Article content
As avian influenza continues to affect local wild bird populations, a Napanee wildlife centre has confirmed that the Highly Pathogenic Avian Influenza (HPAI) variant of avian influenza has been identified in the Kingston region.
Dead bald eagle in Kingston tested positive for the virus

As avian influenza continues to affect local wild bird populations, a Napanee wildlife centre has confirmed that the Highly Pathogenic Avian Influenza (HPAI) variant of avian influenza has been identified in the Kingston region.
Advertisement 2
Article content
According to the Canadian Food Inspection Agency (CFIA), the HPAI virus, also known as H5N1, was first discovered in Canada in 2021 and has since been found in wild birds in every province and territory.
Article content
Leah Birmingham said Sandy Pines Wildlife Centre received confirmation from the Canadian Wildlife Health Cooperative (CWHC) that the highly pathogenic version of the avian influenza virus has not only been discovered in dead Canada geese from Kingston, but also other scavenger species as well.
“They’ve now found it in a raven, a crow and (a bald) eagle,” Birmingham said on Friday. “That makes sense, because all of those birds would potentially feed off of the carcasses of dead Canada geese.”
Last week, Sandy Pines received four crows from Kingston showing neurological symptoms.
Advertisement 3
Article content
“That’s often what you see,” she said. “The water birds typically show a variety of signs of a flu-like disease. But the birds that eat them seem to have more of the neurological signs, like seizures, and less of the upper respiratory ailments.”
In an interview earlier in February, Birmingham told the Whig-Standard that birds showing signs of the virus were being humanely euthanized to limit the risk of spread among the birds who live at or are being rehabilitated at the wildlife centre.
Birmingham said the centre has been sending bird carcasses to the CWHC for viral identification, but lately they’ve been told to stop.
“We’ve already shown positives in the scavenger species essentially,” Birmingham said. “So we know it’s in those bird populations as well.”
Article content
Advertisement 4
Article content
But otherwise, Birmingham said that calls to the wildlife centre about sick birds are on the decline.
“The situation has died down a bit, and it’s just sort of in patches now, not the same intensity,” she said. “That’s a good sign.”
Still, it’s been a record-breaking year in the Kingston region for the virus, Birmingham said.
Kingston, Frontenac and Lennox and Addington Public Health told the Whig-Standard on Friday that as of Feb. 22, 12 birds had tested positive for avian influenza in the region, according to a summary report from the Ontario Ministry of Health.
Of those positive tests, eight of the birds were geese, three were crows and one was an eagle.
It’s not clear how many of those tested positive for the highly pathogenic variant.
Advertisement 5
Article content
The CFIA, which monitors the spread of HPAI with a careful eye to Canada’s poultry industry, keeps a dashboard of active investigations and positive test results from across the country.
Since the end of January, five active outbreaks are under investigation in Ontario, Nova Scotia, Alberta and Quebec.
Max Kaiser, a commercial egg farmer in Greater Napanee, said he treats every wild bird on his property as if it were infected, taking precautions to protect his commercial flocks.
An infection within a commercial poultry flock can take an extreme financial toll on farmers.
