News
The latest news on COVID-19 developments in Canada – Richmond News


The latest news on COVID-19 developments in Canada (all times Eastern):
3 p.m.
Saskatchewan is reporting four new deaths and 264 new cases of COVID-19 today.
Two of those who died were people in their 50s in the Far North West region, while the other two were in their 80s — one in the Regina zone and the other in the province’s southeast.
Saskatchewan’s daily COVID-19 update says the province has 2,413 active infections.
It says the seven-day average of new cases in Saskatchewan is 226, or 18.4 new cases per 100,000 people.
—
2:40 p.m.
Manitoba is reporting the deaths of four people with COVID-19, including a man in his 40s and a woman in her 50s.
The province says in its daily COVID-19 update that 82 new cases of the virus have been identified.
The update says there are 259 people in hospital, 101 of whom have active COVID-19 and 158 who are no longer infectious but who still need active care.
It also notes a COVID-19 outbreak has been declared in the dialysis unit at St. Anthony’s General Hospital in The Pas, in northwestern Manitoba.
—
2:20 p.m.
The Alberta government says it will allow limited school and team sports for children and teens to resume on Monday.
The province says in a news release that starting Feb. 8, children and youth will be allowed to take part in “lessons, practices and conditioning activities for indoor and outdoor team-based minor sports and athletics.”
Late last month the province said children’s sport and performance activities could resume Feb. 8 at off-site facilities, but that they had to relate to school activities, such as physical education classes.
At that time, Premier Jason Kenney said that some COVID-19 public health measures were being eased due to lower hospitalization numbers.
Today’s announcement states participants must be 18 years old or younger, excluding coaches or trainers, and notes all games are still prohibited.
There’s also a 10-person maximum, including coaches and trainers, and participants must maintain physical distancing from each other at all times.
—
1:25 p.m.
Health authorities in Newfoundland and Labrador are confirming three new cases of COVID-19 in the province today.
They say two of the infections are linked to travel, including a Quebecer who came to the province for work.
There are 17 active cases but no one in hospital, with 391 people deemed recovered.
Officials are advising against large gatherings ahead of Sunday’s Super Bowl LV, asking people to keep to their close contacts and being mindful of the risks of holding gatherings of a maximum of 20 people, permitted under public health rules.
—
1 p.m.
New Brunswick is reporting two deaths attributed to COVID-19 and 12 new infections in the province.
Health authorities say the deaths are both in the Edmundston area and include a resident in their 80s at the Manoir Belle Vue, a nursing home, and a person in their 60s.
Of the 12 new cases, ten are in the Edmundston area, which remains under lockdown.
Eight people are in hospital, with two in intensive care.
The province has now reported 20 deaths since the beginning of the pandemic and 1,337 confirmed cases with 1,095 recoveries.
—
11:30 a.m.
There are no new cases of COVID-19 in Nova Scotia today, and provincial health officials say the number of active infections in the province has dropped by one to seven.
Premier Stephen McNeil says in a statement he’s proud of Nova Scotians efforts to keep cases low and is telling them to remain vigilant as new measures easing restrictions don’t go into effect until Monday.
Those new measures, in effect until March 7, include an increase in gathering limits to 150 people outdoors and to 50 per cent of an indoor venue’s capacity to a maximum of 100 people.
Retail and fitness businesses will be able to welcome up to 75 per cent of their legal client capacity.
A total of 17,295 doses of COVID-19 vaccines have been administered in Nova Scotia, including 4,681 second doses.
—
11:15 a.m.
Quebec is reporting 1,204 new cases of COVID-19 and 27 further deaths attributed to the novel coronavirus, including nine in the previous 24 hours.
The province’s Health Department is reporting 58 fewer patients in hospital for a total of 982, along with 159 patients requiring intensive care, a drop of nine.
The province administered 4,373 COVID-19 vaccine doses Friday for a total of 253,904.
Quebec has 268,977 confirmed infections and 9,999 deaths since the beginning of the pandemic, with 246,695 people considered recovered.
—
11 a.m.
Ontario is reporting 1,388 new cses of COVID-19 today along with 45 new associated deaths.
