Staff looking at resuming more of its normal duties, such as food inspections
Health
Sudbury health unit planning for ‘public health in a COVID-19 world’ – Standard Freeholder

Dr. Penny Sutcliffe
Public Health Sudbury & Districts held its monthly board meeting on Thursday, shortly after announcing two new cases of COVID-19 in the region.
At the meeting, board members looked towards the future as the health unit starts to plan for “public health in a COVID-19 world.”
“Since March of this year, we have had a laser focus on the virus to make sure that we had an effective response to the pandemic,” said Medical Officer of Health, Dr. Penny Sutcliffe.
“We have much of our Board of Health public health programming to our pandemic response, and we have deployed, over that time, at least half of our staff to doing that. Of course, with that, we have not been doing much of our regular programming. There are certainly risks as it relates to the deferral of programs when you think about public health work that hasn’t been occurring.”
Since Sudbury’s first local COVID-19 case was confirmed on March 10, the health unit deferred programs like tobacco cessation and some immunization programs.
“There are also risks that have occurred because of the pandemic response itself. Think, for example, about risk as it relates to mental health and isolation. We’ve heard concerns about domestic violence in homes, and of course, with the reopening, we are now seeing additional risk as it relates to the potential spread of COVID-19.”
The health unit put together a list of priorities based on a number of factors categorized by risk.
Highest on the list is Public Health’s continued emergency preparedness and response plan, the control of infectious diseases, outbreak management, onsite clinic services and immunization programs.
It was also announced that the health unit would resume inspection services to monitor food safety, small drinking water systems and blue-green algae, and continue to implement programs like the needle exchange.
Resources for families, who have been put under considerable stress during the COVID-19 pandemic, will also be a high priority as will mental health and addictions services.
During the meeting, the board also made a decision about transferring funds to the operating budget to help offset the costs related to infrastructure modernization projects.
“The Board of Health was apprised at its Feb. 12 meeting of various assessments conducted to inform the agency’s need for physical and technological infrastructure modernization,” said a memo written by Sutcliffe.
“The modernization is grounded in the need to ensure efficient operations and maintain alignment with evolving legislative requirements and service needs.”
The health unit building at 1300 Paris St, needs renovations, and the cost of the project has been estimated to be $3 millio to $5.5 million. The higher end costs would entail a complete renovation of the HVAC system if it is deemed necessary.
Public Health Sudbury & Districts has submitted a capital funding application for the Dental Clinic and if successful, the agency will use this funding to offset the costs of the physical infrastructure changes to the Rainbow Centre office.
The initial estimate for the Dental Clinic is $1.6 million. The cost for the Health Services and Treatment Clinic component of the Rainbow Centre project is estimated to be $1.4 million (funded through reserves).
The board elected to allow the Medical Officer of Health/CEO to transfer up to $6.5 million from the Facility Equipment and Repairs and Maintenance and Public Health Initiatives reserve funds to the operating budget to offset the cost of these projects.
Looking towards the future, Sutcliffe emphasized the importance of remaining flexible and being able to adapt quickly to changing circumstances.
“There will be really unpredictable expectations placed on us as a public health agency, and not just for a couple of weeks or a couple of months, but for a long period of time,” she said.
“We need to be nimble, meaning that we have to be able to act quickly, and we have to be agile, meaning we have to be able to respond to the situation at hand. We must also be able to do this transparently to be able to plan with clear criteria so we can both scale up and scale down our response depending on what it is we need to do.”
The health unit reminds Sudbury and surrounding districts that while businesses are beginning to reopen, we are not clear of the virus yet.
The risk of infection is still present, and the public is encouraged to follow public health recommendations to control the spread of COVID-19.
The Local Journalism Initiative is made possible through funding from the federal government.
sud.editorial@sunmedia.ca
Twitter: @SudburyStar
Health
Whooping cough is at a decade-high level in US

