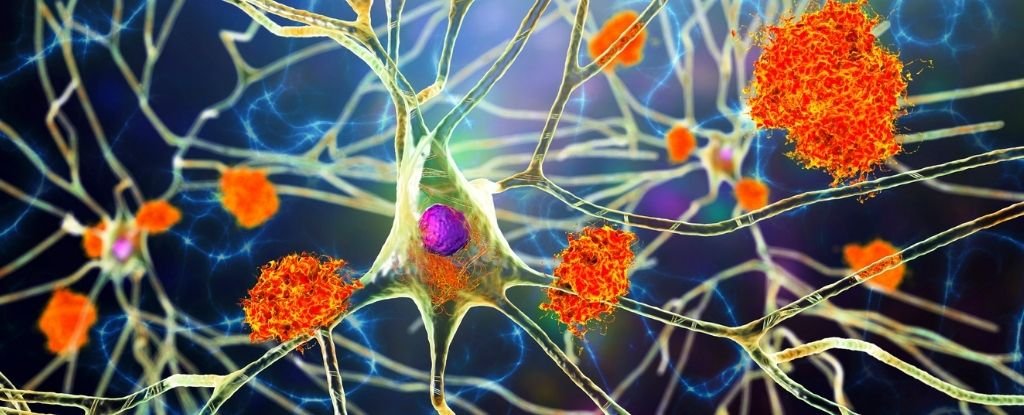
A study of around 500,000 medical records suggested that severe viral infections like encephalitis and pneumonia increase the risk of neurodegenerative diseases like Parkinson’s and Alzheimer’s.
Researchers found 22 connections between viral infections and neurodegenerative conditions in the study of around 450,000 people.
People treated for a type of inflammation of the brain called viral encephalitis were 31 times more likely to develop Alzheimer’s disease. (For every 406 viral encephalitis cases, 24 went on to develop Alzheimer’s disease – around 6 percent.)
Those who were hospitalized with pneumonia after catching the flu seemed to be more susceptible to Alzheimer’s disease, dementia, Parkinson’s disease, and amyotrophic lateral sclerosis (ALS).
Intestinal infections and meningitis (both often caused by a virus), as well as the varicella-zoster virus, which causes shingles, were also implicated in the development of several neurodegenerative diseases.
The impact of viral infections on the brain persisted for up to 15 years in some cases. And there were no instances where exposure to viruses was protective.
Around 80 percent of the viruses implicated in brain diseases were considered ‘neurotrophic’, which means they could cross the blood-brain barrier.
“Strikingly, vaccines are currently available for some of these viruses, including influenza, shingles (varicella-zoster), and pneumonia,” the researchers wrote.
“Although vaccines do not prevent all cases of illness, they are known to dramatically reduce hospitalization rates. This evidence suggests that vaccination may mitigate some risk of developing neurodegenerative disease.”
In 2022, a study of more than 10 million people linked the Epstein-Barr virus with a 32-fold increased risk of multiple sclerosis.
“After reading [this] study, we realized that for years scientists had been searching – one-by-one – for links between an individual neurodegenerative disorder and a specific virus,” said senior author Michael Nalls, a neurogeneticist at the National Institute on Aging in the US.
“That’s when we decided to try a different, more data science-based approach,” he said. “By using medical records, we were able to systematically search for all possible links in one shot.”
First, the researchers analyzed the medical records of around 35,000 Finns with six different types of neurodegenerative diseases and compared this against a group of 310,000 controls who did not have a brain disease.
This analysis yielded 45 links between viral exposure and neurodegenerative diseases, and this was narrowed down to 22 links in a subsequent analysis of 100,000 medical records from the UK Biobank.
While this retrospective observational study cannot demonstrate a causal link, it adds to the pile of research hinting at the role of viruses in Parkinson’s and Alzheimer’s disease.
“Neurodegenerative disorders are a collection of diseases for which there are very few effective treatments and many risk factors,” said co-author Andrew Singleton, a neurogeneticist and Alzheimer’s researcher and the director of the Center for Alzheimer’s and Related Dementias.
“Our results support the idea that viral infections and related inflammation in the nervous system may be common – and possibly avoidable – risk factors for these types of disorders.”