Health
What are the differences between Canada’s approved COVID-19 vaccines? Here’s what we know – Global News
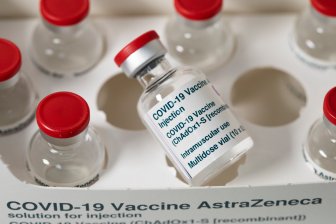
Now that the Oxford-AstraZeneca vaccine has been approved for use in Canada, three different jabs are on the menu for Canadians hoping to protect themselves against the coronavirus.
However, while all the vaccines have the same goal — to inoculate the recipient against COVID-19 — the vaccines are by no means identical.
And while Canada’s contracts secure enough doses from the three manufacturers to vaccinate everyone in the country by September, not everyone will be getting the same kind of jab.
Global News has broken down the key details of the three vaccines to help you understand which dose is going into your arm.
What kinds of COVID-19 vaccines are available?
- Pfizer: mRNA
- Moderna: mRNA
- AstraZeneca: adenovirus-based
All of these vaccines use fairly new vaccine technologies, but they don’t all use the same kind.
Pfizer and Moderna’s vaccines use mRNA technology, which delivers genetic instructions for our cells to make viral proteins themselves. The body then begins to train itself to fight these proteins, building its immunity to the same protein found in COVID-19.

The Oxford-AstraZeneca vaccine works differently. It was built using a kind of virus called an adenovirus, which causes colds in chimpanzees. These adenovirus-based vaccines represent a newly approved method of vaccination that has been studied for decades. The adenovirus is altered to carry a gene for the coronavirus protein, which can then train a person’s immune system to recognize the actual coronavirus if it ever enters the body.
How effective are the COVID-19 vaccines?
- Pfizer: 95 per cent
- Moderna: 94.1 per cent
- AstraZeneca: 62 per cent
Each of the vaccines has been found to be effective in combatting the coronavirus. However, they don’t all offer the same amount of protection.
Pfizer and Moderna have a photo-finish for first place in terms of effectiveness. Clinical trials found Pfizer’s vaccine was 95 per cent effective, while Moderna’s vaccine nipped at Pfizer’s heels with an effectiveness of 94.1 per cent.
The distant bronze goes to the Oxford-AstraZeneca vaccine, which was found to be 62 per cent effective in a two-dose clinical trial.

However, researchers accidentally gave a sub-group of participants a half-dose on their first jab of the Oxford-AstraZeneca jab, followed up by a full second dose. This group saw a leap in the vaccine’s ability to shield them from the virus, with the outcome proving to be 90 per cent effective.
[ Sign up for our Health IQ newsletter for the latest coronavirus updates ]
Because this was just a sub-group within the clinical trial, the vaccine was only approved for use in its full, two-dose iteration — which is over 30 per cent less effective than Pfizer and Moderna’s vaccines.
Still, at the end of the day, Canadians should feel confident that any one of the three approved vaccines will cut off COVID-19’s claws and protect them from the worst outcomes of the virus.
“If there is a vaccine and it’s been authorized by Health Canada, it means that it’s met standards,” said Dr. Supriya Sharma, chief medical advisor with the regulatory branch of Health Canada, said on Friday.
She explained that in clinical trials, all the vaccines were found to quash the worst outcomes in coronavirus patients.
“The number of cases of people that died from COVID-19 that got vaccine was zero. The number of people that were hospitalized because their COVID-19 disease was so severe was zero. The number of people that died because of an adverse event or an effect of the vaccine was zero,” Sharma said.
“So in the areas where we’re really looking to prevent serious illness, prevent hospitalizations and of course prevent death, all of these vaccines are good.”
How are the COVID-19 vaccines stored?
- Pfizer: -70°C
- Moderna: -25°C to -15°C
- AstraZeneca: 2°C to 8°C
Just like people, some of these vaccines are pickier than others about the temperature they like to hang around in.
Of the three vaccines, Pfizer is the most particular — and it likes things chilly. This vaccine requires ultra-cold storage, meaning it has to be transported and stored at -70 C. This makes the vaccine tricky to ship to remote regions, where the appropriate infrastructure is far more difficult to set up.