Virus-relatd hospitalizations in the province stand at 1,021, with 325 patients in intensive care and 228 on a ventilator.
Ontario Health Minister Christine Elliott says there are 455 new cases in Toronto, 288 in Peel and 131 in York Region.
Those regions are expected to be the last to reopen their economies under a provincial plan that’s set to be announced early next week.
The Canadian Press has learned that Premier Doug Ford is set to reveal details on Monday, but a senior government source says four regions with low case counts may be able to start easing restrictions on businesses as early as Wednesday.
—
This report by The Canadian Press was first published Feb. 6, 2021.
The Canadian Press
News
Federal budget 2024: Billions in new spending, $39.8B deficit – CTV News
In an effort to level the playing field for young people, in the 2024 federal budget, the government is targeting Canada’s highest earners with new taxes in order to help offset billions in new spending to enhance the country’s housing supply and social supports.
Aiming to give Canadian millennials and Generation Z “a fair chance at a middle class life,” Deputy Prime Minister and Finance Minister Chrystia Freeland’s budget outlines how the Liberals plan to allocate $39.2 billion in net-new spending, while upholding the intended fiscal guardrails.
Framed as pursuing tax fairness, one of the main ways the Liberals are planning to bring in new revenue is by “asking” Canada’s very wealthiest to pay more, with Freeland saying it would be irresponsible to pass on more debt to future generations by ignoring the fiscal anchors Freeland tied government to last fall.
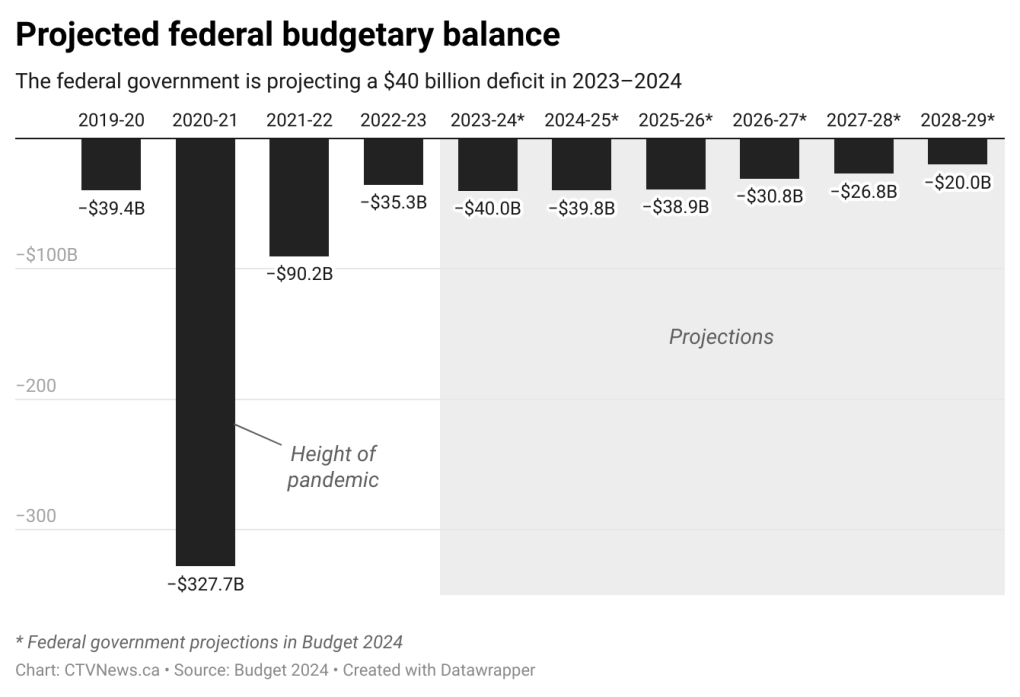
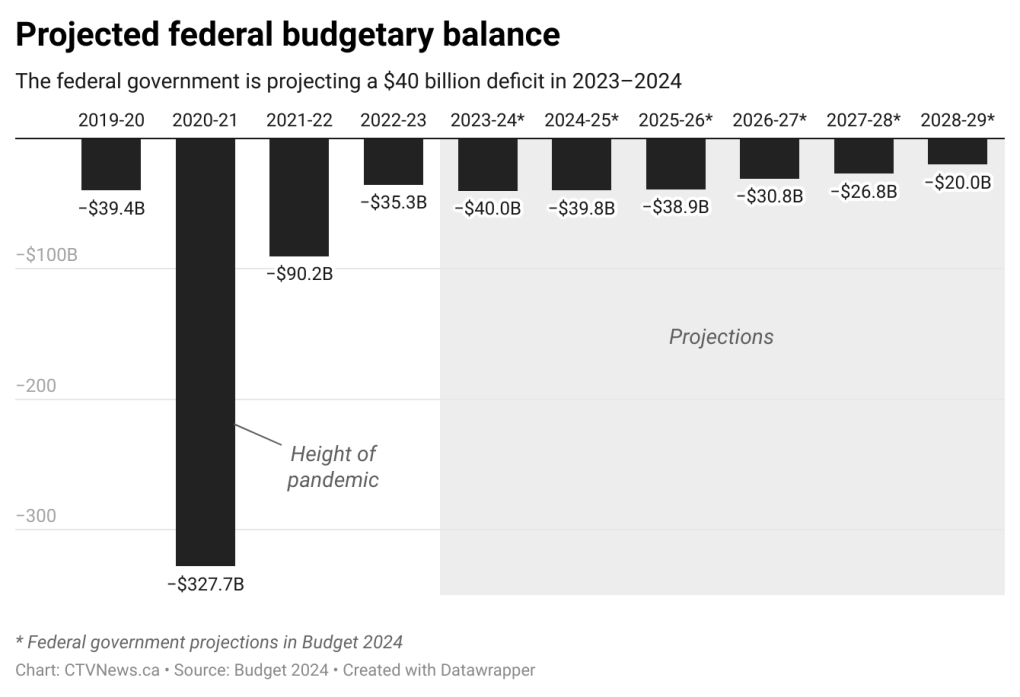
However, with still no projected budget balance and bigger deficits forecasted in every year ahead than was previously projected, the budget — titled “Fairness for Every Generation” — notes that federal public debt charges are on track to balloon to $64.3 billion in 2028-29.
