Health
Canadian ICUs brace for COVID-19 resurgence on top of the flu – CBC.ca
Intensive care physicians and nurses share their concerns as they brace for an influx of patients that threatens to overwhelm hospitals due to the resurgence of the coronavirus and the flu.
When Canadians successfully flattened epidemic curves during the summer, the goal was to prevent hospitals and intensive care units from facing a crush of too many patients with COVID-19 all at once. Health officials wanted to avoid what happened in hospitals in New York City, where refrigerated trailers were used as temporary morgues.
But the recent surge of new coronavirus cases in all provinces beyond Atlantic Canada has already thwarted surgery plans and led to the cancellation of surgeries such as hip replacements at one hospital in Toronto and postponements in Edmonton.
Dr. Bram Rochwerg, an associate professor at McMaster University and critical care lead at the Juravinski Hospital in Hamilton, anticipates a surge of patients with COVID-19, and he worries they won’t be able to accommodate them all as more surgeries resume.
Unlike in the spring, beds and crucial staffing need to be reserved for medical and surgery patients, too. Traditionally, autumn in hospitals means scrambling for health-care workers such as nurses and respiratory therapists to backfill those sick with the cold and flu or who need to stay home to care for sick children.
“We’re all worried about it,” Rochwerg said. “You see the provincial [COVID-19] numbers creep up day by day. We see that critical care numbers [of ICU patients] creep up.”
The challenge, Rochwerg said, is to find a balance between adding restrictions to protect vulnerable populations such as residents in long-term care homes while preserving crucial aspects of society.
Lessons learned
Rochwerg also pointed to several lessons physicians worldwide have learned to help take better care of patients critically ill with COVID-19 during the resurgence.
“We should treat them like we would any other patient,” he said. “Sometimes, you just need [to insert] a breathing tube.”
When patients are on a ventilator, it takes the skilled hands of four to six hospital staff, including a respiratory therapist who regularly checks the breathing set up and tubing to ensure the airway is protected, as well as nurses to safely turn or “prone” them onto the stomach to improve ventilation.
WATCH | COVID-19 resurgence raises hospital capacity concerns:


There is growing concern that Ontario hospitals and ICUs, especially in Ottawa and Toronto, may not have enough capacity for COVID-19 patients after weeks of rising infections. 1:55
The importance of getting patients up and out of bed, including those on ventilators when possible, as well as excellent nursing care and other day-to-day supportive care can’t be minimized.
“Supportive care is not the sexy part of it, but it’s so crucial,” Rochwerg said.
It gives patients’ bodies time to heal themselves, he said.
Fear of flood of sick patients
Patty Tamlin, registered nurse working in critical care at a hospital in Toronto’s east end, said she’s also concerned about the coming cold-and-flu season.
“One of the biggest concerns is you may be overrun by patients,” Tamlin said.


