Read more:
‘Frustrating’ and ‘devastating’: The domino effect of family doctor, LTC shortages on ERs
Read More
It’s a well-known statistic that approximately 50 per cent of Canadians will be diagnosed with cancer in their lifetime. I knew there was a reasonable chance that it could happen to me.
What I didn’t know was that my time would come so soon.
In 2019, at the age of 36, I was diagnosed with Stage 3 invasive ductal carcinoma — a.k.a. locally advanced breast cancer.
Read more:
‘Frustrating’ and ‘devastating’: The domino effect of family doctor, LTC shortages on ERs
Read More
My children were one and three years old when I was blindsided with the diagnosis. I say blindsided because, up until the day my family doctor called to give me the results of my biopsy, everyone had assured me “it’s probably nothing. You’re too young to be diagnosed with cancer.”
Technically, they weren’t wrong: breast cancer in women under the age of 40 is rare. Only about seven per cent of those diagnosed with breast cancer have yet to clear their 30s.
Yet, there I was. Diagnosed with an aggressive cancer just as I was starting my young family, making strides in my career and crafting plans for the future. I didn’t have time for this inconvenient, life-threatening bomb that was suddenly dropped into my lap.
But that’s the thing about cancer — it doesn’t care how old you are. It doesn’t give a s**t about your plans or goals. And it doesn’t discriminate.
Immediately, I was thrown into a medical system that wasn’t designed for someone my age. There was no hospital daycare to help mind my children, I had to make immediate and distressing decisions about my fertility, hair and breasts, and the cancer support groups offered through my hospital were (by no fault of their own) definitely where I felt the loneliest as the youngest person in the room. It was depressing and isolating.
I remember being so desperate for someone I could relate to in the days after my diagnosis, I followed a young woman around the grocery store who had the telltale signs of losing her hair from chemo. Her head was freshly shaved and I could see little bald patches starting to appear in places. I never mustered up the courage to talk to her, but even being in her orbit for a short period of time made me feel a tiny bit better. Just knowing that someone else my age was going through the same thing was a salve.
Looking back, that behaviour seems a bit creepy, but it highlights how rare cancer is in young adults. I was receiving an avalanche of medical information and trying to process what was happening to my life, but I was most fixated on finding a friend who also had cancer — someone I could talk to, someone who would really understand.
Cancer in young adults is often diagnosed at later stages than those in older cohorts for a number of reasons. Young adults are typically healthy, meaning they might be less likely to visit a doctor until they really need to. Many young adults do not have a regular doctor. And when they do go see one, cancer is not high on the list of investigated diseases because cancer is not common in people under 40.
My diagnosis followed the latter pattern. It took a few months for anyone to consider that the lump in my breast was something other than blocked milk ducts from breastfeeding my son. I try not to dabble too much in the “what ifs” of my diagnosis, but I can’t help but wonder how long the cancer was growing inside me and if my life expectancy would be better had someone investigated earlier.
There was pressure to get me into a chemo chair as fast as possible, as my five-centimetre tumour was growing quickly thanks to an aggressive cancer subtype. The goal was to shrink the tumour with eight cycles of chemo before having surgery to remove the cancerous area and affected lymph nodes, and then blast it with daily radiation for six weeks.
Six months after finishing my initial treatments, coinciding with the beginning of the COVID-19 pandemic, I would be diagnosed with another form of breast cancer — an extremely rare type had existed alongside my original tumour but was undiagnosed, again, because the doctors thought I was “too young” for this particular type of cancer. I dodged the chemo chair on my second dance with the disease, luckily, but I was left with only one breast, heightened post-traumatic stress disorder, and a stronger feeling that my body, not to mention the Canadian medical system, had failed me.
The whole time I was being treated for cancer, I couldn’t wait to get to the “finish line,” the day that I finally crossed off all the chemo and surgeries, the 33 rounds of daily radiation, the weekly blood work, the scans, the additional five months of targeted therapy.
What I didn’t know was living with cancer in my body would be less distressing than living life as a cancer survivor. My hair grew back, signalling to the outside world that I was “better,” but that couldn’t be further from the truth. I will never fully shed this disease, no matter how long I remain in remission.
I recently came across a quote on Instagram that sums up my post-cancer life in the most heart-wrenching way: “Just because I’m living disease-free doesn’t mean I’m free of this disease.” There’s not a day that goes by that I don’t think about cancer, worry that it’s going to come back, try to quell intrusive thoughts that I might not live to grow old with my husband and watch our children grow up.
I have done my very best to be an advocate for young cancer patients, which, I have learned, is a double-edged sword. I want nothing more than to help other young breast cancer patients feel less alone. I lend my voice and time to a host of organizations and fundraisers, I create opportunities for young cancer survivors to connect, and I share openly and with vulnerability on social media.
When I was first diagnosed with breast cancer I happened to stumble across a group of other young women in my city who were going through the same ordeal. The “Pink Ladies” (now the Southern Alberta Breasties) would regularly meet for coffee, walks and chats, and they invited me into their cancer club with open arms.