Aside from the weeks long pre-budget blitz of expected new measures, the 2024 budget includes some additional offerings for small businesses and entrepreneurs – including through a new carbon rebate – and finally puts dollar figures on the first phase of national pharmacare, as well as the long-promised disability benefit.
Overall, the 2024 federal budget includes $52.9 billion in new spending plans – some of which is loan-based and reliant on provincial buy-in – as well as an estimated $20 billion in new tax revenue, including tobacco and vaping taxes.
According to the budget, the federal deficit is projected to be $39.8 billion in 2024-25, $38.9 billion in 2025-26, and declining over the three years following, to $20 billion by 2028-29.
Freeland did hit her target of maintaining the 2023-24 federal deficit at $40.1 billion, and will be lowering the debt-to-GDP ratio in the current fiscal year. She’s also standing firm on her plans to “refocus” $15.8 billion over five years and $4.8 billion ongoing in government spending.
“Our renewed focus today is unlocking the door to the middle class for millions of younger Canadians,” Freeland writes in the foreword to the budget, of which all 416 pages were tabled in the House of Commons on Tuesday.
“Because that is what you have earned, and that is what you deserve. And that is what your parents and grandparents want for you, too.”
Speaking with reporters inside the budget lockup, Freeland defended her new revenue plan as helping “make life cost less for millions,” while touting that the Canadian economy is outperforming expectations and on track to continue to improve in the year ahead.


Banking on this “soft landing” and for inflation to decline to close to two per cent by the end of the year, the finance minister said the federal government feels like now is the time to meet the moment with more investments to help spur competition and job growth, while maintaining low deficit- and net debt-to-GDP ratios.
However, some economists warn not enough is being done in this massive financial document, on the productivity side.
