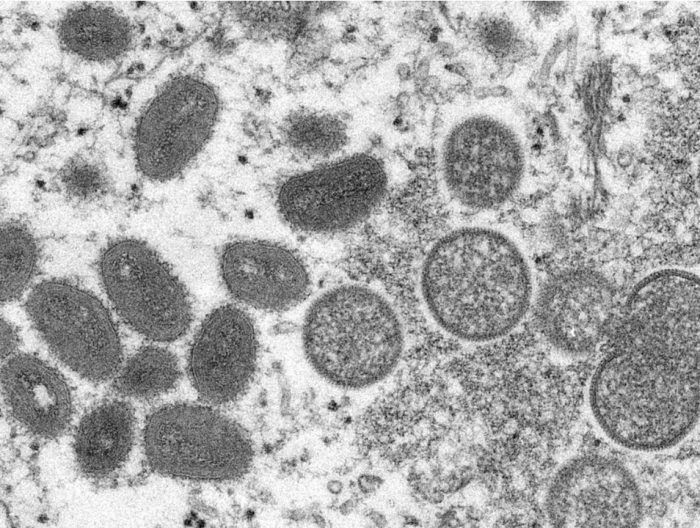
What causes monkeypox?
Like COVID-19, monkeypox is caused by a virus, but a different kind: COVID is caused by a coronavirus made of RNA, while monkeypox comes from what’s known as a poxvirus, made of DNA.
After years of COVID-19 headlines, monkeypox is now in the news.
As of June 3, Canada has confirmed 77 cases of the disease that’s been popping up around the world, with one case found in Alberta last week. According to chief medical officer of health Dr. Deena Hinshaw, the person diagnosed with monkeypox had close contact with a known case outside the province.
David Evans, a microbiology and immunology professor at the University of Alberta, and Timothy Caulfield, a professor in the U of A’s Faculty of Law and School of Public Health, spoke to Postmedia about what Albertans need to know now.
Like COVID-19, monkeypox is caused by a virus, but a different kind: COVID is caused by a coronavirus made of RNA, while monkeypox comes from what’s known as a poxvirus, made of DNA.
Monkeypox was first identified in a lab nearly 70 years ago, and unlike the virus that causes COVID, it isn’t new.
It’s endemic in several countries in west and central Africa, and health authorities there have experience tracking and treating it. But as what’s called a neglected tropical disease, monkeypox has gotten little global attention until the recent cases in non-endemic countries in Europe, as well as U.S. and Canada.
Evans, who specifically studies orthopoxviruses, explained that the monkeypox virus is sometimes used as a stand-in for research on smallpox.
“If we want to test a vaccine that we think will work against smallpox, you check whether it’ll protect against monkeypox, for example.”
While there are still questions around the current disease spread, Evans said he sees “nothing unusual” about this strain of the monkeypox virus.
“It’s not mutating into a new, deadlier strain.”
Hinshaw emphasized last week that monkeypox “does not spread easily between people.” Close, direct contact with an infected person who has symptoms is the main way the disease spreads. There’s risk, too, from contact with items that have been contaminated, like a sick person’s bedsheets or the cutlery they used to eat a meal.
There’s also the potential for monkeypox to spread in respiratory droplets during “prolonged” contact between people.
Symptoms can start out flu-like, with a fever, aches and swollen lymph nodes. After a few days, a rash appears that may spread — although in some recent cases, doctors have seen a more subtle rash with just a few sores in one area of the body.
In Alberta, if you think you’ve been in close contact with someone with monkeypox, or are having symptoms of the disease, you should self-isolate and call 811 or tell your doctor. The infection typically resolves after a few weeks, but the rash can be very painful and cause scarring.
While people should get checked if they think they have a reason to worry, the risk in this province is low.
“That’s not to say that, in the aggregate and from the perspective of global health, this isn’t a serious issue and something that deserves intense scrutiny,” Caulfield said.
“But on that individual risk level right now, I don’t think the average Albertan needs to be too concerned.”
Canada’s deputy chief public health officer Howard Njoo has said that the entire Canadian population is likely susceptible to monkeypox because routine vaccination against smallpox stopped in 1972.
But that doesn’t mean we’re in for a new monkeypox pandemic. It’s much less infectious than COVID, especially when compared to the Omicron variant.
According to the Public Health Agency of Canada (PHAC), the country has a small stockpile of three types of smallpox vaccine that can also work against monkeypox, including a newer vaccine that has far fewer side effects than the shots people would have had before routine immunization stopped.
In Quebec, where there are currently more than 70 confirmed cases of monkeypox, the province is giving access to the vaccine to high-risk contacts of a confirmed or probable monkeypox case. PHAC has said they’re watching the situation closely, but a mass vaccination campaign isn’t necessary at the moment.
Evans said past history of monkeypox outbreaks have historically been small and limited, and there’s more work ahead to find out what’s happening this time
“I think that it’s more the epidemiology of how it got into a particular population and then got spread. That is the difference in this particular case.”
— With files from The Canadian Press
masmith@postmedia.com
twitter.com/meksmith