“We take every precaution to keep everything out of the barn, whether it’s changing footwear, changing clothes, disinfecting tools, everything we can do to keep our barns clean from whatever’s outside,” he told the Whig-Standard on Friday. “That could be walking through bird droppings in the barnyards, to wild birds perching on the rooftop. It’s concerning at every level.”
Advertisement 6
Article content
While Kaiser isn’t losing sleep over the presence of HPAI in the region, and while biosecurity measures are standard practice at Ontario poultry farms, he is taking extra precautions.
“It’s just diligence. Changing footwear is a simple one, but then when our suppliers, like our feed truck and the delivery vehicles, come and go from the barnyard, they have to disinfect, too, even the tires on the trucks as they come up the laneway,” he said.
Kaiser Lake Farms’ egg operation is located on the shores of Hay Bay, an inlet of Lake Ontario.
“Migratory birds are starting to migrate north again, so we’re ramping up,” Kaiser said. “I’m seeing geese in the fields now that weren’t there a week ago. Now that we’re seeing them, we’re back up to full precautions.”
Advertisement 7
Article content
The Feather Board Command Centre, an organization that provides up-to-date information to Ontario poultry industry members about health risks to commercial bird populations, is recommending heightened biosecurity measures on all of the province’s poultry farms as HPAI moves across the country.
“Currently there are 37 active HPAI cases in Canadian provinces, affecting over 11 million birds,” it said in a news release on Feb. 2. “With the unseasonably warmer weather we have been experiencing, wild birds continue to be on the move and we are seeing increases in wild bird die-offs, increasing the potential risk of disease transmission.”
While HPAI has not been observed to infect humans, some mammals have tested positive for the virus, including raccoons, striped skunks, red foxes, cats and dogs, the CFIA stated on its website.
Advertisement 8
Article content
“While HPAI is primarily a disease of birds, it can also infect mammals, especially those who hunt, scavenge or otherwise consume infected birds,” the agency wrote. “For example, cats that go outdoors may hunt and consume an infected bird, or dogs may scavenge dead birds. In 2023, a dog in Canada was infected with avian influenza after chewing on a wild goose, and died after developing clinical signs.”
KFL&A Public Health recommends on its website that people who discover dead birds on their property wear protective gear while handling bird carcasses, and either bury the bird at a minimum of one metre deep, or double bag and dispose of the carcass in the garbage. Those who discover a dead bird on public property should contact their municipality, the organization said.
Advertisement 9
Article content
Birmingham said people should try, if they can, to bury the carcasses. This prevents the spread of the virus among other animal populations, as well as protect domestic pets that may come in contact with a dead bird.
Still, with its potential threat to both wild birds and commercial operations, Birmingham is urging people not to panic abut the virus.
“I don’t want the public to freak out about all wild birds,” she admitted. “There are all kinds of diseases that wildlife can be the reservoir for and carry. Some of them are manmade because of people bringing animals from one continent to another. And others happen naturally, because of high-density populations of animals … in a way this is nature’s way of sort of taking care of dense populations of animals, right?
“I just don’t want people to be so petrified that their dog or cat is going to get this virus because there were crows in their backyards. It’s not that simple.”
Article content