Her message to Canadians? “Tell everyone to get their flu shot.”
In the spring, the Ontario government created more beds for patients needing long-term ventilated care at a rehabilitation hospital. Even if administrators find more space for more beds, adding temp agency nurses can only go so far, she said.
“It’s going to be a long time,” Tamlin said. “It’s fatiguing … to have this constantly on our head all the time about COVID on top of our regular work.”
Experience, though, has helped ICU staff to prepare for a resurgence of COVID-19 patients.
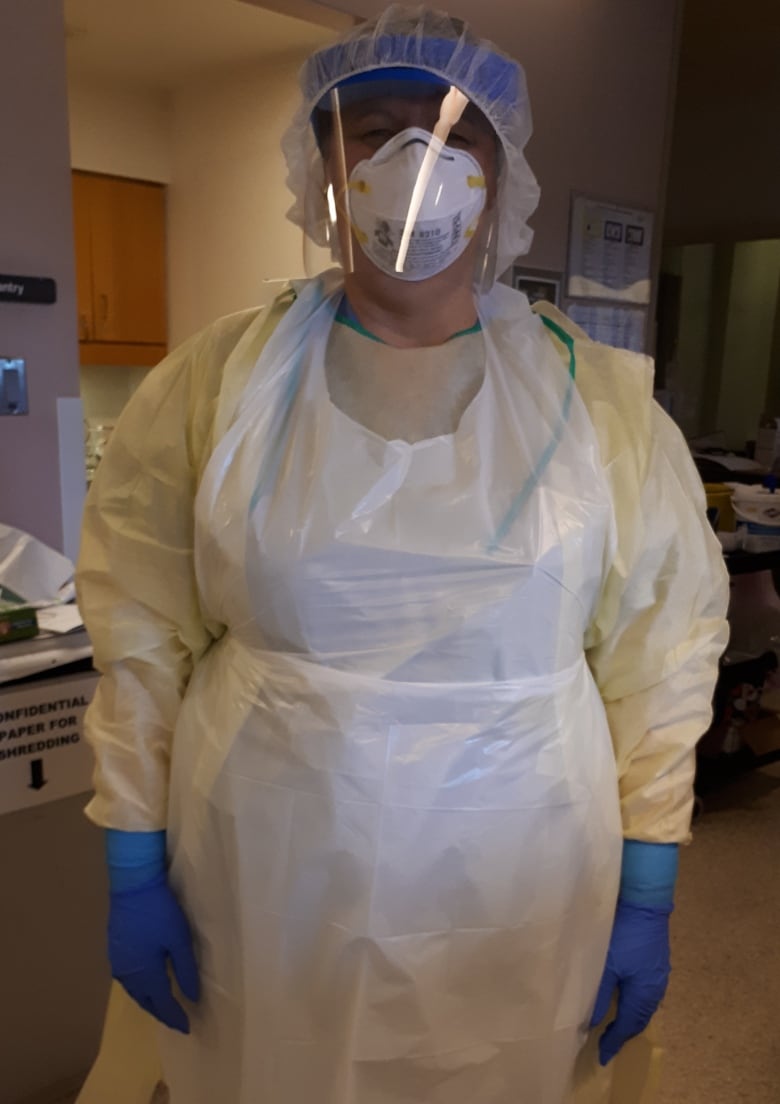
“The more you do something, the more comfortable you are with going in and out of a room,” for example, to perform CPR during a “protected code blue” for cardiac arrest when wearing full personal protective equipment, which can be exhausting. The masks, gowns and gloves need to be donned and removed carefully to avoid health-care workers contaminating themselves.
Dr. Eddy Fan, medical director of the Extracorporeal Life Support (ECLS) program at Toronto’s University Health Network, said the increase in COVID-19 cases so far is “manageable.”
Extracorporeal membrane oxygenation (ECMO) is like an artificial heart and lung machine to support the sickest patients. People with COVID-19 who were intubated at hospitals across Ontario and didn’t improve with conventional therapy were transported to Toronto General for ECMO.
Still, Fan said, “We’re going to need to brace ourselves for another potential flood of very sick patients.”
During the spring, patients were transferred to Toronto General, but family members could not visit. Fan said cutting off patients from their relatives harmed morale not only among loved ones, but it pained people working in the hospital, too.


But influenza season also typically brings patients with lung failure who may need ECMO.
“Their families ask questions like ‘they’re dying of the flu?'” Fan said. “COVID is no different as a viral infection. We see even young patients come with very severe lung failure requiring ECMO.”
During Toronto’s first wave of COVID-19, the team successfully treated a 22-year-old with ECMO.
While respiratory failure from COVID-19 can resemble that of the flu, doctors say the scale is much larger.
Dr. Gregory Haljan, head of Surrey Memorial Hospital’s critical care department in British Columbia, said influenza has vaccines and medical treatments to shorten symptoms and improve death rates. COVID-19 doesn’t, aside from corticosteroids for severe cases.
When Haljan and his co-authors across the Lower Mainland looked at 117 people with COVID-19 who were admitted to ICU between Feb. 20 and April 17, they found the mortality rateranged from one in six to one in 10.
In comparison, the first studies from China and Italy showed mortality rates as high as one in two or one in three.