Some Ontario doctors have started offering a free shot that can protect babies from respiratory syncytial virus while Quebec will begin its immunization program next month.
The new shot called Nirsevimab gives babies antibodies that provide passive immunity to RSV, a major cause of serious lower respiratory tract infections for infants and seniors, which can cause bronchiolitis or pneumonia.
Ontario’s ministry of health says the shot is already available at some doctor’s offices in Ontario with the province’s remaining supply set to arrive by the end of the month.
Quebec will begin administering the shots on Nov. 4 to babies born in hospitals and delivery centers.
Parents in Quebec with babies under six months or those who are older but more vulnerable to infection can also book immunization appointments online.
The injection will be available in Nunavut and Yukon this fall and winter, though administration start dates have not yet been announced.
This report by The Canadian Press was first published Oct. 21, 2024.
-With files from Nicole Ireland
Canadian Press health coverage receives support through a partnership with the Canadian Medical Association. CP is solely responsible for this content.
The Canadian Press. All rights reserved.

ISLAMABAD (AP) — Polio cases are rising ahead of a new vaccination campaign in Pakistan, where violence targeting health workers and the police protecting them has hampered years of efforts toward making the country polio-free.
Since January, health officials have confirmed 39 new polio cases in Pakistan, compared to only six last year, said Anwarul Haq of the National Emergency Operation Center for Polio Eradication.
The new nationwide drive starts Oct. 28 with the aim to vaccinate at least 32 million children. “The whole purpose of these campaigns is to achieve the target of making Pakistan a polio-free state,” he said.
Pakistan regularly launches campaigns against polio despite attacks on the workers and police assigned to the inoculation drives. Militants falsely claim the vaccination campaigns are a Western conspiracy to sterilize children.
Most of the new polio cases were reported in the southwestern Balochistan and southern Sindh province, following by Khyber Pakhtunkhwa province and eastern Punjab province.
The locations are worrying authorities since previous cases were from the restive northwest bordering Afghanistan, where the Taliban government in September suddenly stopped a door-to-door vaccination campaign.
Afghanistan and Pakistan are the two countries in which the spread of the potentially fatal, paralyzing disease has never been stopped. Authorities in Pakistan have said that the Taliban’s decision will have major repercussions beyond the Afghan border, as people from both sides frequently travel to each other’s country.
The World Health Organization has confirmed 18 polio cases in Afghanistan this year, all but two in the south of the country. That’s up from six cases in 2023. Afghanistan used a house-to-house vaccination strategy this June for the first time in five years, a tactic that helped to reach the majority of children targeted, according to WHO.
Health officials in Pakistan say they want the both sides to conduct anti-polio drives simultaneously.
The Canadian Press. All rights reserved.
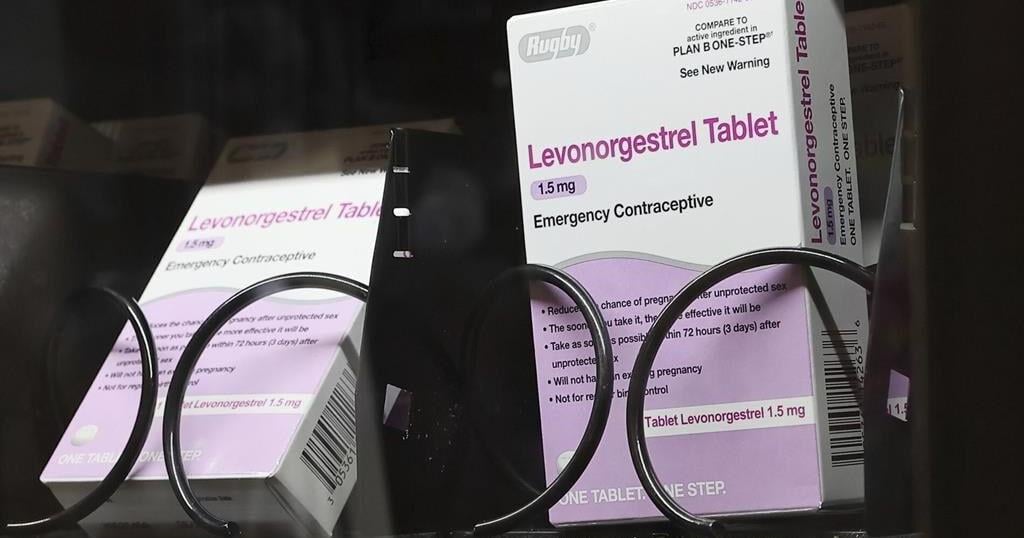