That group provided, and continues to provide, a lifeline for me. A cancer diagnosis early in life is isolating, and the vast majority of my peers have never had to face their own mortality in such an abrupt way, nor deal with the aftermath of such a traumatic life event. The Breasties get it. They speak the language of cancer and know that part of my heart.
Over the past three years, our members have worked tirelessly to catch other young women coming into the cancer system, offering them a soft place to land surrounded by other people who have walked the same path. When I was welcomed into the group there were about 12 members. Now there are 200.
The founding member of the Breasties, a beautiful young woman by the name of Marloes, passed away from metastatic breast cancer last summer. I would visit with her often while she was dying, watching her eventually become deaf from the tumours growing in her brain. She never complained, never felt sorry for herself. She understood how precious her time on Earth was, and she milked every beautiful moment from it until she couldn’t anymore.
One of Marloes’ dying wishes was that the Breasties would continue on without her, that we would always continue to seek out other young women and make sure they had cancer survivors in their corner. She made me promise that the group would continue and I will never go back on that promise.
But making that promise means I’m now the unofficial go-to for the group. Every week there’s a newly diagnosed woman sliding into my direct messages, showing an agonizing amount of vulnerability while they desperately search for someone who understands and can help carry their pain.
This is my double-edged sword. It’s heartbreaking work and I relive my own diagnosis each time I learn of another woman who has this hideous disease. My therapist suggested that I back away from the role from time to time, and I do, but I never want any young woman to feel a fraction of the pain and fear I felt in the weeks after my diagnosis. While it’s extremely fulfilling to help others in this way, it’s a stark reminder that the cancer system is severely lacking in its setup to support those affected by a diagnosis at a young age.
My time in Cancerland, as I’ve been known to call it, has opened my eyes to the unique and frustrating challenges young adults face in the wake of cancer. I’ve shared my story many times, but it’s been a goal to create an in-depth series exploring some of these challenges.
The launch of this series coincides with the beginning of Breast Cancer Awareness month. To outsiders, it’s a sparkly and energetic month dedicated to what has somehow been framed as “the good type of cancer.” To many breast cancer survivors, it’s a stark reminder of a cancer that devastates families, disfigures bodies and steals too many good people. No kind of cancer is “fun,” and no kind of cancer is a “good” kind of cancer.
Against All Odds: Young Canadians & Cancer is an examination of the barriers young cancer patients deal with while accessing life-saving therapies and treatments. It’s also a look into the difficulties many young Canadians face following a cancer diagnosis: the impact on mental health, its effect on families and caretakers and the disappointing and disfiguring changes that often fall on undeserving people.
And while cancer is horrible, this series is also a celebration of those young people who are making the most of a bad situation. The people who fight back at their disease with humour and grace, as well as the organizations who are doing wonderful work to change the way young Canadians navigate cancer.
I would be remiss not to mention that I have always been cognizant and grateful for my own relative privilege. I am a white, cisgender woman who’s had the means and support to take as much time as I needed to recover and heal. I live in a major Canadian city, close to Calgary’s cancer centre and other medical facilities. I had access to unlimited therapy, a decent insurance plan and an amazing support system. For the most part, I received excellent care and my treatment (as far as I know) was successful.
Many people aren’t afforded the same, and with that in mind, we will hear from marginalized and racialized cancer patients and their families, as well as those who don’t live near major cancer hubs. Our series will speak to people across the country with different types of cancer, both men and women, at different stages.
Cancer is not a monolithic illness, but rather a series of separate and varying diseases that are often lumped together. Cancer, and the way it moves and multiplies in each body, is complex and unique. For this reason, no two cancer diagnoses are the same and every person deals with and manages their cancer diagnosis differently.
But there are common threads that almost all those who are diagnosed with cancer as a young adult can relate to: the fear and the unknown, the search for community and meaning in a diagnosis, the guilt in watching this disease take the lives of others, and trying to pick up the pieces of a life and fit them back together while living in a body that has betrayed you.
My hope is that this series shines a light on some of the systemic issues and barriers young adults face when dealing with a cancer diagnosis. I also hope this series highlights some of the Canadian organizations that are doing excellent work in the young adult cancer space.
But, ultimately, if even one person feels less alone after reading this series, then I consider it a success.
—
‘Against All Odds: Young Canadians & Cancer’ is a biweekly ongoing Global News series looking at the realities young adults face when they receive a cancer diagnosis.
Examining issues like institutional and familial support, medicine and accessibility, any roadblocks as well as positive developments in the space, the series shines a light on what it’s like to deal with the life-changing disease.