Safety ‘our primary focus’
Haljan credited having time to prepare, Dr. Bonnie Henry’s “outstanding” leadership as the provincial health officer, the support of British Columbians, hard work and luck.
“We never got overwhelmed,” he said.
To prevent being overwhelmed, Haljan said the hospital and its health region focused on basics, including:
- Engaging patients in the community and long-term care homes through a virtual hospital to keep patients safe at home.
- Improving communication with centralized repositories of information to avoid mixed messages.
- Adapting as the science changes.
“It can be a challenge in that things change very, very slowly because safety is our primary focus,” said Haljan, who works at one of the hospitals caring for among the highest volume of patients in the emergency department, according to the Canadian Institute for Health Information.
“Research is how we keep change safe.”
Haljan said that includes research not only on vaccines and drugs but also measuring patterns and assessing them in areas such as delivering health services.
Health
CFIA continues surveillance for HPAI in cattle, while sticking with original name for disease – RealAgriculture


The Canada Food Inspection Agency will continue to refer to highly pathogenic avian influenza in cattle as HPAI in cattle, and not refer to it as bovine influenza A virus (BIAV), as suggested by the American Association of Bovine Practitioners earlier this month.
Dr. Martin Appelt, senior director for the Canadian Food Inspection Agency, in the interview below, says at this time Canada will stick with “HPAI in cattle” when referencing the disease that’s been confirmed in dairy cattle in multiple states in the U.S.
The CFIA’s naming policy is consistent with the agency’s U.S. counterparts’, as the U.S. Animal and Plant Health Inspection Service has also said it will continue referring to it as HPAI or H5N1.
Appelt explains how the CFIA is learning from the U.S. experience to-date, and how it is working with veterinarians across Canada to stay vigilant for signs of the disease in dairy and beef cattle.
As of April 19, there has not been a confirmed case of HPAI in cattle in Canada. Appelt says it’s too soon to say if an eventual positive case will significantly restrict animal movement, as is the case with positive poultry cases.
This is a major concern for the cattle industry, as beef cattle especially move north and south across the U.S. border by the thousands. Appelt says that CFIA will address an infection in each species differently in conjunction with how the disease is spread and the threat to neighbouring farms or livestock.
Currently, provincial dairy organizations have advised producers to postpone any non-essential tours of dairy barns, as a precaution, in addition to other biosecurity measures to reduce the risk of cattle contracting HPAI.
Subscribe: Apple Podcasts | Spotify | RSS | All Podcasts
jQuery(document).ready(function($) {
$(“#homesub”).validate(
rules:
first_name:
required: true,
minlength: 2
,
last_name:
required: true,
minlength: 2
,
email:
required: true,
email: true,
minlength: 2
,
state:
required: true,
,
role:
required: true,
,
“listid[]”:
required: true,
minlength: 1
,
messages:
first_name: “Your first name is required.”,
last_name: “Your last name is required.”,
email: “Please verify your email is correct.”,
state: “Your state/province is required.”,
role: “Your role is required.”,
“listid[]”: “Select at least one list is required.”
,
submitHandler: function()
$.ajax(
type: “POST”,
url: “https://www.realagriculture.com/wp-admin/admin-ajax.php”,
data:
action: “realag_cc_process_subscribe_onclick”,
form: “homesub”,
data: $(“#homesub”).serialize(),
,
dataType: “html”,
timeout: 30000,
error: function(response)
console.log(response);
,
success: function(response)
$(“#homesub”).html(response);
,
);
);
});
Health
Toronto reports 2 more measles cases. Use our tool to check the spread in Canada – Toronto Star