MILWAUKEE (AP) — Whooping cough is at its highest level in a decade for this time of year, U.S. health officials reported Thursday.
There have been 18,506 cases of whooping cough reported so far, the Centers for Disease Control and Prevention said. That’s the most at this point in the year since 2014, when cases topped 21,800.
The increase is not unexpected — whooping cough peaks every three to five years, health experts said. And the numbers indicate a return to levels before the coronavirus pandemic, when whooping cough and other contagious illnesses plummeted.
Still, the tally has some state health officials concerned, including those in Wisconsin, where there have been about 1,000 cases so far this year, compared to a total of 51 last year.
Nationwide, CDC has reported that kindergarten vaccination rates dipped last year and vaccine exemptions are at an all-time high. Thursday, it released state figures, showing that about 86% of kindergartners in Wisconsin got the whooping cough vaccine, compared to more than 92% nationally.
Whooping cough, also called pertussis, usually starts out like a cold, with a runny nose and other common symptoms, before turning into a prolonged cough. It is treated with antibiotics. Whooping cough used to be very common until a vaccine was introduced in the 1950s, which is now part of routine childhood vaccinations. It is in a shot along with tetanus and diphtheria vaccines. The combo shot is recommended for adults every 10 years.
“They used to call it the 100-day cough because it literally lasts for 100 days,” said Joyce Knestrick, a family nurse practitioner in Wheeling, West Virginia.
Whooping cough is usually seen mostly in infants and young children, who can develop serious complications. That’s why the vaccine is recommended during pregnancy, to pass along protection to the newborn, and for those who spend a lot of time with infants.
But public health workers say outbreaks this year are hitting older kids and teens. In Pennsylvania, most outbreaks have been in middle school, high school and college settings, an official said. Nearly all the cases in Douglas County, Nebraska, are schoolkids and teens, said Justin Frederick, deputy director of the health department.
That includes his own teenage daughter.
“It’s a horrible disease. She still wakes up — after being treated with her antibiotics — in a panic because she’s coughing so much she can’t breathe,” he said.
It’s important to get tested and treated with antibiotics early, said Dr. Kris Bryant, who specializes in pediatric infectious diseases at Norton Children’s in Louisville, Kentucky. People exposed to the bacteria can also take antibiotics to stop the spread.
“Pertussis is worth preventing,” Bryant said. “The good news is that we have safe and effective vaccines.”
___
AP data journalist Kasturi Pananjady contributed to this report.
___
The Associated Press Health and Science Department receives support from the Robert Wood Johnson Foundation. The AP is solely responsible for all content.
The Canadian Press. All rights reserved.
Health
Scientists show how sperm and egg come together like a key in a lock
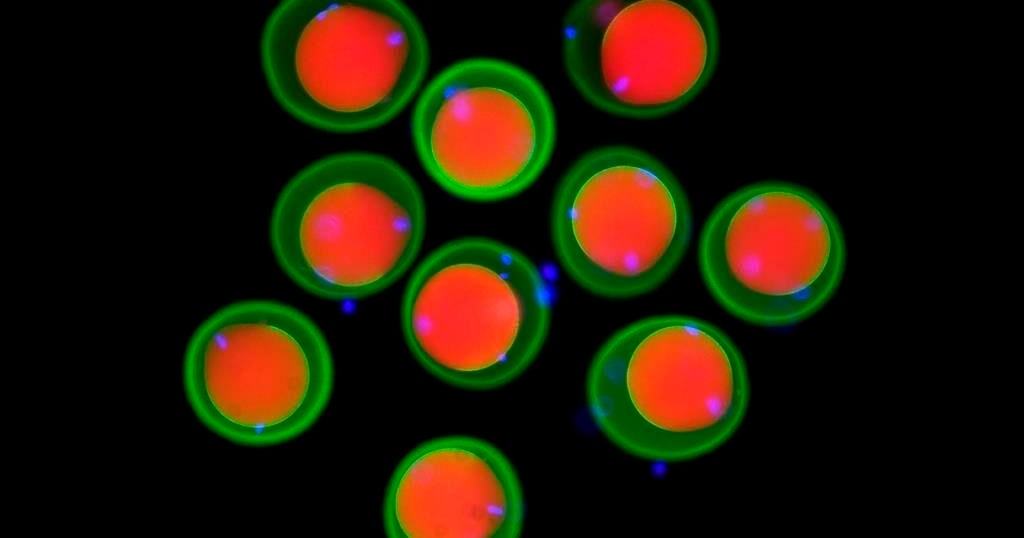
How a sperm and egg fuse together has long been a mystery.
New research by scientists in Austria provides tantalizing clues, showing fertilization works like a lock and key across the animal kingdom, from fish to people.
“We discovered this mechanism that’s really fundamental across all vertebrates as far as we can tell,” said co-author Andrea Pauli at the Research Institute of Molecular Pathology in Vienna.
The team found that three proteins on the sperm join to form a sort of key that unlocks the egg, allowing the sperm to attach. Their findings, drawn from studies in zebrafish, mice, and human cells, show how this process has persisted over millions of years of evolution. Results were published Thursday in the journal Cell.
Scientists had previously known about two proteins, one on the surface of the sperm and another on the egg’s membrane. Working with international collaborators, Pauli’s lab used Google DeepMind’s artificial intelligence tool AlphaFold — whose developers were awarded a Nobel Prize earlier this month — to help them identify a new protein that allows the first molecular connection between sperm and egg. They also demonstrated how it functions in living things.
It wasn’t previously known how the proteins “worked together as a team in order to allow sperm and egg to recognize each other,” Pauli said.
Scientists still don’t know how the sperm actually gets inside the egg after it attaches and hope to delve into that next.
Eventually, Pauli said, such work could help other scientists understand infertility better or develop new birth control methods.
The work provides targets for the development of male contraceptives in particular, said David Greenstein, a genetics and cell biology expert at the University of Minnesota who was not involved in the study.
The latest study “also underscores the importance of this year’s Nobel Prize in chemistry,” he said in an email.
___
The Associated Press Health and Science Department receives support from the Howard Hughes Medical Institute’s Science and Educational Media Group. The AP is solely responsible for all content.
The Canadian Press. All rights reserved.
Health
Older patients, non-English speakers more likely to be harmed in hospital: report

