Health
Questions on cold virus and flu myths
|
|
Early sunsets and chilly temperatures signal a shift from the itchy, watery eyes and sneezing associated with pollen allergies to the runny noses and coughs of winter cold and flu season.
But just how long should these respiratory bugs last? And how long are you contagious? Here are some answers.
Probably not.
“What I see doing pediatric clinics is that once a child gets a cold-like illness, like a runny nose and cough, is that people presume that it will all be gone within a couple of days,” said Dr. Jonathan Gubbay, a medical microbiologist and pediatric infectious disease physician in Toronto.
That’s not exactly right.
“For most of us, it’s a seven-day thing and it’s gone,” said David Proud, a professor of physiology and pharmacology at the University of Calgary. “We whine and complain, but [the cold infection] is really self-limiting.”
Proud studies people infected with cold viruses as part of his research into how colds can trigger attacks of asthma and chronic obstructive pulmonary disease (COPD). He said that in a “tiny” percentage of people, colds can have side-effects such as otitis media, or middle ear infections, which can be worse in those with a tendency to sinusitis.
Gubbay said people are infectious for the first few days after symptoms start, particularly the period with a fever. Health guidelines generally recommend keeping kids home from school until the fever is gone for 24 hours.
“The old joke that we have is, you can take all the best available current medications to treat it and it’ll go away in a week. Or you can do nothing and it will go away in seven days,” Proud said.
The reason, Proud said, is there’s not much clinical trial evidence, which is the gold standard, to tell if over-the-counter cold medications help.

Even so, fever can be uncomfortable for children and adults and fever reducers can help, said Dr. Michelle Murti, a public health physician and Gubbay’s colleague at Public Health Ontario.
“Warm, hot liquid can help make the mucus less sticky and help it drain a little bit better,” Murti said. “That’s why having that steam or a nice hot water or hot tea can be a soothing thing.”
Murti added that honey can also help with coughs. One important caution: Children under the age of one shouldn’t have honey because of the risk of botulism.
Murti said adults don’t tend to get a fever with a cold. Now that flu season has begun in every province and territory, if an adult has a fever and cough that comes on suddenly, consider influenza.
At the end of December and early January, Murti said Canadians will probably see more flu, with a sudden onset of cough, fatigue, muscle aches and “feeling like you got run over by a truck.”
Health officials recommend flu vaccines. “That’s really the best prevention measure that we have,” she said.
Gubbay said lab testing for influenza isn’t recommended for patients outside of the hospital, because it takes days to get the results, which is too late to decide on giving patients antiviral medications.
O.K., you’re no longer going through boxes of tissues. But then the cough sets in … and keeps going.
“We have a physician here who has a chronic cough clinic precisely because … people don’t really understand, if you’ve never experienced it, how miserable it can make life,” said Proud, who also holds the Canada Research Chair in inflammatory airway diseases. “It’s actually quite irritating for people, to say the least, not to mention disruptive.”
No one knows why such coughs occur. “We think it may have something to do with [people’s] nerves and their sensitivity to various kinds of irritants, but that’s really not much more than an educated guess,” Proud said.
Gubbay suggested saltwater sprays or drops can help dry up the nose to prevent such coughs.
The good news is that after a couple of weeks of a prolonged cough, people generally aren’t infectious, because they’re not bringing up the same level of virus as earlier, Murti said.
Murti said concerning symptoms of a cough include:
- Coughing to the point where you can’t breathe.
- Throwing up from a cough.
- Difficulty with underlying respiratory conditions, such as asthma or COPD.
A prolonged, more severe, wheezing cough could be from whooping cough, also called pertussis, a bacterial infection.
Gubbay said respiratory illness in an infant, particularly in the first few months, is worth having checked out by a health-care practitioner. Ditto for a fever in an older child that’s lasted more than 48 hours, or if there are symptoms beyond a runny nose and cough. These include looking lethargic with low energy levels, breathing quickly or requiring a lot of effort to breathe.
Murti said cold viruses can last on your skin, including your hands, for a couple of hours after a cough or sneeze. That’s why it is important to wash your hands with soap and water often in the first five to seven days of a cold, and to use hand sanitizer.
Public health experts also recommend sneezing into the elbow of your sleeve instead of your hands.
Health
Whooping cough cases up slightly in N.L., as officials warn about risks to infants – CBC.ca

Newfoundland and Labrador’s top doctor is warning people to stay up to date on whooping cough vaccinations after a small increase in cases this year.
The province usually sees three to four cases of the disease annually. Up to 10 cases have been reported already since January, however, prompting the province’s chief medical officer to raise the issue publicly.
The increase “generally means there’s a little bit more circulating in the community than what’s presenting for care and testing,” Dr. Janice Fitzgerald said Tuesday.
While officials aren’t overly concerned about a future spike in cases, Fitzgerald said, higher infection rates place infants in particular at risk.
Children under the age of one aren’t yet old enough for the whooping cough vaccine and don’t have immunity to the disease, Fitzgerald said. Infections in small children can be more severe and lead to pneumonia, neurological issues and hospitalization.
Fitzgerald said parents, grandparents and caregivers should check to ensure their vaccinations are up to date.
Whooping cough, also known as pertussis, causes a persistent nagging cough that’s sometimes severe enough to cause vomiting. Vaccines for the disease are offered in early childhood, during high school and in adulthood. Booster shots should be given 10 years after the high school dose, Fitzgerald said.
“Immunity can wane over time,” she said. “Pertussis does circulate on a regular basis in our community.”
The small increase in cases isn’t yet ringing alarm bells for undervaccination within the general population, she added, noting the province still has a vaccination rate over 90 per cent.
Download our free CBC News app to sign up for push alerts for CBC Newfoundland and Labrador. Click here to visit our landing page.
Health
Supervised consumption sites urgently needed, says study – Sudbury.com