/* OOVVUU Targeting */
const path = ‘/news/canada’;
const siteName = ‘thestar.com’;
let domain = ‘thestar.com’;
if (siteName === ‘thestar.com’)
domain = ‘thestar.com’;
else if (siteName === ‘niagarafallsreview.ca’)
domain = ‘niagara_falls_review’;
else if (siteName === ‘stcatharinesstandard.ca’)
domain = ‘st_catharines_standard’;
else if (siteName === ‘thepeterboroughexaminer.com’)
domain = ‘the_peterborough_examiner’;
else if (siteName === ‘therecord.com’)
domain = ‘the_record’;
else if (siteName === ‘thespec.com’)
domain = ‘the_spec’;
else if (siteName === ‘wellandtribune.ca’)
domain = ‘welland_tribune’;
else if (siteName === ‘bramptonguardian.com’)
domain = ‘brampton_guardian’;
else if (siteName === ‘caledonenterprise.com’)
domain = ‘caledon_enterprise’;
else if (siteName === ‘cambridgetimes.ca’)
domain = ‘cambridge_times’;
else if (siteName === ‘durhamregion.com’)
domain = ‘durham_region’;
else if (siteName === ‘guelphmercury.com’)
domain = ‘guelph_mercury’;
else if (siteName === ‘insidehalton.com’)
domain = ‘inside_halton’;
else if (siteName === ‘insideottawavalley.com’)
domain = ‘inside_ottawa_valley’;
else if (siteName === ‘mississauga.com’)
domain = ‘mississauga’;
else if (siteName === ‘muskokaregion.com’)
domain = ‘muskoka_region’;
else if (siteName === ‘newhamburgindependent.ca’)
domain = ‘new_hamburg_independent’;
else if (siteName === ‘niagarathisweek.com’)
domain = ‘niagara_this_week’;
else if (siteName === ‘northbaynipissing.com’)
domain = ‘north_bay_nipissing’;
else if (siteName === ‘northumberlandnews.com’)
domain = ‘northumberland_news’;
else if (siteName === ‘orangeville.com’)
domain = ‘orangeville’;
else if (siteName === ‘ourwindsor.ca’)
domain = ‘our_windsor’;
else if (siteName === ‘parrysound.com’)
domain = ‘parrysound’;
else if (siteName === ‘simcoe.com’)
domain = ‘simcoe’;
else if (siteName === ‘theifp.ca’)
domain = ‘the_ifp’;
else if (siteName === ‘waterloochronicle.ca’)
domain = ‘waterloo_chronicle’;
else if (siteName === ‘yorkregion.com’)
domain = ‘york_region’;
let sectionTag = ”;
try
if (domain === ‘thestar.com’ && path.indexOf(‘wires/’) = 0)
sectionTag = ‘/business’;
else if (path.indexOf(‘/autos’) >= 0)
sectionTag = ‘/autos’;
else if (path.indexOf(‘/entertainment’) >= 0)
sectionTag = ‘/entertainment’;
else if (path.indexOf(‘/life’) >= 0)
sectionTag = ‘/life’;
else if (path.indexOf(‘/news’) >= 0)
sectionTag = ‘/news’;
else if (path.indexOf(‘/politics’) >= 0)
sectionTag = ‘/politics’;
else if (path.indexOf(‘/sports’) >= 0)
sectionTag = ‘/sports’;
else if (path.indexOf(‘/opinion’) >= 0)
sectionTag = ‘/opinion’;
} catch (ex)
const descriptionUrl = ‘window.location.href’;
const vid = ‘mediainfo.reference_id’;
const cmsId = ‘2665777’;
let url = `https://pubads.g.doubleclick.net/gampad/ads?iu=/58580620/$domain/video/oovvuu$sectionTag&description_url=$descriptionUrl&vid=$vid&cmsid=$cmsId&tfcd=0&npa=0&sz=640×480&ad_rule=0&gdfp_req=1&output=vast&unviewed_position_start=1&env=vp&impl=s&correlator=`;
url = url.split(‘ ‘).join(”);
window.oovvuuReplacementAdServerURL = url;
Canada has seen a concerning rise in measles cases in the first months of 2024.
By the third week of March, the country had already recorded more than three times the number of cases as all of last year. Canada had just 12 cases of measles in 2023, up from three in 2022.
function buildUserSwitchAccountsForm()
var form = document.getElementById(‘user-local-logout-form-switch-accounts’);
if (form) return;
// build form with javascript since having a form element here breaks the payment modal.
var switchForm = document.createElement(‘form’);
switchForm.setAttribute(‘id’,’user-local-logout-form-switch-accounts’);
switchForm.setAttribute(‘method’,’post’);
switchForm.setAttribute(‘action’,’https://www.thestar.com/tncms/auth/logout/?return=https://www.thestar.com/users/login/?referer_url=https%3A%2F%2Fwww.thestar.com%2Fnews%2Fcanada%2Ftoronto-reports-2-more-measles-cases-use-our-tool-to-check-the-spread-in-canada%2Farticle_20aa7df4-e88f-11ee-8fad-8f8368d7ff53.html’);
switchForm.setAttribute(‘style’,’display:none;’);
var refUrl = document.createElement(‘input’); //input element, text
refUrl.setAttribute(‘type’,’hidden’);
refUrl.setAttribute(‘name’,’referer_url’);
refUrl.setAttribute(‘value’,’https://www.thestar.com/news/canada/toronto-reports-2-more-measles-cases-use-our-tool-to-check-the-spread-in-canada/article_20aa7df4-e88f-11ee-8fad-8f8368d7ff53.html’);
var submit = document.createElement(‘input’);
submit.setAttribute(‘type’,’submit’);
submit.setAttribute(‘name’,’logout’);
submit.setAttribute(‘value’,’Logout’);
switchForm.appendChild(refUrl);
switchForm.appendChild(submit);
document.getElementsByTagName(‘body’)[0].appendChild(switchForm);
function handleUserSwitchAccounts()
window.sessionStorage.removeItem(‘bd-viafoura-oidc’); // clear viafoura JWT token
// logout user before sending them to login page via return url
document.getElementById(‘user-local-logout-form-switch-accounts’).submit();
return false;
buildUserSwitchAccountsForm();
#ont-map-iframepadding:0;width:100%;border:0;overflow:hidden;
#ontario-cases-iframepadding:0;width:100%;border:0;overflow:hidden;
#province-table-iframepadding:0;width:100%;border:0;overflow:hidden;
console.log(‘=====> bRemoveLastParagraph: ‘,0);
Health
Cancer Awareness Month – Métis Nation of Alberta