WASHINGTON (AP) — Millions of people with private health insurance would be able to pick up over-the-counter methods like condoms, the “morning after” pill and birth control pills for free under a new rule the White House proposed on Monday.
Right now, health insurers must cover the cost of prescribed contraception, including prescription birth control or even condoms that doctors have issued a prescription for. But the new rule would expand that coverage, allowing millions of people on private health insurance to pick up free condoms, birth control pills, or “morning after” pills from local storefronts without a prescription.
The proposal comes days before Election Day, as Vice President Kamala Harris affixes her presidential campaign to a promise of expanding women’s health care access in the wake of the U.S. Supreme Court’s decision to undo nationwide abortion rights two years ago. Harris has sought to craft a distinct contrast from her Republican challenger, Donald Trump, who appointed some of the judges who issued that ruling.
“The proposed rule we announce today would expand access to birth control at no additional cost for millions of consumers,” Health and Human Services Secretary Xavier Becerra said in a statement. “Bottom line: women should have control over their personal health care decisions. And issuers and providers have an obligation to comply with the law.”
The emergency contraceptives that people on private insurance would be able to access without costs include levonorgestrel, a pill that needs to be taken immediately after sex to prevent pregnancy and is more commonly known by the brand name “Plan B.”
Without a doctor’s prescription, women may pay as much as $50 for a pack of the pills. And women who delay buying the medication in order to get a doctor’s prescription could jeopardize the pill’s effectiveness, since it is most likely to prevent a pregnancy within 72 hours after sex.
If implemented, the new rule would also require insurers to fully bear the cost of the once-a-day Opill, a new over-the-counter birth control pill that the U.S. Food and Drug Administration approved last year. A one-month supply of the pills costs $20.
Federal mandates for private health insurance to cover contraceptive care were first introduced with the Affordable Care Act, which required plans to pick up the cost of FDA-approved birth control that had been prescribed by a doctor as a preventative service.
The proposed rule would not impact those on Medicaid, the insurance program for the poorest Americans. States are largely left to design their own rules around Medicaid coverage for contraception, and few cover over-the-counter methods like Plan B or condoms.
The Canadian Press. All rights reserved.


Forward Jade Kovacevic is the first player signing announced by Northern Super League


What Difference Will You Make to an Employer?


Supply shortage for Ontario home care, palliative patients unacceptable: minister

Harris raises $633 million in the third quarter but spends heavily in final push


Carbon monoxide poisoning suspected in deaths of three found in car in Quebec’s Gaspé


A look at Susan Holt, Liberal premier-designate of New Brunswick


New Brunswick Liberals win majority, Susan Holt first woman to lead province


Jays reliever Green and Canadian slugger O’Neill nominated for comeback player award