Patients who are older, don’t speak English, and don’t have a high school education are more likely to experience harm during a hospital stay in Canada, according to new research.
The Canadian Institute for Health Information measured preventableharmful events from 2023 to 2024, such as bed sores and medication errors,experienced by patients who received acute care in hospital.
The research published Thursday shows patients who don’t speak English or French are 30 per cent more likely to experience harm. Patients without a high school education are 20 per cent more likely to endure harm compared to those with higher education levels.
The report also found that patients 85 and older are five times more likely to experience harm during a hospital stay compared to those under 20.
“The goal of this report is to get folks thinking about equity as being a key dimension of the patient safety effort within a hospital,” says Dana Riley, an author of the report and a program lead on CIHI’s population health team.
When a health-care provider and a patient don’t speak the same language, that can result in the administration of a wrong test or procedure, research shows. Similarly, Riley says a lower level of education is associated with a lower level of health literacy, which can result in increased vulnerability to communication errors.
“It’s fairly costly to the patient and it’s costly to the system,” says Riley, noting the average hospital stay for a patient who experiences harm is four times more expensive than the cost of a hospital stay without a harmful event – $42,558 compared to $9,072.
“I think there are a variety of different reasons why we might start to think about patient safety, think about equity, as key interconnected dimensions of health-care quality,” says Riley.
The analysis doesn’t include data on racialized patients because Riley says pan-Canadian data was not available for their research. Data from Quebec and some mental health patients was also excluded due to differences in data collection.
Efforts to reduce patient injuries at one Ontario hospital network appears to have resulted in less harm. Patient falls at Mackenzie Health causing injury are down 40 per cent, pressure injuries have decreased 51 per cent, and central line-associated bloodstream infections, such as IV therapy, have been reduced 34 per cent.
The hospital created a “zero harm” plan in 2019 to reduce errors after a hospital survey revealed low safety scores. They integrated principles used in aviation and nuclear industries, which prioritize safety in complex high-risk environments.
“The premise is first driven by a cultural shift where people feel comfortable actually calling out these events,” says Mackenzie Health President and Chief Executive Officer Altaf Stationwala.
They introduced harm reduction training and daily meetings to discuss risks in the hospital. Mackenzie partnered with virtual interpreters that speak 240 languages and understand medical jargon. Geriatric care nurses serve the nearly 70 per cent of patients over the age of 75, and staff are encouraged to communicate as frequently as possible, and in plain language, says Stationwala.
“What we do in health care is we take control away from patients and families, and what we know is we need to empower patients and families and that ultimately results in better health care.”
This report by The Canadian Press was first published Oct. 17, 2024.
Canadian Press health coverage receives support through a partnership with the Canadian Medical Association. CP is solely responsible for this content.
The Canadian Press. All rights reserved.
-

 Sports15 hours ago
Sports15 hours agoIn The Rings: Curling Canada still looking for Canadian Curling Trials title sponsor
-

 Politics15 hours ago
Politics15 hours agoN.B. election debate: Tory leader forced to defend record on gender policy, housing
-

 News14 hours ago
News14 hours agoAfter hurricane, with no running water, residents organize to meet a basic need
-

 News15 hours ago
News15 hours agoAlberta government shifts continuing care from Health to Seniors Ministry
-

 News15 hours ago
News15 hours agoBuhai, Green and Shin lead in South Korea after 8-under 64s in first round
-

 News15 hours ago
News15 hours agoManitoba government halts school building plan, says other methods will be found
-

 Sports15 hours ago
Sports15 hours agoMaple Leafs winger Bobby McMann finding game after opening-night scratch
-

 News15 hours ago
News15 hours ago‘Significant overreach’: Ontario municipalities slam province over bike lane rules






















