Article content
Here is a roundup of stories from The Canadian Press designed to bring you up to speed on what you need to know today…
Tourism operators face heavy debt, even as business roars back
OTTAWA —
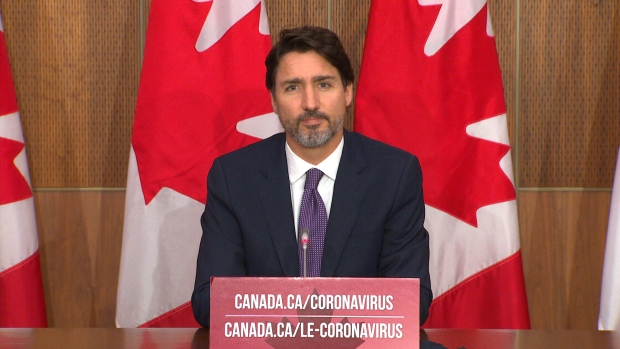
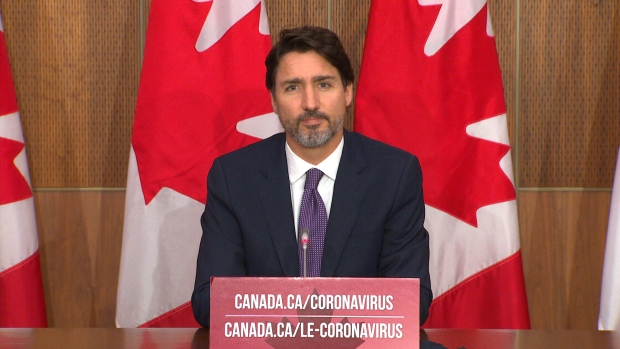
Prime Minister Justin Trudeau is trying to offer Canadians modest hope about progress in testing and vaccine development after Canada notched an all-time high of new COVID-19 cases in a day.
Trudeau told a news conference Friday that the government is spending $214 million towards the development of COVID-19 vaccines, signing deals with two Canadian biotech firms.
But even as he touted Canada’s portfolio of potential vaccines, Trudeau warned it’s unlikely that any of these candidates will be ready to distribute to Canadians this year or early next year. It’s reasonable to expect that vaccines will start to roll out at some point in 2021, said Trudeau, but even then, supply will be limited, and high-risk populations will be prioritized for inoculation.
“We are hopeful that the vaccines will arrive yesterday, but they won’t,” said Trudeau. “There’s still a number more months of work to do.”
Trudeau said his government signed a $173-million contract with Quebec’s Medicago to secure the rights to buy 76 million doses of its vaccine, should it meet health and safety standards. The funding will also be used to establish a production facility in Quebec City, he said.
Ottawa is also investing $18.2 million in a potential vaccine from British Columbia’s Precision NanoSystems. Meanwhile, the National Research Council is spending $23 million to support other Canadian vaccine initiatives, Trudeau said.
The prime minister said Canada has signed six agreements with a number of companies taking part in the global race to produce a safe and effective vaccine for COVID-19 .
Two more American vaccine makers, Moderna and Pfizer, have asked Health Canada to review their products, which are undergoing clinical trials.
The prime minister also said Canada has acquired “hundreds of thousands” of rapid test kits from medical company Abbott. Trudeau said his government has started distributing the kits to provinces and territories, and it will be up to those authorities to decide how to deploy them.
But new innovations and investments will only prove effective in the fight against the COVID-19 contagion if Canadians do their part to curb the spread, Trudeau said.
Canada’s chief public health officer told reporters Friday that a record 2,788 new illnesses were reported Thursday, bringing the country’s total count to just over 209,000 COVID-19 cases, including more than 9,800 deaths.
Dr. Theresa Tam said authorities need the public’s help to rein in infection rates through practices such as limiting in-person contacts, wearing masks and physical distancing.
Meanwhile, a Quebec health institute released projections Friday suggesting that province’s health system should have the capacity to handle the number of COVID-19 patients expected to need care in the next four weeks.
Quebec is reporting 905 new cases of COVID-19 and 12 more deaths from the illness.
Ontario also reported 826 new cases of COVID-19 on Friday, and nine new deaths linked to the virus.
Manitoba reported a total of 163 new infections Friday, most concentrated in Winnipeg, and the positivity rate is now up to 6.5 per cent. The province also said a man in his 80s is the latest death linked to an outbreak at Winnipeg’s Parkview Place that has killed a total of 15 people.
New Brunswick is reporting two new cases of COVID-19 in the Campbellton region, which is one of two areas that saw significant outbreaks two weeks ago.
Newfoundland and Labrador is asking passengers who travelled on Air Canada Flight 7484 from Toronto to Deer Lake on Oct. 12 to get tested in relation to a new COVID-19 case announced on Thursday.
This report by The Canadian Press was first published Oct. 23, 2020.


