Health
What social science says about convincing people to wear masks during the COVID-19 pandemic – CBC.ca
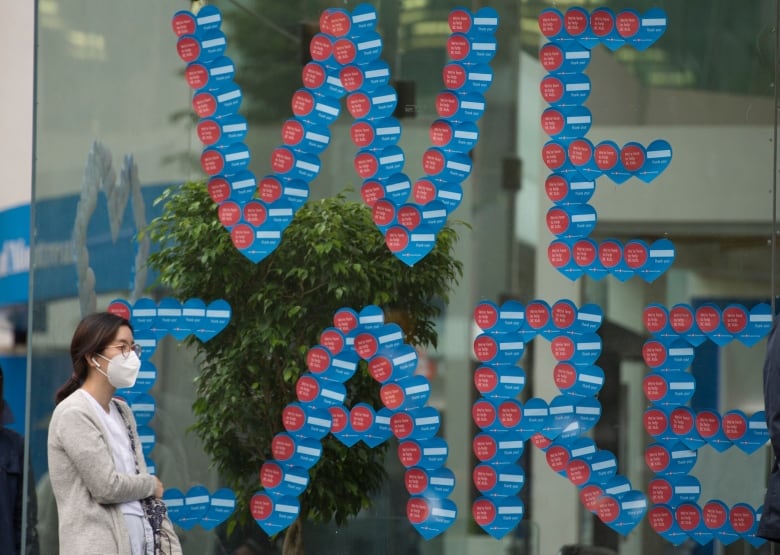
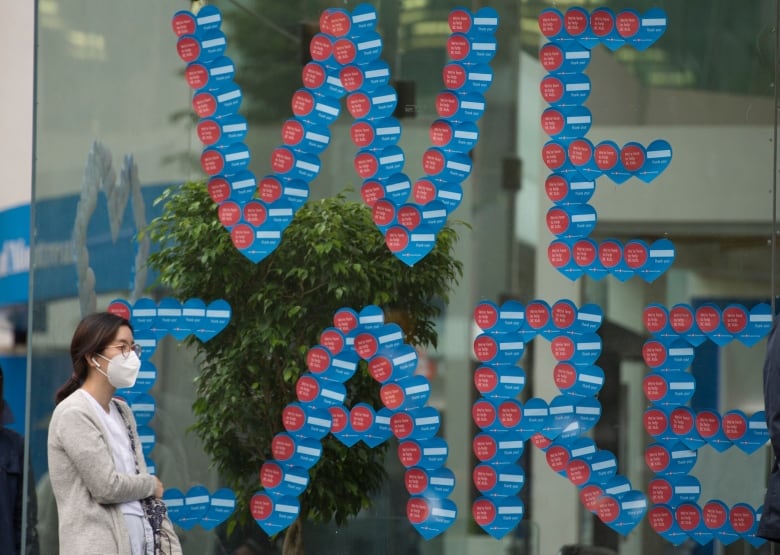
Mandating, not just recommending, the use of non-medical masks will help convince more Canadians to wear them as the economy reopens, just as wearing seatbelts is now the norm, some social scientists and physicians say.
In Canada’s largest city, wearing non-medical masks is now mandatory for people riding with the Toronto Transit Commission, with certain exemptions, to prevent the spread of the novel coronavirus. A bylaw extending the rule to indoor public spaces goes into effect on July 7. Similarly, mayors in Peel Region, which includes Mississauga and Brampton, west of Toronto, and York Region to the north also plan to introduce such bylaws.
In Quebec, Premier François Legault announced that public transit users in the province will be required to wear masks starting on July 13.
Governments are passing laws that require the wearing of masks, but they’re difficult to enforce. That’s why behavioural scientists say it’s so important for the public to get on board with many health authorities who now consider face coverings a necessity.
Kim Lavoie, a professor of psychology in behavioural medicine at the University of Quebec at Montreal, is among the experts calling for governments in Canada to consult social scientists on preventive measures like wearing masks as lockdowns lift in the absence of vaccines or effective treatments for COVID-19.
“Wearing a mask is something we control. Washing our hands, staying home, skipping that party are all things we control,” Lavoie said.
“People forget that the virus isn’t more powerful than our collective will to get rid of it, and there are things we can do. But right now, they’re behavioural.”
Dr. David Fisman, an epidemiologist at the University of Toronto’s Dalla Lana School of Public Health, said masks could help more people get back to business and “regular life.”
“We think it’s sort of low-hanging fruit and a no-brainer,” Fisman said.
Why? Layering on masks on top of hand hygiene, avoiding touching your face and physical distancing helps reduce transmission in small case reports, observational studies and a preliminary model.
“Me wearing a mask protects you. If I have COVID, you wearing a mask also protects you from breathing in my virus,” Fisman said.
While Fisman called Canada “a country of rule followers,” there are people who oppose mandating masks, saying it impinges on individual rights and freedoms.
But with COVID-19, one person’s behaviour affects the next person — the basis for secondhand smoke laws.
“It’s no more [an infringement] than asking you to wear a seatbelt,” Lavoie said. “You’re not free to drink yourself under the table and then get behind the wheel. If you don’t have a PCR test at your house to test yourself negative, then you have to consider the possibility that you might be infected and not know it and be putting us all at risk.”
Protecting yourself a major motivator
Lavoie is one of the researchers behind a large study called iCARE (International assessment of COVID-19-related attitudes, concerns, responses and impacts). Together with collaborators from Johns Hopkins University’s project on cases and Oxford’s policy tracker, they’re regularly surveying Canadians and people around the world on how they feel about and adhere to policies.
The goal of the research is to disentangle what motivates people of different ages and socioeconomic backgrounds to change their behaviour to inform health-care policy and messaging.