A study in the Canadian Medical Association Journal (CMAJ) said the opioid drug crisis has reached such a critical level that a public safety response is urgently required and that includes the need for expanded supervised consumption sites.
The report was published by the medical journal Monday and was authored by Shaleesa Ledlie, David N. Juurlink, Mina Tadrous, Muhammad Mamdani, J. Michael Paterson and Tara Gomes; physicians and scientists associated with the University of Toronto, Sunnybrook Research Institute and the Li Ka Shing Knowledge Institute at St. Michael’s Hospital.
“The drug toxicity crisis continues to accelerate across Canada, with rapid increases in opioid-related harms following the onset of the COVID-19 pandemic,” the authors wrote. “We sought to describe trends in the burden of opioid-related deaths across Canada throughout the pandemic, comparing these trends by province or territory, age and sex.”
The study determined that across Canada, the burden of premature opioid-related deaths doubled between 2019 and 2021, representing more than one-quarter of deaths among younger adults. The disproportionate loss of life in this demographic group highlights the critical need for targeted prevention efforts, said the study.
The researchers found that the death rate increased significantly as fentanyl was introduced to the mix of street drugs that individuals were using, in some cases, unknowingly.
The authors said this demonstrates the need for consumption sites, not only as overwatch as people with addictions consume their drugs, but also to make an effort to identify the substances and inform those people beforehand.
“The increased detection of fentanyl in opioid-related deaths in Canada highlights the need for expansion of harm-reduction programs, including improved access to drug-checking services, supervised consumption sites, and treatment for substance use disorders,” the authors wrote.
The study said a more intense public safety response is needed.
“Given the rapidly evolving nature of the drug toxicity crisis, a public safety response is urgently required and may include continued funding of safer opioid supply programs that were expanded beginning in March 2020, improved flexibility in take-home doses of opioid agonist treatment, and enhanced training for health care workers, harm reduction workers, and people who use drugs on appropriate responses to opioid toxicities involving polysubstance use.
In conclusion, the authors wrote that during the height of the COVID pandemic in 2020 and 2021, the burden of premature death from accidental opioid toxicities in Canada dramatically increased, especially in Alberta, Saskatchewan, and Manitoba.
“In 2021, more than 70 per cent of opioid-related deaths occurred among males and about 30 per cent occurred among people aged 30–39 years, representing one in every four deaths in this age group. The disproportionate rates of opioid-related deaths observed in these demographic groups highlight the critical need for the expansion of targeted harm reduction–based policies and programs across Canada,” said the study.
The full text of the report can be found online here.
Health
Business Plan Approved for Cancer Centre at NRGH – My Cowichan Valley Now


A business plan for a new BC Cancer Centre at Nanaimo Regional General Hospital has been approved by the province.
Health Minister Adrian Dix says the state-of-the-art cancer facility will benefit patients in Nanaimo and the surrounding region through the latest medical technology.
The facility will have 12 exam rooms, four consultation rooms and space for medical physicists and radiation therapists, medical imaging and radiation treatment of cancer patients.
The procurement process is underway, and construction is expected to begin in 2025 and be complete in 2028.
Upgrades to NRGH have also been approved, such as a new single-storey addition to the ambulatory care building and expanded pharmacy.
Dix says Nanaimo’s population is growing rapidly and aging, and stronger health services in the region, so people get the health care they need closer to home.
-
News20 hours ago
Loblaws Canada groceries: Shoppers slam store for green onions with roots chopped off — 'I wouldn't buy those' – Yahoo News Canada
-
News23 hours ago
Toronto airport gold heist: Police announce nine arrests – CP24
-
Investment19 hours ago
Saudi Arabia Highlights Investment Initiatives in Tourism at International Hospitality Investment Forum
-
Business19 hours ago
Rupture on TC Energy's NGTL gas pipeline sparks wildfire in Alberta – The Globe and Mail
-
Art19 hours ago
Squatters at Gordon Ramsay's Pub Have 'Left the Building' After Turning It Into an Art Café – PEOPLE
-



 Tech23 hours ago
Tech23 hours agoVenerable Video App Plex Emerges As FAST Favorite – Forbes
-



 Tech12 hours ago
Tech12 hours agoCytiva Showcases Single-Use Mixing System at INTERPHEX 2024 – BioPharm International
-


 Sports22 hours ago
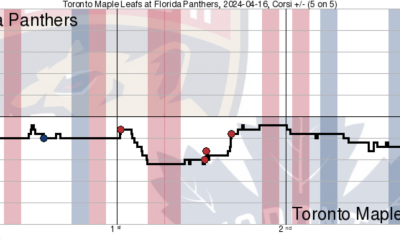
Sports22 hours agoGame in 10: Maple Leafs squander multi-goal lead to Florida, draw the Boston Bruins in the first round – Maple Leafs Hot Stove