Enter the Moderna vaccine, which is a little less discerning. While this vaccine still likes the cold, it isn’t quite as particular as the Pfizer jab. The Moderna doses can be stored in a freezer between -25 C and -15 C. That’s why the territories have been guaranteed priority access to this particular vaccine, as it’s much easier to safely transport and store.
This category is also where AstraZeneca’s vaccine truly shines. The doses can be stored at normal fridge temperature — meaning the doses are much easier to both ship and keep.
How many doses of each COVID-19 vaccine are required?
- Pfizer: two
- Moderna: two
- AstraZeneca: two
Pfizer, Moderna and AstraZeneca’s vaccines are all two-dose shots — leaving little room for relief for those Canadians who get sweaty palms at the very thought of needles.
Some, including the head of Ontario’s vaccine rollout Gen. Rick Hillier, have pushed for Moderna to be approved as a single-dose vaccine, as the jab has proven to be about 80 per cent effective after the first injection.
However, no clinical trials have been conducted to prove whether that inoculation lasts long-term — and Moderna hasn’t shown any interest in conducting further trials to determine if less effective, one-time vaccine is a safe and effective option.
Who can take the COVID-19 vaccine?
- Pfizer: 16+
- Moderna: 18+
- AstraZeneca: 18+
While Canada is on track to have tens of millions of doses available to Canadians this year, not everyone who may want the vaccine will be able to take it.
Pfizer’s clinical trials were only conducted on those over the age of 16, which means that until further studies are completed in younger age groups, anyone under 16 years old is ineligible for the jab. The same issue comes into play for both Moderna and AstraZeneca, which only conducted their clinical trials on Canadians over the age of 18.

Moderna is currently conducting additional studies in children over 12 years old, so teens may be able to access the jabs once that work is done.
However, age isn’t the only limitation those hoping to be vaccinated may face. Anyone who is allergic to the ingredients in the vaccines is not allowed to receive the injections, and pregnant or breastfeeding mothers have been asked to consult their doctors before moving ahead with their vaccinations.
Finally, if you have COVID-19, you can’t get the vaccine until you’re better.
How many doses is Canada getting?
- Pfizer: 40 million doses
- Moderna: 40 million doses
- AstraZeneca: 20 million doses
Out of the three approved vaccines, individual Canadians are most likely to wind up receiving the Moderna vaccine. Canada’s agreement with Moderna is for 40 million doses — although the feds have the option of purchasing another 16 million in addition to that. The 40 million doses are enough to inoculate 20 million Canadians, over half of the population.
Meanwhile, Canada has 40 million Pfizer doses secured in its agreement with the manufacturer. That’s enough to inoculate another 20 million Canadians, which means that between Pfizer and Moderna alone, Canada has enough doses to vaccine every Canadian and then some.

As for the agreement with AstraZeneca, Canada has purchased 20 million doses — enough to vaccine another 10 million Canadians. That means that between the three agreements, Canada has enough doses to inoculate 40 million people, which is more than the entire population, within the year.
Should Canada opt to purchase more of any of the vaccines, there’s no guarantee they’d arrive any faster than the initial 80 million doses. Any additional doses would be entirely dependent on the manufacturer’s production capacity, which is under serious strain as every country battles to get the vaccines.
Either way, Canada’s current vaccine agreements point in an optimistic direction: every Canadian who wants a vaccine should be able to access one in 2021.
© 2021 Global News, a division of Corus Entertainment Inc.
Health
RCMP warn about benzodiazepine-laced fentanyl tied to overdose in Alberta – Edmonton Journal


Article content
Grande Prairie RCMP issued a warning Friday after it was revealed fentanyl linked to a deadly overdose was mixed with a chemical that doesn’t respond to naloxone treatment.
The drugs were initially seized on Feb. 28 after a fatal overdose, and this week, Health Canada reported back to Mounties that the fentanyl had been mixed with Bromazolam, which is a benzodiazepine.
Article content
Mounties say this is the first recorded instance of Bromazolam in Alberta. The drug has previously been linked to nine fatal overdoses in New Brunswick in 2022.
The pills seized in Alberta were oval-shaped and stamped with “20” and “SS,” though Mounties say it can come in other forms.
Naloxone treatment, given in many cases of opioid toxicity, is not effective in reversing the effects of Bromazalam, Mounties said, and therefore, any fentanyl mixed with the benzodiazepine “would see a reduced effectiveness of naloxone, requiring the use of additional doses and may still result in a fatality.”
From January to November of last year, there were 1,706 opioid-related deaths in Alberta, and 57 linked to benzodiazepine, up from 1,375 and 43, respectively, in 2022.
Mounties say officers responded to about 1,100 opioid-related calls for service, last year with a third of those proving fatal. RCMP officers also used naloxone 67 times while in the field, a jump of nearly a third over the previous year.
Recommended from Editorial
Share this article in your social network
Health
CFIA continues surveillance for HPAI in cattle, while sticking with original name for disease – RealAgriculture