Here is a roundup of stories from The Canadian Press designed to bring you up to speed on what you need to know today…
Tourism operators face heavy debt, even as business roars back
Article content
Canadian tourism operators says the tourism sector hasn’t returned to what it was pre-COVID.
Many businesses report carrying a heavy debt load, with Vancouver-based ecotourism company Maple Leaf Adventures saying it’s carrying it’s heaviest debt load in 38 years.
Advertisement 2
Article content
Co-owner Maureen Gordon says while she and her competitors are recovering, higher interest rates are putting a damper on the post-COVID rebound.
Tourism Industry Association of Canada C-E-O Beth Potter says while the sector brought in 109-billion dollars in revenue last year, the federal government must help out by bringing in a new low interest loan program.
Tourism Minister Soraya Martinez Ferrada has said tourism operators have been affected by the warmest winter on record, but will be helped by the federal carbon rebate.
Here’s what else we’re watching …
Trudeau to make announcement in Saskatoon today
Prime Minister Justin Trudeau will be in Saskatoon today, where he will make an announcement highlighting measures focused on youth, education, and health that were contained in last week’s budget.
Joining Trudeau at the announcement in Saskatchewan’s largest city are minister for northern affairs Dan Vandal and Women and Gender Equality and Youth Minister Marci Ien.
Trudeau has faced conflict with the Saskatchewan Party government, whose leader, Premier Scott Moe, has been a vocal and long-standing opponent of the federal carbon levy.
Advertisement 3
Article content
Moe is one of several premiers who have asked Trudeau to host a meeting to discuss alternatives to the consumer carbon price.
—
‘Perfect storm’: Quebec farmer protests continue
Quebec farmers are continuing a series of protests that have brought slow rolling tractors to communities across the province’s agricultural regions.
The president of Quebec’s farmers union Martin Caron says producers are struggling with higher interest rates, growing paperwork and fees on plastic products, like containers of seeds, fertilizer and pesticides.
His organization is asking the current Coalition Avenir Quebec government to ensure farmers can get loans with interest rates of three per cent.
A spokesperson for Quebec’s agriculture minister says farmers can get emergency financial aid through a new program and that the government is consulting with the farmers union about reducing paperwork.
—
Study shows caribou growth at wolves’ expense
New research suggests western Canada’s caribou population is growing.
But the same study also shows the biggest reason for the rebound is the slaughter of hundreds of wolves, a policy which will likely need to continue.
Advertisement 4
Article content
Thirty-four researchers compared notes on herds in Alberta and British Columbia based on a study in Ecological Applications and found between 1991 and 2023, the caribou population dropped by half.
However, over the last few years the numbers have begun to slowly rise, as it’s estimated there are now more than 1500 caribou than there were had not restoration effort been made.
—
Second World War hangar in Edmonton burns in fire
An aircraft hangar built during the Second World War at Edmonton’s former municipal airport has been destroyed by fire.
A spokesman for the City of Edmonton says in an email firefighters were called to Hangar 11 just before 7 p.m. Monday.
The city’s email says 11 fire crews were dispatched to the scene to deal with the heavy smoke and flames and the wooden building later collapsed.
—
How a Newfoundland town shaped creepy ‘King Tide’
A new movie shot in Newfoundland showcases a community heavily reliant on a magical child.
“The King Tide” is about an isolated villagers having their lives forever changed after a mysterious infant washes up on their shores, the sole survivor of a devastating boat wreck.
They name the baby Isla, raise and learn she has healing powers promising immunity from injury and illness.
As the years pass, they become reliant on Isla’s abilities, but when her powers start to fade, a panic sets in as the community begins to fracture.
The movie was shot by Newfoundlander Christian Sparkes in Keels, Newfoundland, a former bustling fishing community which he says he’s been looking to film in for years, but couldn’t until recently due to the cost.
This report by The Canadian Press was first published April 23, 2024.
Article content
Canada’s plastic bag ban has had an unintended consequence: a proliferation of reusable bags piling up in basements, closets and, eventually, landfills.
“They’re everywhere,” said environmental researcher Tony Walker. “We’re drowning in them, and we shouldn’t be.”
To combat the problem, several of Canada’s big grocers have introduced solutions. Last week, Walmart launched a free national recycling pilot program for the retailer’s reusable blue bags. Competitors Sobeys and chains owned by Loblaw Companies Ltd. use recyclable paper bags for grocery delivery.
But some environmental experts argue that paper bags are also problematic and that the best solutions are those that help customers actually reuse their reusable bags.
“We just can’t keep giving [them] out,” said Walker, a professor at Dalhousie University’s School for Resource and Environmental Studies in Halifax. “We’re only meant to have a few of them, and we’re meant to use them until they fall apart.”
In late 2022, the federal government rolled out a ban on the manufacture, import and sale of several single-use plastics, including checkout bags. The regulations are being contested in court, but in the meantime, they remain in effect.


