harm-reduction policies.
Researchers from the University of Toronto analyzed accidental opioid-related deaths between Jan. 1, 2019 and Dec. 31, 2021 in those provinces as well as British Columbia, Ontario, Quebec, New Brunswick and Nova Scotia, and the Northwest Territories.
Manitoba saw the sharpest rise in overdose deaths for those aged 30 to 39 – reaching 500 deaths per million population, more than five times the 89 deaths per million population recorded at the beginning of the study period.
In Saskatchewan, the death toll for that age group nearly tripled to 424 per million, up from 146 per million, while Alberta’s rate spiked more than 2.5 times to 729 fatalities per million, up from 272 per million. Ontario’s death rate reached 384, up from 210 per million.
British Columbia, which has been the epicentre of the overdose crisis, recorded 229 deaths per million for that age group in 2019, climbing to 394 in 2020. All data for 2021 from that province’s coroners service was not yet available when researchers completed their work based on information collected by the Public Health Agency of Canada.
Nationally, the annual number of opioid overdose deaths surged from 3,007 to 6,222 over the three-year study period, which researchers note coincided with pandemic public health measures that reduced access to harm reduction programs and imposed border restrictions that may have increased the toxicity of the drug supply.
“In addition, for many, the pandemic exacerbated feelings of anxiety, uncertainty, and loneliness, contributing to increased substance use globally,” they said.
The study was published Monday in the Canadian Medical Association Journal.
Senior author Tara Gomes said one in four deaths involved people in their 20s and 30s. More than 70 per cent of the overall deaths were among men.
A spokesman with the coroners service in British Columbia said 78 per cent of people that fatally overdosed in that province between 2019 and the end of 2021 were men.
The sharp surge in fatal overdoses – especially among young adults in the Prairies – suggests provinces must act quickly, said Gomes, an epidemiologist who called for more harm-reduction services including supervised consumption sites.
“Being slow and not being as nimble as we would like to be in our responses can have really devastating impacts,” said Gomes, also lead principal investigator of the Ontario Drug Policy Research Network.
Bernadette Smith, Manitoba’s minister of housing, addiction, homelessness and mental health, said the province plans to open its first supervised consumption site in Winnipeg next year and will also offer drug-testing machines so people can check if their illicit substances are toxic.
“We came out of a previous government that didn’t take a harm-reduction approach, unfortunately,” said the New Democrat, whose party defeated the Progressive Conservatives last fall.
“We’re working with front-line organizations because they have not been listened to or worked with for the last seven years in our province, which has been a real problem.”
Manitoba plans to train family doctors to treat addiction with medications including Suboxone and methadone, said Smith, noting the physicians typically refer patients to detox for care.
“We’re creating a model so that folks aren’t having to go to a bunch of different places to get different services,” said Smith.
She declined to say whether Manitobans will have access to a prescribed safer supply of drugs.
Tanya Hornbuckle of Edmonton said her son Joel Wolstenholme was 30 when he died in 2022. He became addicted to illicit substances at about age 14, starting with cannabis before shifting to methamphetamine, cocaine and other drugs that were increasingly laced with fentanyl.
He also battled a mental illness but getting help for both that issue and addiction in a single service was challenging, Hornbuckle said.
Wolstenholme tried multiple times to detox but there were never enough beds at a clinic where people had to line up at 8 a.m., she said.
“It would happen over and over and then he would call me. I went and stood in line or I drove him there and waited with him in the lineup. They wouldn’t have enough beds.”
Her son’s anxieties and addiction worsened when pandemic restrictions prevented her from entering an emergency room with him because he did not trust staff, Hornbuckle said.
On Feb. 6, 2022, Hornbuckle went to her son’s home so they could cook together. She found him dead.
The Alberta government’s strategy of focusing more on recovery and abstinence-based treatment than harm reduction, mental health and housing is the wrong approach, said Hornbuckle, noting that for a time her son slept in parks and abandoned houses after losing his vehicle and apartment to addiction.
Rebecca Haines-Saah, an associate professor of community health services at the University of Calgary, called the deaths of young people from overdose a tragedy, and said many more suffer from brain injury due to toxic substances.
“Obviously, we have the incorrect response. We do not have the approach and services available to keep people alive,” said Haines-Saah, who also called for more harm-reduction services.
“We don’t have a full-scale public health response that is required. We don’t have any plans to fund anything that relates to what we would call harm reduction.”
