Health
Engineer Says Where You Sit in a Room Can Influence Your Risk of Catching COVID-19 – ScienceAlert
It doesn’t take long for airborne coronavirus particles to make their way through a room. At first, only people sitting near an infected speaker are at high risk, but as the meeting or class goes on, the tiny aerosols can spread.
That doesn’t mean everyone faces the same level of risk, however.
As an engineer, I have been conducting experiments tracking how aerosols move, including those in the size range that can carry viruses.
What I’ve found is important to understand as more people return to universities, offices and restaurants and more meetings move indoors as temperatures fall. It points to the highest-risk areas in rooms and why proper ventilation is crucial.
As we saw this past few weeks with President Donald Trump and others in Washington, the coronavirus can spread quickly in close quarters if precautions aren’t taken.
University campuses have also been struggling with COVID-19. Cases among 18- to 22-year-olds more than doubled in the Midwest and Northeast after schools reopened in August.
As the case numbers rise, the risk to anyone who spends time in those rooms rises as well.
An experiment shows who’s at greatest risk
Most current models describing the role of ventilation on the fate of airborne microbes in a room assume the air is well mixed, with the particle concentration uniform throughout.
In a poorly ventilated room or small space, that is likely true. In those scenarios, the entire room is a high-risk region.
However, in larger spaces, such as classrooms, good ventilation reduces risk, but likely not uniformly. My research shows that how high the level of risk gets depends a lot on ventilation.
To understand how the coronavirus can spread, we injected aerosol particles similar in size to those from humans into a room and then monitored them with sensors.
We used a 30-foot by 26-foot university classroom designed to accommodate 30 students that had a ventilation system that met the recommended standards.
When we released particles at the front of the classroom, they reached all the way to the back of the room within 10 to 15 minutes.
However, because of active ventilation in the room, the concentrations at the back, about 20 feet (6.1 metres) from the source, were about one-tenth of the concentrations close to the source.
That suggests that with appropriate ventilation, the highest risk for getting COVID-19 could be limited to a small number of people near the infected speaker.
As the time spent indoors with an infected speaker increases, however, risk extends to the entire room, even if ventilation is good.
[embedded content]
CDC finally acknowledges the aerosol risk
In the past, the transmission of respiratory diseases has focused on the role of larger particles that are generated when we sneeze and cough.
These droplets fall quickly to the ground, and social distancing and mask wearing can largely prevent infection from them.
The bigger concern now is the role of tiny particles known as aerosols that are generated when we talk, sing or even just breathe. These particles, often smaller than 5 micrometers, can escape from cloth face masks and linger in air for up to about 12 hours.
The Centers for Disease Control and Prevention finally acknowledged that risk on October 5 after Trump was hospitalized and several other people in or close to the administration tested positive for COVID-19.
While these smaller particles, on average, carry less virus than larger particles that people emit when they cough or sneeze, the high infectivity of SARS-CoV-2 combined with the high viral load before symptoms appear makes these particles important for airborne disease transmission.
How much ventilation is enough?
To minimize COVID-19 transmission indoors, the CDC’s top recommendation is to eliminate the source of infection. Remote learning has effectively done this on many campuses. For face-to-face teaching, engineering measures such as ventilation, partition shields and filtration units can directly remove particles from the air.
Of all the engineering controls, ventilation is probably the most effective tool to minimize infection spread.
Understanding how ventilation lowers your risks of getting COVID-19 starts with air exchange rates. An air exchange of one per hour means that the air supplied to the room over one hour equals the volume of air in the room.
Air exchange rate ranges from less than one for homes to around 15-25 for hospital operating rooms.
For classrooms, the current regulations of primary air flow correspond to an air exchange of about six per hour. That means that every 10 minutes, the amount of air brought into the room equals that of the volume of the room.
How high the concentration gets depends in part on the number of people in the room, how much they emit and the air exchange rate.