Based on 50,000 responses since the end of March, Lavoie said the findings to this point suggest that concern about getting infected with the virus is a major motivator.
“One thing people don’t realize is how contagious it is,” she said.
Most people recover at home, but people of all ages have also been severely sickened, some for months, says the Public Health Agency of Canada. Patients say long-term symptoms and consequences such as heart damage are coming to the fore.
An urgent need
While making mask wearing the norm would help prevent transmission, Fisman said mixed messaging and “dithering” by Ontario’s government have hindered mask use from becoming commonplace.
“Once the signal comes from our public health leaders that this is the expectation and this is how we’re going to move forward, I think people will fall in line pretty fast,” he said.
Wearing masks could be considered a behaviour that needs to be adopted urgently and collectively, Lavoie said.
She pointed to how behavioural change boils down to three factors:
- Awareness of the need to wear masks.
- Motivation, such as protecting yourself, loved ones or neighbours who may be vulnerable to serious complications.
- Confidence in the ability to execute the behaviour.
Cost can be a barrier. That’s why Alberta’s government is distributing 20 million non-medical masks at drive-thru restaurants.
Shift from self-consciousness to the norm
Mitsutoshi Horii, a professor of sociology at Chaucer College in Canterbury, England, studied the uptake of masks in Japan during the 1918 flu pandemic. The practice continues in Japan during flu and hay fever season, as well as during COVID-19.
Horii said when the 1918 flu pandemic hit, the Japanese government prohibited traditional folk rituals around health as part of its efforts to promote modernization and to avoid colonization.
“Then the mask came in and that gave people a sense of direction. When you’re facing uncertainty, you want to do something. By doing something, we establish a sense of control,” he said.
WATCH | Canada’s patchwork of mask measures:
Horii contrasts that with his experience in the U.K. now, where wearing masks is not common.
“Personally, I still feel embarrassed to wear a mask” in the U.K., Horii said, even though they’re now compulsory on public transit in England and will soon be required in stores in Scotland.
He said he thinks changing the rules would encourage him and others to overcome self-consciousness.
“At the same time, I bought some masks and we’re ready to wear [them] at any time. We just need a bit of a push to do it.”
Health
Bird flu raises concern of WHO – ecns