Much of the current approach to addiction excludes a large number of recreational drug users, said Gomes. She said between a third and half of the deaths in Ontario involved people without an opioid use disorder diagnosis.
“So, focusing on (residential treatment) alone is something that really concerns me because we really need to make sure that we have different options for different people.”
READ ALSO: Stories from the overdose crisis’ front lines
READ ALSO: Make overdose education mandatory in B.C. schools amid drug emergency, advocates say
Health
Manitoba significantly impacted by opioid-related deaths at start of pandemic | CTV News – CTV News Winnipeg
A new study out of Ontario and posted in the Canadian Medical Association Journal is highlighting the significant increase in accidental opioid-related deaths in Canada leading into the COVID-19 pandemic, with Manitoba being one of the most impacted provinces in the country.
The research looked at opioid-related deaths between 2019 and 2021 in nine provinces and territories in Canada.
Across Canada, opioid-related deaths more than doubled from 2019 with 3,007, to 6,222 in 2021.
It also found the years of life lost per 100,000 people climbed from 3.5 years in 2019 to seven in 2021.
After dipping halfway through 2019, opioid-related deaths spiked dramatically through the first quarter of 2020 and spiked again in the third quarter of 2021.
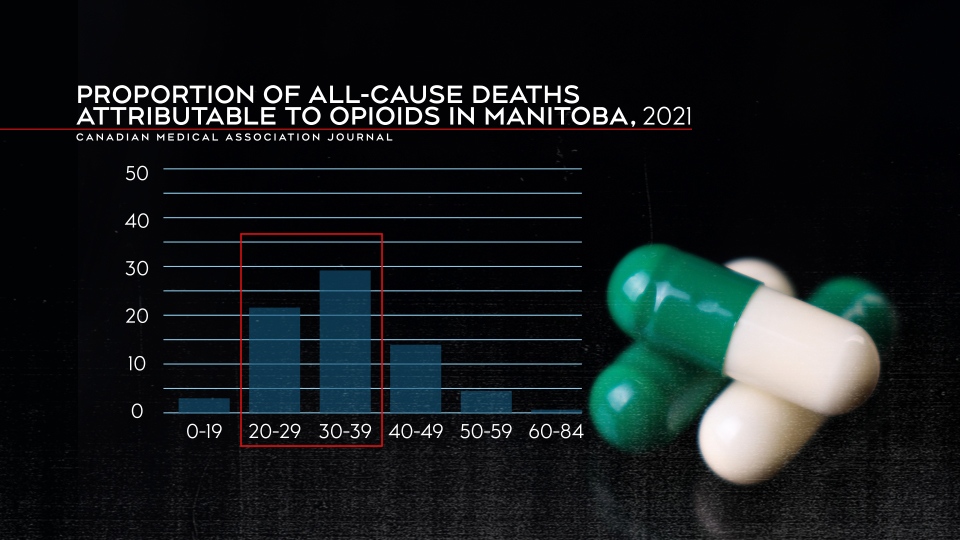
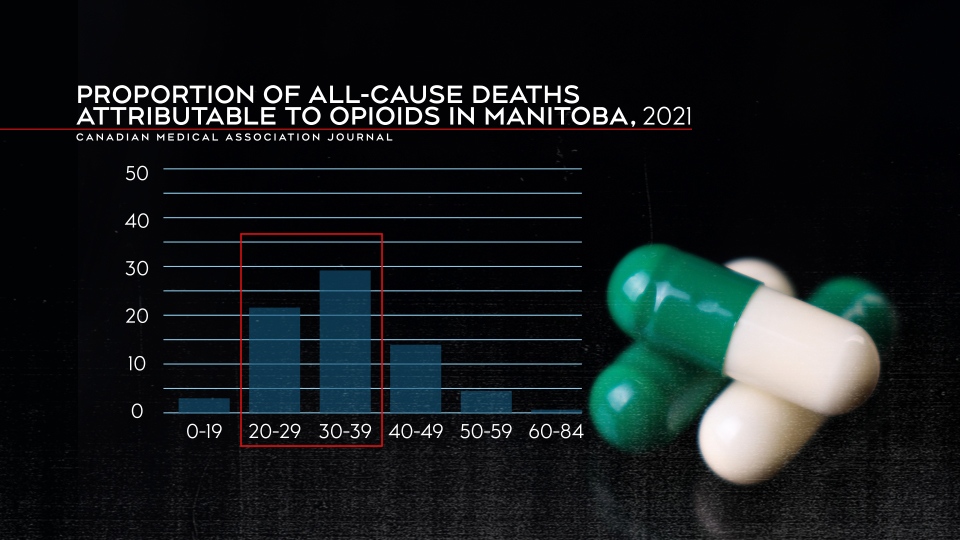
People in their 20s and 30s were most impacted by opioid deaths as they represented 29.3 per cent of all deaths in people aged 20 to 29 and 29 per cent of all deaths for people between 30 and 39.