|
Give the gift of great skin this holiday season Skinstitut Holiday Gift Kits take the stress out of gifting Toronto, October 31, 2024 – Beauty gifts are at the top of holiday wish lists this year, and Laser Clinics Canada, a leader in advanced beauty treatments and skincare, is taking the pressure out of seasonal shopping. Today, Laser Clincs Canada announces the arrival of its 2024 Holiday Gift Kits, courtesy of Skinstitut, the exclusive skincare line of Laser Clinics Group. In time for the busy shopping season, the limited-edition Holiday Gifts Kits are available in Laser Clinics locations in the GTA and Ottawa. Clinics are conveniently located in popular shopping centers, including Hillcrest Mall, Square One, CF Sherway Gardens, Scarborough Town Centre, Rideau Centre, Union Station and CF Markville. These limited-edition Kits are available on a first come, first served basis. “These kits combine our best-selling products, bundled to address the most relevant skin concerns we’re seeing among our clients,” says Christina Ho, Senior Brand & LAM Manager at Laser Clinics Canada. “With several price points available, the kits offer excellent value and suit a variety of gift-giving needs, from those new to cosmeceuticals to those looking to level up their skincare routine. What’s more, these kits are priced with a savings of up to 33 per cent so gift givers can save during the holiday season. There are two kits to select from, each designed to address key skin concerns and each with a unique theme — Brightening Basics and Hydration Heroes. Brightening Basics is a mix of everyday essentials for glowing skin for all skin types. The bundle comes in a sleek pink, reusable case and includes three full-sized products: 200ml gentle cleanser, 50ml Moisture Defence (normal skin) and 30ml1% Hyaluronic Complex Serum. The Brightening Basics kit is available at $129, a saving of 33 per cent. Hydration Heroes is a mix of hydration essentials and active heroes that cater to a wide variety of clients. A perfect stocking stuffer, this bundle includes four deluxe products: Moisture 15 15 ml Defence for normal skin, 10 ml 1% Hyaluronic Complex Serum, 10 ml Retinol Serum and 50 ml Expert Squalane Cleansing Oil. The kit retails at $59. In addition to the 2024 Holiday Gifts Kits, gift givers can easily add a Laser Clinic Canada gift card to the mix. Offering flexibility, recipients can choose from a wide range of treatments offered by Laser Clinics Canada, or they can expand their collection of exclusive Skinstitut products.
|
||
|
Brightening Basics 2024 Holiday Gift Kit by Skinstitut, available exclusively at Laser Clincs Canada clinics and online at skinstitut.ca. |
||
|
Hydration Heroes 2024 Holiday Gift Kit by Skinstitut – available exclusively at Laser Clincs Canada clinics and online at skinstitut.ca. |