With social distancing reducing classroom populations by half and everyone wearing masks, the air in many indoor spaces is actually cleaner now than it was before the pandemic.
Parts of the room to avoid
It’s important to remember that not all parts of a room are at equal risk.
The corners of the room will likely have a lower air exchange – so particles can linger there longer.
Being close to an air exit vent could mean that airborne particles from the rest of the room could wash over you.
A study of ventilation airflow in a restaurant in China traced its role in several COVID-19 illnesses among the patrons there.
About 95 percent of particles in the room will be removed by a properly functioning ventilation system in 30 minutes, but an infected person in the room means those particles are also continuously emitted.
The pace of particle removal can be accelerated by increasing the air exchange rate or adding other engineering controls such as filtration units. Opening windows will also often increase the effective air exchange rate.
As schools, restaurants, malls and other communal spaces start accommodating more people indoors, understanding the risks and following the CDC’s recommendations can help minimize infection spread.
This story has been updated with the CDC’s newly released guidance on aerosols.
Suresh Dhaniyala, Bayard D. Clarkson Distinguished Professor of Mechanical and Aeronautical Engineering, Clarkson University.
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Health
Quebec successfully pushes back against rise in measles cases – CBC.ca
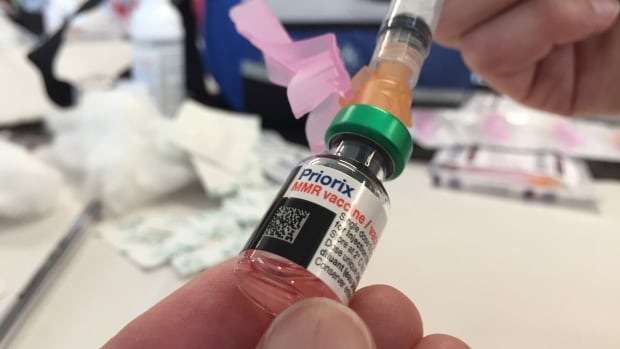
Quebec appears to be winning its battle against the rising tide of measles after 45 cases were confirmed province-wide this year.
“We’ve had no locally transmitted measles cases since March 25, so that’s good news,” said Dr. Paul Le Guerrier, responsible for immunization for Montreal Public Health.
There are 17 patients with measles in Quebec currently, and the most recent case is somebody who was infected while abroad, he said.
But it was no small task to get to this point.
Le Guerrier said once local transmission was detected, news was spread fast among health centres to ensure proper protocols were followed — such as not letting potentially infected people sit in waiting rooms for hours on end.
Then about 90 staffers were put to work, tracking down those who were in contact with positive cases and are not properly vaccinated. They were given post-exposure prophylaxis, which prevents disease, said Le Guerrier.
From there, a vaccination campaign was launched, especially in daycares, schools and neighbourhoods with low inoculation rates. There was an effort to convince parents to get their children vaccinated.
Vaccination in schools boosted
Some schools, mostly in Montreal, had vaccination rates as low as 30 or 40 per cent.
“Vaccination was well accepted and parents responded well,” said Le Guerrier. “Some schools went from very low to as high as 85 to 90 per cent vaccination coverage.”
But it’s not only children who aren’t properly vaccinated. Le Guerrier said people need two doses after age one to be fully inoculated, and he encouraged people to check their status.
There are all kinds of reasons why people aren’t vaccinated, but it’s only about five per cent who are against immunization, he said. So far, some 10,000 people have been vaccinated against measles province-wide during this campaign, Le Guerrier said.
The next step is to continue pushing for further vaccination, but he said, small outbreaks are likely in the future as measles is spreading abroad and travellers are likely to bring it back with them.
Need to improve vaccination rate, expert says
Dr. Donald Vinh, an infectious diseases specialist from the McGill University Health Centre, said it’s not time to rest on our laurels, but this is a good indication that public health is able to take action quickly and that people are willing to listen to health recommendations.
“We are not seeing new cases or at least the new cases are not exceeding the number of cases that we can handle,” said Vinh.
“So these are all reassuring signs, but I don’t think it’s a sign that we need to become complacent.”
Vinh said there are also signs that the public is lagging in vaccine coverage and it’s important to respond to this with improved education and access. Otherwise, microbes capitalize on our weaknesses, he said.
Getting vaccination coverage up to an adequate level is necessary, Vinh said, or more small outbreaks like this will continue to happen.
“And it’s very possible that we may not be able to get one under control if we don’t react quickly enough,” he said.
Health
Pregnant women in the Black Country urged to get whooping cough vaccine – BBC.com