The Canada Food Inspection Agency will continue to refer to highly pathogenic avian influenza in cattle as HPAI in cattle, and not refer to it as bovine influenza A virus (BIAV), as suggested by the American Association of Bovine Practitioners earlier this month.
Dr. Martin Appelt, senior director for the Canadian Food Inspection Agency, in the interview below, says at this time Canada will stick with “HPAI in cattle” when referencing the disease that’s been confirmed in dairy cattle in multiple states in the U.S.
The CFIA’s naming policy is consistent with the agency’s U.S. counterparts’, as the U.S. Animal and Plant Health Inspection Service has also said it will continue referring to it as HPAI or H5N1.
Appelt explains how the CFIA is learning from the U.S. experience to-date, and how it is working with veterinarians across Canada to stay vigilant for signs of the disease in dairy and beef cattle.
As of April 19, there has not been a confirmed case of HPAI in cattle in Canada. Appelt says it’s too soon to say if an eventual positive case will significantly restrict animal movement, as is the case with positive poultry cases.
This is a major concern for the cattle industry, as beef cattle especially move north and south across the U.S. border by the thousands. Appelt says that CFIA will address an infection in each species differently in conjunction with how the disease is spread and the threat to neighbouring farms or livestock.
Currently, provincial dairy organizations have advised producers to postpone any non-essential tours of dairy barns, as a precaution, in addition to other biosecurity measures to reduce the risk of cattle contracting HPAI.
Subscribe: Apple Podcasts | Spotify | RSS | All Podcasts
jQuery(document).ready(function($) {
$(“#homesub”).validate(
rules:
first_name:
required: true,
minlength: 2
,
last_name:
required: true,
minlength: 2
,
email:
required: true,
email: true,
minlength: 2
,
state:
required: true,
,
role:
required: true,
,
“listid[]”:
required: true,
minlength: 1
,
messages:
first_name: “Your first name is required.”,
last_name: “Your last name is required.”,
email: “Please verify your email is correct.”,
state: “Your state/province is required.”,
role: “Your role is required.”,
“listid[]”: “Select at least one list is required.”
,
submitHandler: function()
$.ajax(
type: “POST”,
url: “https://www.realagriculture.com/wp-admin/admin-ajax.php”,
data:
action: “realag_cc_process_subscribe_onclick”,
form: “homesub”,
data: $(“#homesub”).serialize(),
,
dataType: “html”,
timeout: 30000,
error: function(response)
console.log(response);
,
success: function(response)
$(“#homesub”).html(response);
,
);
);
});
Health
Toronto reports 2 more measles cases. Use our tool to check the spread in Canada – Toronto Star
/* OOVVUU Targeting */
const path = ‘/news/canada’;
const siteName = ‘thestar.com’;
let domain = ‘thestar.com’;
if (siteName === ‘thestar.com’)
domain = ‘thestar.com’;
else if (siteName === ‘niagarafallsreview.ca’)
domain = ‘niagara_falls_review’;
else if (siteName === ‘stcatharinesstandard.ca’)
domain = ‘st_catharines_standard’;
else if (siteName === ‘thepeterboroughexaminer.com’)
domain = ‘the_peterborough_examiner’;
else if (siteName === ‘therecord.com’)
domain = ‘the_record’;
else if (siteName === ‘thespec.com’)
domain = ‘the_spec’;
else if (siteName === ‘wellandtribune.ca’)
domain = ‘welland_tribune’;
else if (siteName === ‘bramptonguardian.com’)
domain = ‘brampton_guardian’;
else if (siteName === ‘caledonenterprise.com’)
domain = ‘caledon_enterprise’;
else if (siteName === ‘cambridgetimes.ca’)
domain = ‘cambridge_times’;
else if (siteName === ‘durhamregion.com’)
domain = ‘durham_region’;
else if (siteName === ‘guelphmercury.com’)
domain = ‘guelph_mercury’;
else if (siteName === ‘insidehalton.com’)
domain = ‘inside_halton’;
else if (siteName === ‘insideottawavalley.com’)
domain = ‘inside_ottawa_valley’;
else if (siteName === ‘mississauga.com’)
domain = ‘mississauga’;
else if (siteName === ‘muskokaregion.com’)
domain = ‘muskoka_region’;
else if (siteName === ‘newhamburgindependent.ca’)
domain = ‘new_hamburg_independent’;
else if (siteName === ‘niagarathisweek.com’)
domain = ‘niagara_this_week’;
else if (siteName === ‘northbaynipissing.com’)
domain = ‘north_bay_nipissing’;
else if (siteName === ‘northumberlandnews.com’)
domain = ‘northumberland_news’;
else if (siteName === ‘orangeville.com’)
domain = ‘orangeville’;
else if (siteName === ‘ourwindsor.ca’)