Fred O’Riordan, the national leader for tax policy at EY, told CTV News that in his view, it was the “missing element” of the budget. “There are very few measures that are designed to increase capital investment and enhance labour productivity.”
“Today’s budget contains few surprises… and the government’s projections for the deficit are largely in line with previous predictions,” said Canadian Chamber of Commerce CEO Perrin Beatty.
“Instead of using a revenue windfall to reduce the deficit more quickly, the government chose to use it along with changes to the capital gains tax, to fund this new spending. What’s still missing is a clear plan to promote productivity and restore economic growth in Canada.”
On Parliament Hill, Freeland’s fiscal roadmap received mixed reviews, with opposition parties largely decrying the missed opportunities and “box-checking politics” within it.
Wealthiest Canadians to be taxed more
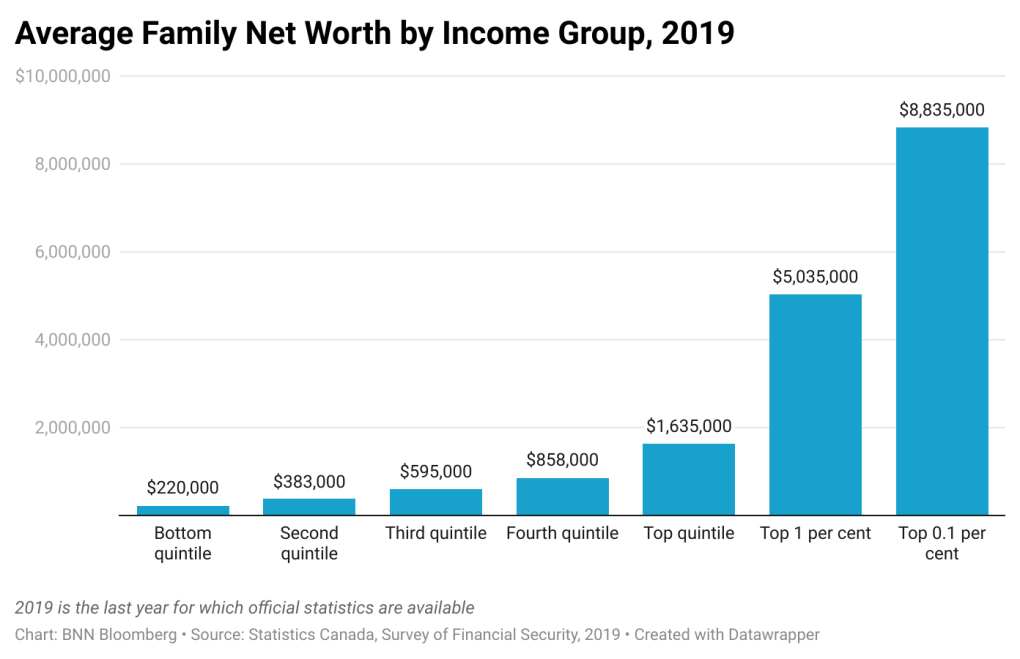
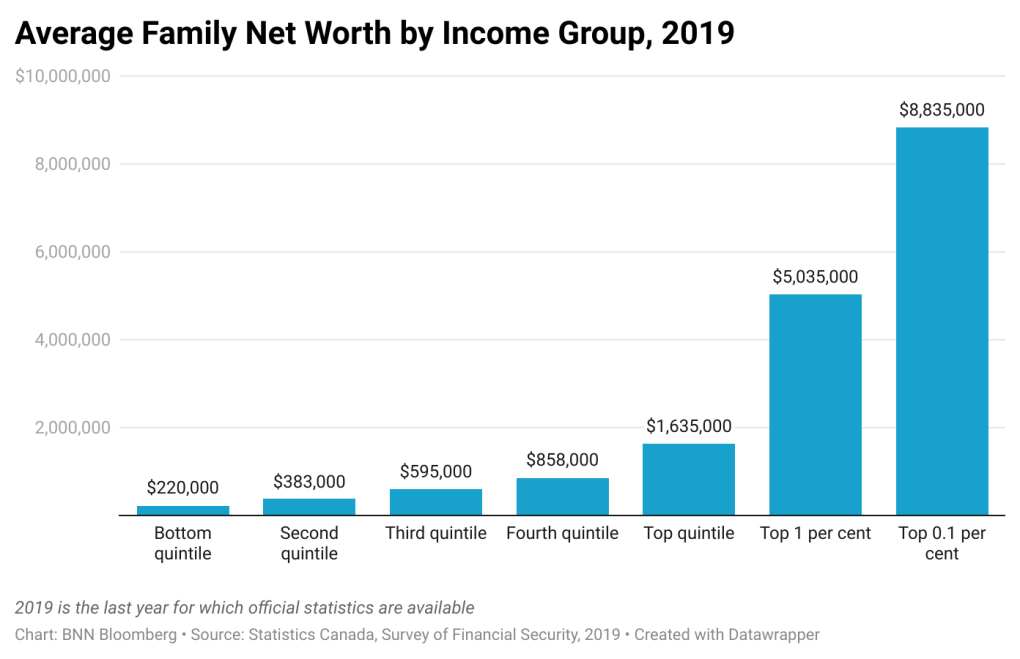
The most significant new component of Tuesday’s budget is a new revenue stream: an increase in taxes on capital gains for Canada’s highest earners, projected to rake in $19.3 billion over the next five years.
While not exactly the wealth tax or excess profit tax some had suspected, Freeland is targeting the wealthiest 0.13 per cent by increasing the capital gains inclusion rate — the portion of capital gains on which tax is paid – for individuals with more than $250,000 in capital gains in a year.
The rate will increase from one-half to two-thirds, and will also apply to all capital gains realized by corporations and trusts. This is expected to impact approximately 12 per cent of Canada’s corporations and Canadians with an average income of $1.42 million.
This tax change will apply to capital gains realized on, or after June 25, 2024.
The Liberals, who vowed to not raise taxes on Canada’s middle class, made a point of noting in the budget that this change will not impact 99.87 per cent of Canadians.
Freeland also said this increase to the capital gains inclusion rate is not expected to hinder Canada’s business competitiveness, as corporations in most other countries pay corporate income tax on 100 per cent of their capital gains.