Pregnant women urged to get whooping cough vaccine
Pregnant women in the Black Country are being urged to get vaccinated against whooping cough after a rise in cases.
The bacterial infection of the lungs spreads very easily and can cause serious problems, especially in babies and young children.
The Black Country Integrated Care Board (ICB) is advising pregnant women between 16 and 32 weeks to contact their GP to get the vaccine so their baby has protection from birth.
The UK Health Security Agency warned earlier this year of a steady decline in uptake of the vaccine in pregnant women and children.
Symptoms of the infection, also known as “100-day cough”, are similar to a cold, with a runny nose and sore throat.
Sally Roberts, chief nursing officer for the ICB, which covers Wolverhampton, Dudley, Walsall and Sandwell, said anyone could catch it, but it was more serious for young children and babies.
“Getting vaccinated while you’re pregnant is highly effective in protecting your baby from developing whooping cough in the first few weeks of their life – ideally from 16 weeks up to 32 weeks of pregnancy,” she said.
“If for any reason you miss having the vaccine, you can still have it up until you go into labour.”
Follow BBC West Midlands on Facebook, X and Instagram. Send your story ideas to: newsonline.westmidlands@bbc.co.uk
Health
Measles cases stabilize in Montreal – CityNews Montreal
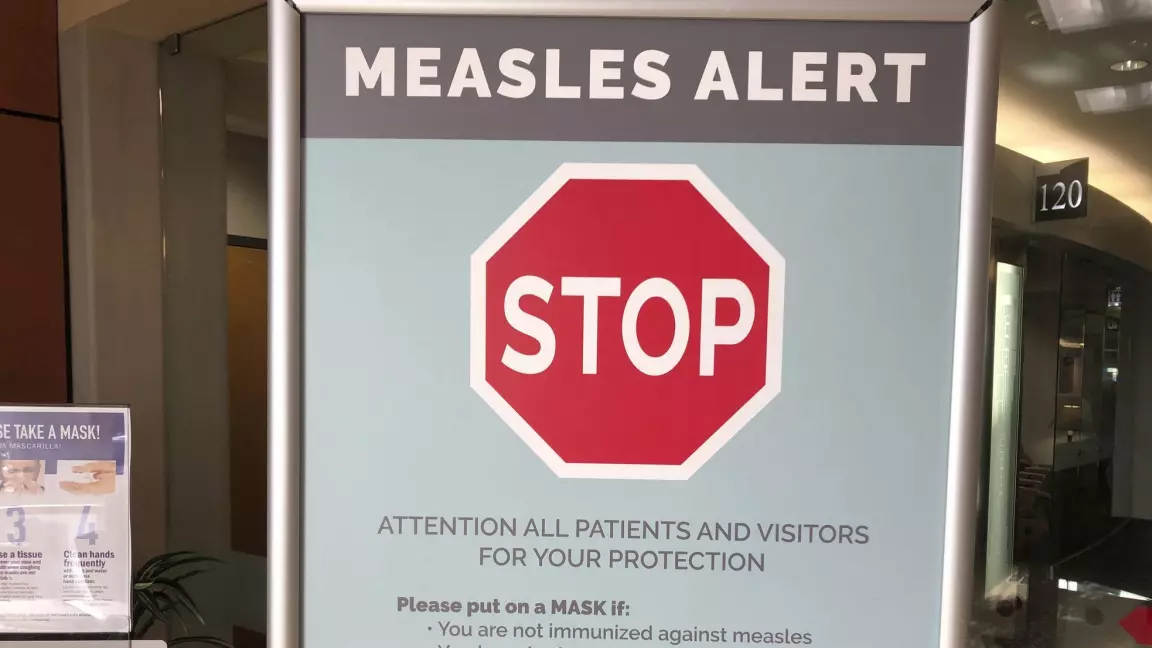
The number of measles cases has stabilized, according to the Montreal Public Health.
Since March 25, there have been no contaminations reported within the community.
“Our teams have identified all contact cases of measles,” said media relations advisor Geneviève Paradis. “It’s a laborious task: each measles case produces hundreds of contacts.”
All community transmission cases since February 2024 have been caused by returning travelers who were either unvaccinated or partially vaccinated.
Currently, there are 18 measles cases in Montreal – with 46 total in Quebec. This according to the April 18 figures from the provincial government.
“With the summer vacations approaching, if you’re travelling, it is essential to check if you are protected against measles,” explained Paradis.
According to Montreal Public Health, a person needs to have received two doses after the age of 12 months to be immunized against the virus.
They’ve launched a vaccination campaign throughout the region, and currently, 11,341 people have been vaccinated against measles in Montreal between March 19 and April 15.
Vaccination is also being provided in schools and at local service points.
“The vaccination operation is under the responsibility of the five CIUSSS of the territory,” concluded Paradis.
-



 Science7 hours ago
Science7 hours agoJeremy Hansen – The Canadian Encyclopedia
-



 Investment7 hours ago
Investment7 hours agoUK Mulls New Curbs on Outbound Investment Over Security Risks – BNN Bloomberg
-



 Health20 hours ago
Health20 hours agoSupervised consumption sites urgently needed, says study – Sudbury.com
-



 Tech6 hours ago
Tech6 hours agoSave $700 Off This 4K Projector at Amazon While You Still Can – CNET
-



 Sports5 hours ago
Sports5 hours agoAuston Matthews denied 70th goal as depleted Leafs lose last regular-season game – Toronto Sun
-
News20 hours ago
Canada's 2024 budget announces 'halal mortgages'. Here's what to know – National Post
-



 Tech5 hours ago
Tech5 hours ago'Kingdom Come: Deliverance II' Revealed In Epic New Trailer And It Looks Incredible – Forbes
-



 Science20 hours ago
Science20 hours agoGiant, 82-foot lizard fish discovered on UK beach could be largest marine reptile ever found – Livescience.com