LONDON (AP) — Most people have accumulated a pile of data — selfies, emails, videos and more — on their social media and digital accounts over their lifetimes. What happens to it when we die?
It’s wise to draft a will spelling out who inherits your physical assets after you’re gone, but don’t forget to take care of your digital estate too. Friends and family might treasure files and posts you’ve left behind, but they could get lost in digital purgatory after you pass away unless you take some simple steps.
Here’s how you can prepare your digital life for your survivors:
Apple
The iPhone maker lets you nominate a “ legacy contact ” who can access your Apple account’s data after you die. The company says it’s a secure way to give trusted people access to photos, files and messages. To set it up you’ll need an Apple device with a fairly recent operating system — iPhones and iPads need iOS or iPadOS 15.2 and MacBooks needs macOS Monterey 12.1.
For iPhones, go to settings, tap Sign-in & Security and then Legacy Contact. You can name one or more people, and they don’t need an Apple ID or device.
You’ll have to share an access key with your contact. It can be a digital version sent electronically, or you can print a copy or save it as a screenshot or PDF.
Take note that there are some types of files you won’t be able to pass on — including digital rights-protected music, movies and passwords stored in Apple’s password manager. Legacy contacts can only access a deceased user’s account for three years before Apple deletes the account.
Google takes a different approach with its Inactive Account Manager, which allows you to share your data with someone if it notices that you’ve stopped using your account.
When setting it up, you need to decide how long Google should wait — from three to 18 months — before considering your account inactive. Once that time is up, Google can notify up to 10 people.
You can write a message informing them you’ve stopped using the account, and, optionally, include a link to download your data. You can choose what types of data they can access — including emails, photos, calendar entries and YouTube videos.
There’s also an option to automatically delete your account after three months of inactivity, so your contacts will have to download any data before that deadline.
Facebook and Instagram
Some social media platforms can preserve accounts for people who have died so that friends and family can honor their memories.
When users of Facebook or Instagram die, parent company Meta says it can memorialize the account if it gets a “valid request” from a friend or family member. Requests can be submitted through an online form.
The social media company strongly recommends Facebook users add a legacy contact to look after their memorial accounts. Legacy contacts can do things like respond to new friend requests and update pinned posts, but they can’t read private messages or remove or alter previous posts. You can only choose one person, who also has to have a Facebook account.
You can also ask Facebook or Instagram to delete a deceased user’s account if you’re a close family member or an executor. You’ll need to send in documents like a death certificate.
TikTok
The video-sharing platform says that if a user has died, people can submit a request to memorialize the account through the settings menu. Go to the Report a Problem section, then Account and profile, then Manage account, where you can report a deceased user.
Once an account has been memorialized, it will be labeled “Remembering.” No one will be able to log into the account, which prevents anyone from editing the profile or using the account to post new content or send messages.
X
It’s not possible to nominate a legacy contact on Elon Musk’s social media site. But family members or an authorized person can submit a request to deactivate a deceased user’s account.
Passwords
Besides the major online services, you’ll probably have dozens if not hundreds of other digital accounts that your survivors might need to access. You could just write all your login credentials down in a notebook and put it somewhere safe. But making a physical copy presents its own vulnerabilities. What if you lose track of it? What if someone finds it?
Instead, consider a password manager that has an emergency access feature. Password managers are digital vaults that you can use to store all your credentials. Some, like Keeper,Bitwarden and NordPass, allow users to nominate one or more trusted contacts who can access their keys in case of an emergency such as a death.
But there are a few catches: Those contacts also need to use the same password manager and you might have to pay for the service.
___
Is there a tech challenge you need help figuring out? Write to us at onetechtip@ap.org with your questions.