Heading into budget day, economic experts had cautioned that more direct wealth or excess profit taxes could have run counter to the Liberals’ efforts to boost productivity, and growth, but opting to go this route is largely being characterized as a safer bet.
New details on housing, Gen Z pledges
Taking the premise that the best way to make home prices and rents more affordable is to quickly increase supply, the 2024 budget includes the comprehensive package of housing policy initiatives Prime Minister Justin Trudeau and his cabinet have been teasing out for weeks.
Promising to build 3.9 million homes by 2031, the housing strategy includes a bevy of measures and $8.5 billion in additional spending. Much of this spending is spread out over the years ahead.
Among the biggest ticket housing commitments are a $15-billion top-up to the Apartment Construction Loan Program; $6 billion for a Canada Housing Infrastructure Fund; as well as $1 billion in loans and $470 million in contributions for a new rental protection fund.
The 2024 budget also includes $400 million to top up the Housing Accelerator Fund by $400 million, plus $600 million for a series of new homebuilding innovation efforts aimed at scaling up modular and prefabricated homes.
It remains to be seen what the timeline will be for enacting the promised Canadian Renters’ Bill of Rights, and select other mortgage and rental rule reforms. Though, allowing 30-year mortgage amortizations for first-time homebuyers purchasing new builds, will be available starting Aug. 1, 2024.
Policy-wise, the budget offers more intel about plans to enact a “public lands for homes” strategy. According to the government, this initiative intends to “unlock 250,000 new homes” by converting unused office towers, parking lots, Canada Post and National Defence properties, into residential land.
Specifically, $1.1 billion is being earmarked over 10 years to convert 50 per cent of the federal government’s office space into housing, saving $3.9 billion over that same period of time. It remains to be seen what the pricing strategy will be for this federal effort to sell off, or re-zone, this land.
The first batch of five federal properties being leased to housing providers “immediately” are in Calgary, Edmonton, Ottawa, Toronto, and Montreal, amounting to 800 new homes.