Cancer Awareness Month
Posted on: Apr 18, 2024
April is Cancer Awareness Month
As we recognize Cancer Awareness Month, we stand together to raise awareness, support those affected, advocate for prevention, early detection, and continued research towards a cure. Cancer is the leading cause of death for Métis women and the second leading cause of death for Métis men. The Otipemisiwak Métis Government of the Métis Nation Within Alberta is working hard to ensure that available supports for Métis Citizens battling cancer are culturally appropriate, comprehensive, and accessible by Métis Albertans at all stages of their cancer journey.
Receiving a cancer diagnosis, whether for yourself or a loved one, can feel overwhelming, leaving you unsure of where to turn for support. In June, our government will be launching the Cancer Supports and Navigation Program which will further support Métis Albertans and their families experiencing cancer by connecting them to OMG-specific cancer resources, external resources, and providing navigation support through the health care system. This program will also include Métis-specific peer support groups for those affected by cancer.
With funding from the Canadian Partnership Against Cancer (CPAC) we have also developed the Métis Cancer Care Course to ensure that Métis Albertans have access to culturally safe and appropriate cancer services. This course is available to cancer care professionals across the country and provides an overview of who Métis people are, our culture, our approaches to health and wellbeing, our experiences with cancer care, and our cancer journey.
Together, we can make a difference in the fight against cancer and ensure equitable access to culturally safe and appropriate care for all Métis Albertans. Please click on the links below to learn more about the supports available for Métis Albertans, including our Compassionate Care: Cancer Transportation program.
I wish you all good health and happiness!
Bobbi Paul-Alook
Secretary of Health & Seniors
-
Media5 hours ago
DJT Stock Rises. Trump Media CEO Alleges Potential Market Manipulation. – Barron's
-
Business24 hours ago
BC short-term rental rules take effect May 1 – CityNews Vancouver
-
Media7 hours ago
Trump Media alerts Nasdaq to potential market manipulation from 'naked' short selling of DJT stock – CNBC
-
Art23 hours ago
Collection of First Nations art stolen from Gordon Head home – Times Colonist
-



 Investment24 hours ago
Investment24 hours agoBenjamin Bergen: Why would anyone invest in Canada now? – National Post
-
Media20 hours ago
DJT Stock Jumps. The Truth Social Owner Is Showing Stockholders How to Block Short Sellers. – Barron's
-
Investment6 hours ago
Private equity gears up for potential National Football League investments – Financial Times
-



 Health20 hours ago
Health20 hours agoType 2 diabetes is not one-size-fits-all: Subtypes affect complications and treatment options – The Conversation