The World Health Organization (WHO) said the rising number of bird flu cases has raised “great concern” because it had an “extremely high” mortality rate among those who had been infected around the world.
The WHO’s data show that from 2003 through March 2024, a total of 889 worldwide human cases of H5N1 infection had been recorded in 23 countries, resulting in 463 deaths and a 52 percent mortality rate. The majority of deaths occurred in Southeast Asian countries and Egypt.
The most recent death was in Vietnam in late March, when a 21-year-old male without underlying conditions died of the infection after bird hunting. So far, cases in Europe and the United States have been mild.
Jeremy Farrar, chief scientist at the WHO, said recently that H5N1, predominantly started in poultry and ducks, “has spread effectively over the course of the last one or two years to become a global zoonotic — animal — pandemic”.
He said that the great concern is that the virus is increasingly infecting mammals and then develops the ability to infect humans. It would become critical if the virus develops the ability to “go from human-to-human transmission”, Farrar said.
In the past month, health officials have detected H5N1 in cows and goats from 29 dairy herds across eight states in the US, saying it is an alarming development because those livestock weren’t considered susceptible to H5N1.
The development worries health experts and officials because humans regularly come into contact with livestock on farms. In the US, there are only two recorded cases of human infection — one in 2022 and one in April this year in Texas. Both infected individuals worked in close proximity to livestock, but their symptoms were mild.
Wenqing Zhang, head of the WHO’s global influenza program, told the Daily Mail that “bird-to-cow, cow-to-cow and cow-to-bird transmission have also been registered during these current outbreaks, which suggest that the virus may have found other routes of transition than we previously understood”.
Zhang said that multiple herds of cow infections in the US states meant “a further step of the virus spillover to mammals”.
The virus has been found in raw milk, but the Texas Health Services department has said the cattle infections don’t present a concern for the commercial milk supply, as dairies are required to destroy milk from sick cows. In addition, pasteurization also kills the virus.
Darin Detwiler, a former food safety adviser to the Food and Drug Administration and the US Agriculture Department, said that Americans should avoid rare meat and runny eggs while the outbreak in cattle is going on to avoid the possibility of infection from those foods.
Nevertheless, both the WHO and the Centers for Disease Control and Prevention (CDC) said that the risk the virus poses to the public is still low. Currently no human-to-human infection has been detected.
On the potential HN51 public health risk, Farrar cautioned that vaccine development was not “where we need to be”.
According to a report by Barron’s, under the current plan by the US Health and Human Services Department, if there is an H5N1 pandemic, the government would be able to supply a few hundred thousand doses within weeks, then 135 million within about four months.
People would need two doses of the shot to be fully protected. That means the US government would be able to inoculate about 68 million people — 20 percent — of 330 million in case of an outbreak.
The situation is being closely watched by scientists and health officials. Some experts said that a high mortality rate might not necessarily hold true in the event the virus became contagious among people.
“We may not see the level of mortality that we’re really concerned about,” Seema Lakdawala, a virologist at Emory University, told The New York Times. “Preexisting immunity to seasonal flu strains will provide some protection from severe disease.”
Agencies contributed to this story.
Health
Peel Region has major childhood vaccination backlog – CBC.ca