Further, consultations are coming on a potential tax on residentially-zoned vacant land.
“I think what they are doing on land is quite smart. We have more Canada Posts in this country than we have Tim Hortons. So, that’s a lot of re-development opportunities,” said economist Mike Moffatt, who the Liberals have directly consulted in recent months on their housing plans.
While the Liberals are framing this overall major push on housing as helping younger Canadians, there are also a few specifically Generation Z and millennial-targeted measures, including creating more jobs through a $207.6 million Student Work Placement Program boost, and extending increased student grants and interest-free loans.
The federal government will also be updating the formula that is used by the Canada Student Financial Assistance Program to calculate housing costs when determining financial need, to reflect today’s higher housing costs. The budget estimates this will deliver more student aid to 79,000 students a year.
“We may look back on the 2024 budget as a game-changer,” Paul Kershaw, founder of Generation Squeeze told CTV News.
“This budget is saying ‘we have to acknowledge that hard work isn’t paying off for younger Canadians as it did for past generations… The first step in solving a problem, is acknowledging it.”
Next steps on social safety net efforts
There are a series of chapters within the 2024 federal budget focused on various efforts to expand elements that could be considered part of Canada’s social safety net.
Newly unveiled Tuesday, this includes $1.5 billion over five years to launch the new national universal pharmacare plan. The first phase, as pre-announced, will help cover diabetes and contraception medications starting this fiscal year.
“The preliminary coverage of diabetes and birth control drugs in this budget is another example of the Liberal-NDP supply confidence agreement bearing fruit… While this program is still limited in scope, it represents the most tangible steps towards universal pharmacare that we’ve ever seen in this country,” said Canadian Centre for Policy Alternatives senior economist David Macdonald.
And, the Liberals have finally put funding behind their long-promised Canada Disability Benefit: $6.1 billion over six years and $1.4 billion ongoing, seeing the first payments issued in July 2025.
This federal income supplement has been framed as a legacy social policy that will help hundreds of thousands of low-income, working-age people with disabilities, and is meant to supplement existing provincial and territorial benefits. The budget also vows coverage for the cost of medical forms required to apply for this financial assistance.
The budget also includes more than a dozen new initiatives connected to the Liberals’ longstanding commitment to Indigenous reconciliation.
Among them: a promise to spend $927 million over five years on new on-reserve income assistance; $1.8 billion to help Indigenous people exercise their jurisdiction; $5 billion in loan guarantees related to energy projects; and $1.3 million to advance the “Red Dress Alert” (similar to an Amber Alert) initiative.
Further, as pre-announced, the 2024 budget includes $1 billion over five years to fund a new national school food program intended to provide meals to 400,000 more kids.
It also earmarks $500 million for a new youth mental health fund; $1 billion in loans and $60 million in grants to build or renovate child-care centres; and $48 million to extend student loan forgiveness for early childhood educators.
Small business, research supports
Freeland’s plans include new measures meant to provide businesses more certainty when it comes to investing in Canada, including a series of incentives and supports to boost productivity.
As part of a new small business-focused package, the budget earmarks $200 million over two years, starting in 2026-27, to increase access to venture capital for “equity-deserving entrepreneurs,” and those outside of major hubs.
Further, the Liberals are promising a new “Canada Carbon Rebate for Small Businesses” that vows to rapidly return the proceeds from the federal pollution price from 2019-20 to 2023-24 to 600,000 businesses with fewer than 500 employees through a new refundable tax credit, estimated to cost $2.5 billion.
There’s talk of a new Canadian Entrepreneurs’ Incentive to provide a tax break, advancing work on regulatory “sandboxes,” further red tape reduction measures and acting on foreign credential recognition.
Further, $3.5 billion is being promised for strategic research infrastructure, investments in modernized facilities, including $2.4 billion for core research grants and to foster homegrown talent through improved scholarships and fellowships.
As expected, the budget also includes $2.4 billion to build capacity in artificial intelligence, largely for computing capabilities and technical infrastructure.