MILWAUKEE (AP) — Whooping cough is at its highest level in a decade for this time of year, U.S. health officials reported Thursday.
There have been 18,506 cases of whooping cough reported so far, the Centers for Disease Control and Prevention said. That’s the most at this point in the year since 2014, when cases topped 21,800.
The increase is not unexpected — whooping cough peaks every three to five years, health experts said. And the numbers indicate a return to levels before the coronavirus pandemic, when whooping cough and other contagious illnesses plummeted.
Still, the tally has some state health officials concerned, including those in Wisconsin, where there have been about 1,000 cases so far this year, compared to a total of 51 last year.
Nationwide, CDC has reported that kindergarten vaccination rates dipped last year and vaccine exemptions are at an all-time high. Thursday, it released state figures, showing that about 86% of kindergartners in Wisconsin got the whooping cough vaccine, compared to more than 92% nationally.
Whooping cough, also called pertussis, usually starts out like a cold, with a runny nose and other common symptoms, before turning into a prolonged cough. It is treated with antibiotics. Whooping cough used to be very common until a vaccine was introduced in the 1950s, which is now part of routine childhood vaccinations. It is in a shot along with tetanus and diphtheria vaccines. The combo shot is recommended for adults every 10 years.
“They used to call it the 100-day cough because it literally lasts for 100 days,” said Joyce Knestrick, a family nurse practitioner in Wheeling, West Virginia.
Whooping cough is usually seen mostly in infants and young children, who can develop serious complications. That’s why the vaccine is recommended during pregnancy, to pass along protection to the newborn, and for those who spend a lot of time with infants.
But public health workers say outbreaks this year are hitting older kids and teens. In Pennsylvania, most outbreaks have been in middle school, high school and college settings, an official said. Nearly all the cases in Douglas County, Nebraska, are schoolkids and teens, said Justin Frederick, deputy director of the health department.
That includes his own teenage daughter.
“It’s a horrible disease. She still wakes up — after being treated with her antibiotics — in a panic because she’s coughing so much she can’t breathe,” he said.
It’s important to get tested and treated with antibiotics early, said Dr. Kris Bryant, who specializes in pediatric infectious diseases at Norton Children’s in Louisville, Kentucky. People exposed to the bacteria can also take antibiotics to stop the spread.
“Pertussis is worth preventing,” Bryant said. “The good news is that we have safe and effective vaccines.”
___
AP data journalist Kasturi Pananjady contributed to this report.
___
The Associated Press Health and Science Department receives support from the Robert Wood Johnson Foundation. The AP is solely responsible for all content.
The Canadian Press. All rights reserved.
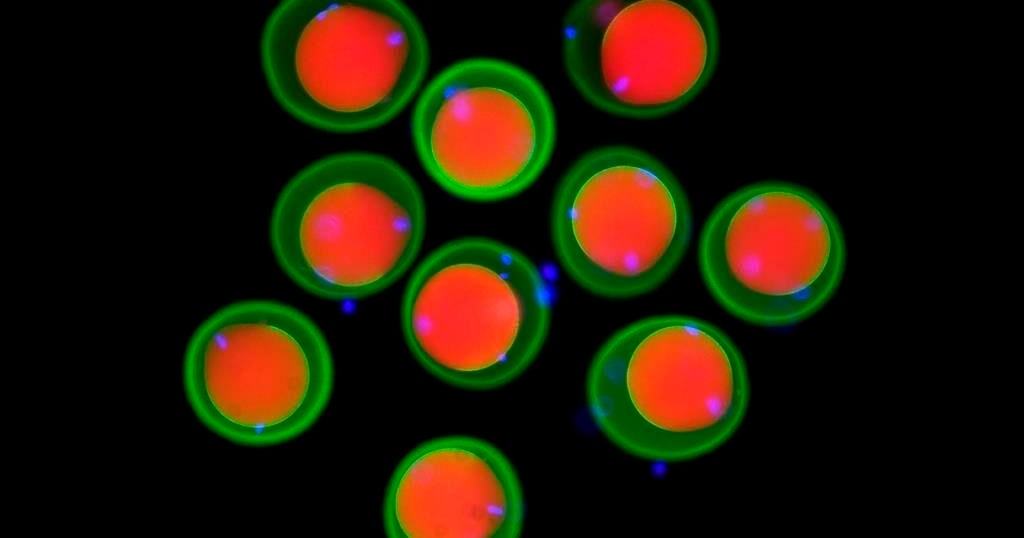
How a sperm and egg fuse together has long been a mystery.
New research by scientists in Austria provides tantalizing clues, showing fertilization works like a lock and key across the animal kingdom, from fish to people.
“We discovered this mechanism that’s really fundamental across all vertebrates as far as we can tell,” said co-author Andrea Pauli at the Research Institute of Molecular Pathology in Vienna.
The team found that three proteins on the sperm join to form a sort of key that unlocks the egg, allowing the sperm to attach. Their findings, drawn from studies in zebrafish, mice, and human cells, show how this process has persisted over millions of years of evolution. Results were published Thursday in the journal Cell.
Scientists had previously known about two proteins, one on the surface of the sperm and another on the egg’s membrane. Working with international collaborators, Pauli’s lab used Google DeepMind’s artificial intelligence tool AlphaFold — whose developers were awarded a Nobel Prize earlier this month — to help them identify a new protein that allows the first molecular connection between sperm and egg. They also demonstrated how it functions in living things.
It wasn’t previously known how the proteins “worked together as a team in order to allow sperm and egg to recognize each other,” Pauli said.
Scientists still don’t know how the sperm actually gets inside the egg after it attaches and hope to delve into that next.
Eventually, Pauli said, such work could help other scientists understand infertility better or develop new birth control methods.
The work provides targets for the development of male contraceptives in particular, said David Greenstein, a genetics and cell biology expert at the University of Minnesota who was not involved in the study.
The latest study “also underscores the importance of this year’s Nobel Prize in chemistry,” he said in an email.
___
The Associated Press Health and Science Department receives support from the Howard Hughes Medical Institute’s Science and Educational Media Group. The AP is solely responsible for all content.
The Canadian Press. All rights reserved.