domain = ‘our_windsor’;
else if (siteName === ‘parrysound.com’)
domain = ‘parrysound’;
else if (siteName === ‘simcoe.com’)
domain = ‘simcoe’;
else if (siteName === ‘theifp.ca’)
domain = ‘the_ifp’;
else if (siteName === ‘waterloochronicle.ca’)
domain = ‘waterloo_chronicle’;
else if (siteName === ‘yorkregion.com’)
domain = ‘york_region’;
let sectionTag = ”;
try
if (domain === ‘thestar.com’ && path.indexOf(‘wires/’) = 0)
sectionTag = ‘/business’;
else if (path.indexOf(‘/autos’) >= 0)
sectionTag = ‘/autos’;
else if (path.indexOf(‘/entertainment’) >= 0)
sectionTag = ‘/entertainment’;
else if (path.indexOf(‘/life’) >= 0)
sectionTag = ‘/life’;
else if (path.indexOf(‘/news’) >= 0)
sectionTag = ‘/news’;
else if (path.indexOf(‘/politics’) >= 0)
sectionTag = ‘/politics’;
else if (path.indexOf(‘/sports’) >= 0)
sectionTag = ‘/sports’;
else if (path.indexOf(‘/opinion’) >= 0)
sectionTag = ‘/opinion’;
} catch (ex)
const descriptionUrl = ‘window.location.href’;
const vid = ‘mediainfo.reference_id’;
const cmsId = ‘2665777’;
let url = `https://pubads.g.doubleclick.net/gampad/ads?iu=/58580620/$domain/video/oovvuu$sectionTag&description_url=$descriptionUrl&vid=$vid&cmsid=$cmsId&tfcd=0&npa=0&sz=640×480&ad_rule=0&gdfp_req=1&output=vast&unviewed_position_start=1&env=vp&impl=s&correlator=`;
url = url.split(‘ ‘).join(”);
window.oovvuuReplacementAdServerURL = url;
Canada has seen a concerning rise in measles cases in the first months of 2024.
By the third week of March, the country had already recorded more than three times the number of cases as all of last year. Canada had just 12 cases of measles in 2023, up from three in 2022.
function buildUserSwitchAccountsForm()
var form = document.getElementById(‘user-local-logout-form-switch-accounts’);
if (form) return;
// build form with javascript since having a form element here breaks the payment modal.
var switchForm = document.createElement(‘form’);
switchForm.setAttribute(‘id’,’user-local-logout-form-switch-accounts’);
switchForm.setAttribute(‘method’,’post’);
switchForm.setAttribute(‘action’,’https://www.thestar.com/tncms/auth/logout/?return=https://www.thestar.com/users/login/?referer_url=https%3A%2F%2Fwww.thestar.com%2Fnews%2Fcanada%2Ftoronto-reports-2-more-measles-cases-use-our-tool-to-check-the-spread-in-canada%2Farticle_20aa7df4-e88f-11ee-8fad-8f8368d7ff53.html’);
switchForm.setAttribute(‘style’,’display:none;’);
var refUrl = document.createElement(‘input’); //input element, text
refUrl.setAttribute(‘type’,’hidden’);
refUrl.setAttribute(‘name’,’referer_url’);
refUrl.setAttribute(‘value’,’https://www.thestar.com/news/canada/toronto-reports-2-more-measles-cases-use-our-tool-to-check-the-spread-in-canada/article_20aa7df4-e88f-11ee-8fad-8f8368d7ff53.html’);
var submit = document.createElement(‘input’);
submit.setAttribute(‘type’,’submit’);
submit.setAttribute(‘name’,’logout’);
submit.setAttribute(‘value’,’Logout’);
switchForm.appendChild(refUrl);
switchForm.appendChild(submit);
document.getElementsByTagName(‘body’)[0].appendChild(switchForm);
function handleUserSwitchAccounts()
window.sessionStorage.removeItem(‘bd-viafoura-oidc’); // clear viafoura JWT token
// logout user before sending them to login page via return url
document.getElementById(‘user-local-logout-form-switch-accounts’).submit();
return false;
buildUserSwitchAccountsForm();
#ont-map-iframepadding:0;width:100%;border:0;overflow:hidden;
#ontario-cases-iframepadding:0;width:100%;border:0;overflow:hidden;
#province-table-iframepadding:0;width:100%;border:0;overflow:hidden;
console.log(‘=====> bRemoveLastParagraph: ‘,0);
-
Media18 hours ago
DJT Stock Rises. Trump Media CEO Alleges Potential Market Manipulation. – Barron's
-
Media20 hours ago
Trump Media alerts Nasdaq to potential market manipulation from 'naked' short selling of DJT stock – CNBC
-
Investment19 hours ago
Private equity gears up for potential National Football League investments – Financial Times
-
Real eState10 hours ago
Botched home sale costs Winnipeg man his right to sell real estate in Manitoba – CBC.ca
-
News17 hours ago
Canada Child Benefit payment on Friday | CTV News – CTV News Toronto
-



 Sports23 hours ago
Sports23 hours ago2024 Stanley Cup Playoffs 1st-round schedule – NHL.com
-
Business19 hours ago
Gas prices see 'largest single-day jump since early 2022': En-Pro International – Yahoo Canada Finance
-
Art22 hours ago
Enter the uncanny valley: New exhibition mixes AI and art photography – Euronews