“The disproportionate loss of life in this demographic group highlights the critical need for targeted prevention efforts,” the report said.
The data also showed men were much more likely to suffer an opioid-related death compared to women, with more than 4,500 deaths in 2021 compared to more than 1,600 women.
Manitoba one of the most impacted provinces by opioid-related deaths
Breaking down the provinces individually, the research found the Prairie provinces were impacted the most by opioid-related deaths.
Alberta and Saskatchewan both recorded fatality numbers that more than doubled between 2019 and 2021 – 619 deaths to 1,618 in Alberta and 109 to 322 deaths in Saskatchewan.
Meanwhile, Manitoba’s opioid-related deaths spiked nearly five-fold by 2021. There were 54 deaths in the province in 2019 and by the end of 2021, there were 263.
“In Manitoba, 70 per cent of opioid toxicity deaths in 2019 had fentanyl or fentanyl analogues detected, increasing to 86 per cent in 2020,” the report said.
Arlene Last-Kolb, a member of Moms Stop the Harm, lost her son Jessie to fentanyl drug poisoning in 2014.
She said the toxic drug supply is one of the main issues that needs to be addressed.
“We’re losing a whole generation of young people like my son,” Last-Kolb said. “It’s going to take a lot more than safe spaces and more treatment to address the toxic drug supply, including opiates, fentanyl that we have on our streets.”
Proportion of all-cause deaths attributable to opioids in Manitoba in 2021. (Canadian Medical Association Journal)
The years of life lost also jumped dramatically in Manitoba, going from 1.8 per 100,000 to 8.5 per 100,000 in 2021.
Those in the 30 to 39 age range were most impacted by opioid-related deaths in Manitoba. Almost 30 per cent of deaths in that age group were attributable to opioids.
Marion Willis, the founder and executive director of St. Boniface Street Links, called the numbers horrifying. She says something needs to be done as soon as possible.
“If that is not the strongest statement ever to support that we need a plan to address the drug crisis in this city, in this province – I don’t know what it takes,” said Willis.
She said plans for a new safe consumption site are a good first step, but agreed the drug supply also needs to be addressed.
“Safe consumption needs to include safer supply, or will we still have people using the same toxic drugs off the street.”
Bernadette Smith, the minister of housing, addictions and homelessness, said the province has a number of items on its agenda to help deal with the problem.
“That’s exactly what our government is doing. So supervised consumption site, drug testing machines, that’s our first step – getting those up and running,” said Smith.
However, Willis and Last-Kolb want to see action now.
“This is a challenge that is impacting all members of our human family. We’re all losing our loved ones, you know, from the wealthiest families to the poorest families. This is affecting everybody,” said Willis.
“It’s frustrating to talk about things that are going to happen down the road when somebody dies here every single day,” said Last-Kolb.
-
Media16 hours ago
Trump Media plunges amid plan to issue more shares. It's lost $7 billion in value since its peak. – CBS News
-
Media24 hours ago
Trump Media stock slides again to bring it nearly 60% below its peak as euphoria fades – National Post
-
Business24 hours ago
Tesla May Be Headed For Massive Layoffs As Woes Mount: Reports – InsideEVs
-



 Tech20 hours ago
Tech20 hours agoJava News Roundup: JobRunr 7.0, Introducing the Commonhaus Foundation, Payara Platform, Devnexus – InfoQ.com
-
Real eState20 hours ago
Real estate mogul concerned how Americans will deal with squatters: ‘Something really bad is going to happen’ – Fox Business
-



 Sports19 hours ago
Sports19 hours agoRafael Nadal confirms he’s ready for Barcelona: ‘I’m going to give my all’ – ATP Tour
-



 Sports24 hours ago
Sports24 hours agoPoints and payouts: Scottie Scheffler cements FedExCup top spot with Masters win, earns $3.6M – PGA TOUR – PGA TOUR
-
Science20 hours ago
Total solar eclipse: Continent watches in wonder – Yahoo News Canada