Patients who are older, don’t speak English, and don’t have a high school education are more likely to experience harm during a hospital stay in Canada, according to new research.
The Canadian Institute for Health Information measured preventableharmful events from 2023 to 2024, such as bed sores and medication errors,experienced by patients who received acute care in hospital.
The research published Thursday shows patients who don’t speak English or French are 30 per cent more likely to experience harm. Patients without a high school education are 20 per cent more likely to endure harm compared to those with higher education levels.
The report also found that patients 85 and older are five times more likely to experience harm during a hospital stay compared to those under 20.
“The goal of this report is to get folks thinking about equity as being a key dimension of the patient safety effort within a hospital,” says Dana Riley, an author of the report and a program lead on CIHI’s population health team.
When a health-care provider and a patient don’t speak the same language, that can result in the administration of a wrong test or procedure, research shows. Similarly, Riley says a lower level of education is associated with a lower level of health literacy, which can result in increased vulnerability to communication errors.
“It’s fairly costly to the patient and it’s costly to the system,” says Riley, noting the average hospital stay for a patient who experiences harm is four times more expensive than the cost of a hospital stay without a harmful event – $42,558 compared to $9,072.
“I think there are a variety of different reasons why we might start to think about patient safety, think about equity, as key interconnected dimensions of health-care quality,” says Riley.
The analysis doesn’t include data on racialized patients because Riley says pan-Canadian data was not available for their research. Data from Quebec and some mental health patients was also excluded due to differences in data collection.
Efforts to reduce patient injuries at one Ontario hospital network appears to have resulted in less harm. Patient falls at Mackenzie Health causing injury are down 40 per cent, pressure injuries have decreased 51 per cent, and central line-associated bloodstream infections, such as IV therapy, have been reduced 34 per cent.
The hospital created a “zero harm” plan in 2019 to reduce errors after a hospital survey revealed low safety scores. They integrated principles used in aviation and nuclear industries, which prioritize safety in complex high-risk environments.
“The premise is first driven by a cultural shift where people feel comfortable actually calling out these events,” says Mackenzie Health President and Chief Executive Officer Altaf Stationwala.
They introduced harm reduction training and daily meetings to discuss risks in the hospital. Mackenzie partnered with virtual interpreters that speak 240 languages and understand medical jargon. Geriatric care nurses serve the nearly 70 per cent of patients over the age of 75, and staff are encouraged to communicate as frequently as possible, and in plain language, says Stationwala.
“What we do in health care is we take control away from patients and families, and what we know is we need to empower patients and families and that ultimately results in better health care.”
This report by The Canadian Press was first published Oct. 17, 2024.
Canadian Press health coverage receives support through a partnership with the Canadian Medical Association. CP is solely responsible for this content.
The Canadian Press. All rights reserved.


In The Rings: Curling Canada still looking for Canadian Curling Trials title sponsor


N.B. election debate: Tory leader forced to defend record on gender policy, housing


After hurricane, with no running water, residents organize to meet a basic need


Alberta government shifts continuing care from Health to Seniors Ministry


Buhai, Green and Shin lead in South Korea after 8-under 64s in first round


Manitoba government halts school building plan, says other methods will be found


Maple Leafs winger Bobby McMann finding game after opening-night scratch


‘Significant overreach’: Ontario municipalities slam province over bike lane rules
Comments