Peel Region has a massive childhood vaccination backlog, with more than half of children missing at least one mandated vaccine dose.
That’s the warning from Peel’s acting medical officer of health, who says the lack of school immunizations is spelling trouble for communicable diseases.
“Without significant dedicated resources, we estimate it will take seven years to complete screening catch up and achieve pre-pandemic coverage rates,” said Dr. Katherine Bingham in a presentation to Peel council on April 11.
She says low immunization coverage among students significantly increases the risk for the re-emergence of vaccine-preventable diseases such as measles.
Unless children have a valid exception, the following vaccines are mandatory for Ontario school children: diphtheria, tetanus, polio, measles, mumps, rubella, meningitis, whooping cough and chicken pox. Several other vaccines are strongly recommended by public health units and doctors.
Advocates, doctors and Peel public health are advocating for more attention to the issue, more money from the province for public health and the formation of an action plan to quickly address the currently low vaccination rates.
Peel stacks lower than the provincial average on a number of vaccinations. For example, just over 37 per cent of seven-year-olds had been vaccinated against measles compared to more than 52 per cent province-wide as of August 31, 2022.
Peel Public Health says many children missed vaccinations they would have received at school or a doctor’s offices. Reporting of vaccines and enforcement also fell behind in the pandemic. To tackle the backlog more quickly, Peel Public Health opened public clinics for mandatory vaccines as of April 1 of this year.
‘We never thought it would be us’: mother
Jill Promoli, a Mississauga mother, lost her son, Jude, to a school flu outbreak eight years ago even though he was vaccinated. She’s now an illness prevention advocate championing immunizations and said the low vaccination rates in Peel children are “very concerning.”
“We never thought it would be us, but it is going to be someone,” said Promoli, who’s also a Peel District School Board Trustee, but did not speak to CBC Toronto in that capacity.
“The reason that we do vaccinate against these diseases is not because they’re inconvenient or uncomfortable, but it’s because people do die from them,” she said.
Promoli says she’s also concerned about children who are vaccinated being exposed, given vaccines do not provide complete immunity.
Pediatric and infectious disease specialist, Dr. Anna Banerji, called the proportion of Peel students missing a mandated dose “very high.”
“It needs to be addressed,” she said.
She says part of the problem in the region is access, including to family doctors, but the region also has a diverse population, which can mean additional challenges.
“I think that language and cultural support and trying to get these kids vaccinated will be very important,” she said.
Banerji also pointed to vaccine hesitancy being higher for some coming out of the pandemic.
She says seven years is far too long to have school-aged children not protected against such concerning diseases.
Needs will only grow, says Caledon mayor
The public health unit says they have less money than several nearby health units to try and tackle the issue, receiving one of the lowest provincial per capita funding rates in the province.
For cost-shared programs, in Peel, public health was funded by the province at approximately $34 per capita in 2022, while Toronto and Hamilton each received $49 per capita, according to the health authority’s report.
Caledon Mayor Annette Groves says the funding needs to change now to address problems that will continue to climb for Peel Public Health.
“Peel is a growing region and there will be greater need for funding as our resident population increases,” she said in a statement.
Province says funding has been increasing
Asked why Peel Public Health gets fewer dollars per capita, Ministry of Health spokesperson Hannah Jensen didn’t dispute Toronto and Hamilton received more funding per capita.
“Since 2018, our government has increased our investment into Peel Public Health by nearly 20 per cent,” she said in a statement.
Jensen said that’s in addition to the $100 million the provincial government invested into public health units across the province to provide support throughout the COVID-19 pandemic.
The government has restored a funding model where the province pays 75 percent of cost sharing for public health units and municipalities including Peel pay 25 percent, she said, noting the province had been paying 70 per cent for some time, so this represented an increase.
The province also increased base funding by one per cent per year, over the next three years, starting this year for public health units and municipalities including Peel, she added.
Asked why Peel would still receive a lower per capita rate that some of its neighbours, the province did not respond directly.
She says the government is working closely with its partners to get children caught up on vaccines.


Promoli says the per capita discrepancy in funding between regions is “shocking” and diverse populations need more, not less.
“It’s always important to try to meet people where they are,” she said. “To hear those questions, to hear the reasons why people are hesitant or even refusing and to try to understand…and then find the best ways to help people make decisions that will best protect their families.”
Peel Public Health says it plans to return to council soon with more details about the challenges and its plans to address them.
Health
It's possible to rely on plant proteins without sacrificing training gains, new studies say – The Globe and Mail


