How a sperm and egg fuse together has long been a mystery.
New research by scientists in Austria provides tantalizing clues, showing fertilization works like a lock and key across the animal kingdom, from fish to people.
“We discovered this mechanism that’s really fundamental across all vertebrates as far as we can tell,” said co-author Andrea Pauli at the Research Institute of Molecular Pathology in Vienna.
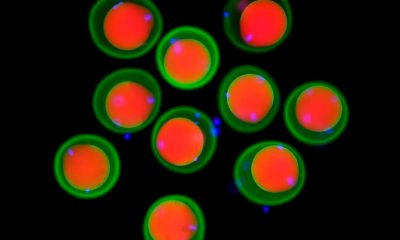
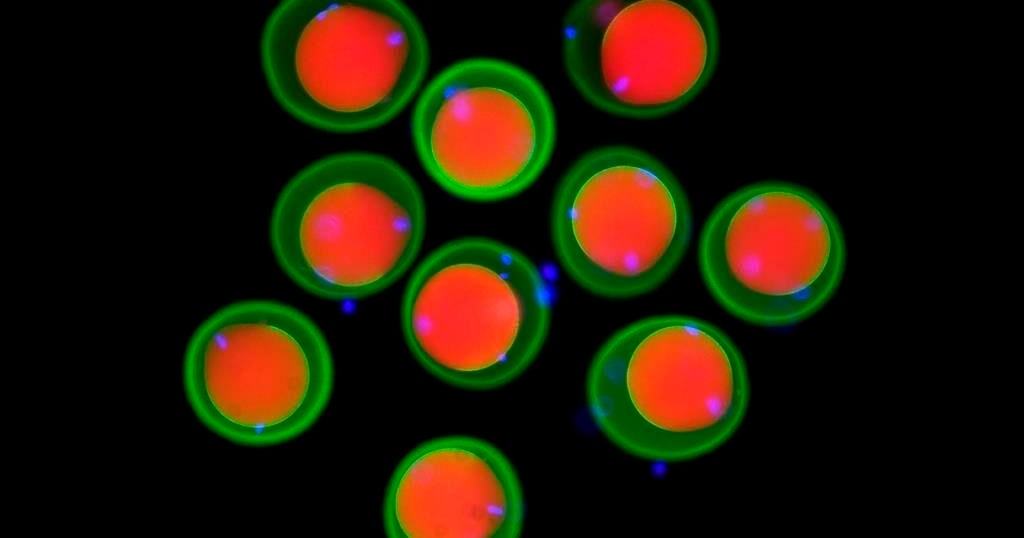
The team found that three proteins on the sperm join to form a sort of key that unlocks the egg, allowing the sperm to attach. Their findings, drawn from studies in zebrafish, mice, and human cells, show how this process has persisted over millions of years of evolution. Results were published Thursday in the journal Cell.
Scientists had previously known about two proteins, one on the surface of the sperm and another on the egg’s membrane. Working with international collaborators, Pauli’s lab used Google DeepMind’s artificial intelligence tool AlphaFold — whose developers were awarded a Nobel Prize earlier this month — to help them identify a new protein that allows the first molecular connection between sperm and egg. They also demonstrated how it functions in living things.
It wasn’t previously known how the proteins “worked together as a team in order to allow sperm and egg to recognize each other,” Pauli said.
Scientists still don’t know how the sperm actually gets inside the egg after it attaches and hope to delve into that next.
Eventually, Pauli said, such work could help other scientists understand infertility better or develop new birth control methods.
The work provides targets for the development of male contraceptives in particular, said David Greenstein, a genetics and cell biology expert at the University of Minnesota who was not involved in the study.
The latest study “also underscores the importance of this year’s Nobel Prize in chemistry,” he said in an email.
___
The Associated Press Health and Science Department receives support from the Howard Hughes Medical Institute’s Science and Educational Media Group. The AP is solely responsible for all content.