The regulations have made single-use shopping bags scarce in Canada, but they’ve also led to the proliferation of reusable bags, especially for grocery delivery.
“It just creates more waste, which is what we’re trying to avoid in the first place,” Walmart customer Udi Sela said in a CBC News interview in late 2022.
At the time, Sela, who lives in Maple, Ont., estimated his family had acquired about 300 reusable Walmart bags via grocery delivery.
“We can’t return them, we can’t do much with them.”
Now, a little more than a year later, Walmart has launched a pilot project to address the problem.
It allows customers to pack up their unwanted reusable Walmart blue bags and ship them — at no charge — to a facility where they’ll get a second life.
According to Walmart, bags in good condition will be laundered and donated to charity, primarily Food Banks Canada. Damaged bags will get recycled into other materials. Reusable bags typically can’t go in blue bins because they’re costly and difficult to recycle.
Customers must sign up for Walmart’s program, and enrolment is limited.
Jennifer Barbazza, Walmart’s senior manager of sustainability, said the retailer will fine-tune the details as the program progresses.
“[We] know that some customers have more reusable bags than maybe they need,” she said. “One of the things that we’re really excited to learn about from the pilot is customer acceptance and customer feedback.”
Reusable bags are living rent free in closets and car trunks across the country. Most major retailers made the switch away from single-use plastic bags about a year ago, but it’s taking time for some customers to catch on. They’re forgetting to bring their bags with them, and buying more every week.
Udi Sela has already signed up.
“I definitely think it’s a step in the right direction,” he said in an interview on Friday. “It’s something that needed to be done a while ago. God knows we’ve got a ton of bags kind of piled up.”
He said he’s concerned that some customers may find mailing the bags a hurdle. However, it’s not deterring Sela, who soon plans to ship hundreds.
Not everyone is keen on Walmart’s project. Emily Alfred, a waste campaigner with Toronto Environmental Alliance, said donating the bags to the food bank is just passing on the problem.
“We need to remove waste from the system entirely, and just sending these somewhere else for someone else to deal with is not really a solution,” she said.
Alfred said a better option is a program Walmart piloted in Guelph, Ont., in 2022. For a fee, customers could check out reusable bags from an in-store kiosk and later return them to be cleaned and reused.
“That’s a real circular reuse system,” she said.


Walmart’s Barbazza said the retailer is continuing to explore different reusable bag programs, including ones placed in stores.
She also said she’s confident Canada’s food banks will make good use of the bags.
“There’s definitely a need for sturdy items to distribute materials to the food bank clients.”
Among Canada’s major grocers, only Walmart offers a reusable bag program for all customers.
Loblaw recently switched from reusable to recyclable paper bags for grocery delivery. Sobeys did not respond to requests for comment, but according to its website, the grocer also uses paper bags and “reusable options” for home delivery.
Several environmental experts say paper bags aren’t a good solution, because their production leaves a sizable carbon footprint.
“Paper bags are a problem,” Alfred said. “It takes a lot of energy to recycle paper, takes a lot of trees and energy to make new paper.”
Loblaw said it continues to explore a variety of more sustainable solutions. “It’s a challenge we’re committed to addressing,” spokesperson Dave Bauer said in an email.


Both Walker and Alfred applaud Metro for its grocery delivery program, because the grocer, which operates in Ontario and Quebec, reuses delivery materials.
Metro said customers can get their goods delivered in a cardboard box or reusable bags, which can be returned and used for another delivery. Or customers can opt for a plastic bin and remove their groceries from it upon arrival.
Metro does not offer similar programs for in-store shoppers.
Alfred said the federal government should introduce regulations that mandate retailers adopt effective reusable bag programs for all customers.
“It’s up to our governments and people to demand that these companies do better,” she said.
But Walker suggested that the regulations would be hard to enforce and that incentives could be a better tactic.
For example, if retailers increased the price of reusable bags, shoppers might be less likely to forget them when they head to the store, he said.
“When the cost is a disincentive to do an activity, people change their behaviour.”
[unable to retrieve full-text content]
CTV National News: Honda’s big move in Canada CTV News





Source link
Honda to build electric vehicles and battery plant in Ontario, sources say – Global News




Will We Know if TRAPPIST-1e has Life? – Universe Today
Down 80%, Is Carnival Stock a Once-in-a-Generation Investment Opportunity?




See how chicken farmers are trying to stop the spread of bird flu – Fox 46 Charlotte




Simcoe-Muskoka health unit urges residents to get immunized




Own a cottage or investment property? Here's how to navigate the new capital gains tax changes – The Globe and Mail




Watch The World’s First Flying Canoe Take Off
Honda expected to announce multi-billion dollar deal to assemble EVs in Ontario
Comments