At the 1936 Olympics in Berlin, a scientist named Paul Schenk surveyed the eating habits of top athletes from around the world. The Canadians reported plowing through more than 800 grams of meat per day on average; the Americans were downing more than two litres of milk daily.
While there have been plenty of changes in sports nutrition since then, the belief that meat and dairy are the best fuel for building muscle persists. These days, though, a growing number of athletes are interested in reducing or eliminating their reliance on animal proteins, for environmental, ethical or health reasons. A pair of new studies bolsters the case that it’s possible to rely on plant proteins without sacrificing training gains, as long as you pick your proteins carefully.
The standard objection to plant proteins is that they don’t have the right mix of essential amino acids needed to assemble new muscle fibres. Unlike animal proteins, most plant proteins are missing or low in at least one essential amino acid.
In particular, there’s one specific amino acid, leucine, that seems to play a special role in triggering the synthesis of new muscle. It’s particularly abundant in whey, one of the two proteins (along with casein) found in milk. That’s why whey protein is the powdered beverage of choice in gyms around the world, backed by decades of convincing research, which was often funded by the dairy industry.
But one of the reasons whey looks so good may be that we haven’t fully explored the alternatives. A 2018 study by Luc van Loon of the University of Maastricht in the Netherlands, for example, tested nine vegetable proteins including wheat, hemp, soy, brown rice, pea and corn. To their surprise, they found that corn protein contains 13.5 per cent leucine – even more than whey.
Based on that insight, van Loon decided to pit corn against milk in a direct test of muscle protein synthesis. Volunteers consumed 30 grams of one of the proteins; a series of blood tests and muscle biopsies were collected over the next five hours to determine how much of the ingested protein was being turned into new muscle fibres. The results, which appeared in the journal Amino Acids, were straightforward: Despite all the hype about whey, there was no discernible difference between them.
A second study, this one published in Medicine & Science in Sports & Exercise by a team led by Benjamin Wall of the University of Exeter in Britain, had similar findings. Instead of corn, it used a mix of 40 per cent pea, 40 per cent brown rice and 20 per cent canola proteins. Since different plants have different amino acids profiles, mixing complementary proteins has long been suggested as a way overcoming the deficiencies of any single plant protein. Sure enough, the protein blend triggered just as much new muscle synthesis as whey.
On the surface, the message from these studies is straightforward: Plant proteins are – or at least can be – as effective as even the best animal proteins for supporting muscle growth. There are a few caveats to consider, though. One is that the studies used isolated protein powders rather than whole foods. You would need nearly nine cobs of corn to get the 30 grams of protein used in van Loon’s study, compared to just three-and-a-half cups of milk.
Another is that plants are generally harder to digest, meaning that not all the amino acids will be usable. That may not be a problem for healthy young adults consuming 30 grams of protein at once, which is enough to trigger a near-maximal muscle response. But for older people, who tend to have blunted muscle-building responses to protein, or in situations where you’re getting a smaller dose of protein, the details of protein quality may become more important.
Of course, the effectiveness of plant proteins won’t be news to notable plant-based athletes such as ultrarunner Scott Jurek or basketball star Chris Paul – but it’s encouraging to see the science finally begin to catch up.
Alex Hutchinson is the author of Endure: Mind, Body, and the Curiously Elastic Limits of Human Performance. Follow him on Threads @sweat_science.
-
Business16 hours ago
Honda to build electric vehicles and battery plant in Ontario, sources say – Global News
-



 Science16 hours ago
Science16 hours agoWill We Know if TRAPPIST-1e has Life? – Universe Today
-
Investment20 hours ago
Down 80%, Is Carnival Stock a Once-in-a-Generation Investment Opportunity?
-



 Health13 hours ago
Health13 hours agoSee how chicken farmers are trying to stop the spread of bird flu – Fox 46 Charlotte
-



 Health16 hours ago
Health16 hours agoSimcoe-Muskoka health unit urges residents to get immunized
-



 Investment14 hours ago
Investment14 hours agoOwn a cottage or investment property? Here's how to navigate the new capital gains tax changes – The Globe and Mail
-



 Science22 hours ago
Science22 hours agoWatch The World’s First Flying Canoe Take Off
-
News21 hours ago
Honda expected to announce multi-billion dollar deal to assemble EVs in Ontario