The Canadian Paediatric Society says doctors should regularly screen children for reading difficulties and dyslexia, calling low literacy a “serious public health concern” that can increase the risk of other problems including anxiety, low self-esteem and behavioural issues, with lifelong consequences.
New guidance issued Wednesday says family doctors, nurses, pediatricians and other medical professionals who care for school-aged kids are in a unique position to help struggling readers access educational and specialty supports, noting that identifying problems early couldhelp kids sooner — when it’s more effective — as well as reveal other possible learning or developmental issues.
The 10 recommendations include regular screening for kids aged four to seven, especially if they belong to groups at higher risk of low literacy, including newcomers to Canada, racialized Canadians and Indigenous Peoples. The society says this can be done in a two-to-three-minute office-based assessment.
Other tips encourage doctors to look for conditions often seen among poor readers such as attention-deficit hyperactivity disorder; to advocate for early literacy training for pediatric and family medicine residents; to liaise with schools on behalf of families seeking help; and to push provincial and territorial education ministries to integrate evidence-based phonics instruction into curriculums, starting in kindergarten.
Dr. Scott McLeod, one of the authors and chair of the society’s mental health and developmental disabilities committee, said a key goal is to catch kids who may be falling through the cracks and to better connect families to resources, including quicker targeted help from schools.
“Collaboration in this area is so key because we need to move away from the silos of: everything educational must exist within the educational portfolio,” McLeod said in an interview from Calgary, where he is a developmental pediatrician at Alberta Children’s Hospital.
“Reading, yes, it’s education, but it’s also health because we know that literacy impacts health. So I think that a statement like this opens the window to say: Yes, parents can come to their health-care provider to get advice, get recommendations, hopefully start a collaboration with school teachers.”
McLeod noted that pediatricians already look for signs of low literacy in young children by way of a commonly used tool known as the Rourke Baby Record, which offers a checklist of key topics, such as nutrition and developmental benchmarks, to cover in a well-child appointment.
But he said questions about reading could be “a standing item” in checkups and he hoped the society’s statement to medical professionals who care for children “enhances their confidence in being a strong advocate for the child” while spurring partnerships with others involved in a child’s life such as teachers and psychologists.
The guidance said pediatricians also play a key role in detecting and monitoring conditions that often coexist with difficulty reading such as attention-deficit hyperactivity disorder, but McLeod noted that getting such specific diagnoses typically involves a referral to a specialist, during which time a child continues to struggle.
He also acknowledged that some schools can be slow to act without a specific diagnosis from a specialist, and even then a child may end up on a wait list for school interventions.
“Evidence-based reading instruction shouldn’t have to wait for some of that access to specialized assessments to occur,” he said.
“My hope is that (by) having an existing statement or document written by the Canadian Paediatric Society … we’re able to skip a few steps or have some of the early interventions present,” he said.
McLeod added that obtaining specific assessments from medical specialists is “definitely beneficial and advantageous” to know where a child is at, “but having that sort of clear, thorough assessment shouldn’t be a barrier to intervention starting.”
McLeod said the society was partly spurred to act by 2022’s “Right to Read Inquiry Report” from the Ontario Human Rights Commission, which made 157 recommendations to address inequities related to reading instruction in that province.
He called the new guidelines “a big reminder” to pediatric providers, family doctors, school teachers and psychologists of the importance of literacy.
“Early identification of reading difficulty can truly change the trajectory of a child’s life.”
This report by The Canadian Press was first published Oct. 23, 2024.
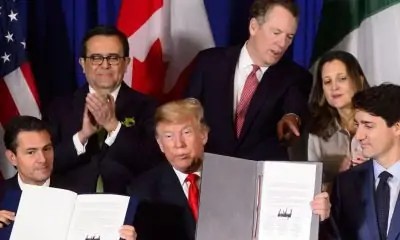

Freeland says she’s ready to deal with Trump |


NASA astronauts won’t say which one of them got sick after almost eight months in space


43 monkeys remain on the run from South Carolina lab. CEO thinks they’re having an adventure


Freeland rallies a united front ahead of Trump’s return to White House


Deputy minister appointed interim CEO of AIMCo after Alberta government fires board


Montreal says Quebec-Canada dispute stalling much-needed funding to help homeless


S&P/TSX composite index down Friday, Wall St. extends post-election gains


Mitch Marner powers Matthews-less Maple Leafs over Red Wings