New spending on safety, defence, online harms
Lastly, the 2024 federal budget includes the pre-promised billions in defence spending over the long-term and volunteer firefighter and search and rescue tax credits.
Beyond this on the safety front, the government notes it plans to move ahead with “additional penalties under the Criminal Code for those who commit an auto-theft related offence,” and is earmarking $30.4 million for the buyback of assault-style firearms.
The budget also includes $273.6 million for Canada’s Action Plan on Combatting Hate, and $16 million to help “create a safer and more welcoming sport environment” for all athletes.
Related to the yet-to-be-passed online harms legislation, the federal government proposes to provide $52 million over five years, starting this year, to Canadian Heritage and the Royal Canadian Mounted Police to fulfill their obligations regarding protecting children, ensuring major online platforms are abiding by the coming new regulations, and to set up the promised Digital Safety Commission.
An additional $7.5 million will be going to the Public Health Agency of Canada to support the Kids Help Phone over the next three years, while Public Safety Canada is getting $2.5 million to support the Canadian Centre for Child Protection.
Political reaction to Freeland’s plans
Rising to respond to the budget in the House of Commons, Conservative Leader Pierre Poilievre echoed the demand he made in the morning, before having seen the document, for Trudeau to “please stop” his spending plans until a Conservative government can take over.
“Everything on which the prime minister spends gets worse and more costly. He has spent, and Canadians are broke,” Poilievre said. “This is not a government that gives people everything they want. It’s a government that takes everything they have.”


In an exchange during Tuesday’s post-budget debate, Freeland attempted to pin Poilievre down on whether he would show his “true colours” and come out and say that while framing himself as “being on the side of working people,” he opposes making those at the very top pay more.
It is expected that the Liberals’ effort to wedge the Conservatives on this point will continue in the days of priority debate ahead.
In an interview on CTV News Channel’s Power Play, NDP Leader Jagmeet Singh – as has become an annual tradition since the two-party confidence pact went into effect – wouldn’t say whether he will support this budget.
Singh said while there are a number of elements in the budget that his party fought for, he’s “got some concerns” that he wants addressed before the New Democrats can commit to supporting the spending plan.
“What about the fact that they have not addressed the gap in infrastructure and housing spending for Indigenous communities? Or the fact that people waited for a year and a half for the disability benefit, and it’s only $200, at a time when the cost of living is so high? What’s the plan to increase that? So I want to hear (a) response to those concerns,” Singh said.
The Bloc Quebecois, meanwhile, wrote in a press release that “the budget only serves Justin Trudeau” and the prime minister’s electoral goals.
Bloc Leader Yves-François Blanchet added in the release that the budget does not meet his party’s expectations when it comes to support for seniors or asylum seekers, and that it steps on Quebec’s provincial jurisdiction when it comes to issues like housing.
Green Party co-leader Elizabeth May called the budget “a prime example of box-checking politics, showcasing a series of half-measures that do not respond to the scale of the challenges Canadians are facing.”
“This budget looked like our dream budget, with so many mentions of our key demands on climate, housing and inequality, until we delved into the details,” May said in a statement. “This budget was an opportunity to start a systemic shift to rise to the challenges currently facing the country. The Liberals failed that test.”
News
'Terrific news': Chief economist reacts to latest inflation data – BNN Bloomberg


After Statistics Canada’s latest consumer price index revealed a 2.9 per cent increase in the annual inflation rate in March, largely boosted by higher prices for gasoline, one chief economist says the path towards a June interest rate cut seems clear.
Excluding gasoline prices, Statistics Canada reported that the overall annual inflation rate for March was 2.8 per cent, a drop from 2.9 per cent in February.
“It’s terrific news, really,” said Pedro Antunes, chief economist of the Conference Board of Canada, during an interview with BNN Bloomberg on Tuesday.
“I think this is going to be another sign and insurance that the (Bank of Canada) is going to start to take that burden off of households by lowering interest rates come June,” he said, adding that the central bank has been “very careful around its messaging.”
“Perhaps some mistakes were made during the pandemic about where interest rates are going to go, and I think they’ve been very careful now in the downswing of things,” Antunes said.
Despite anticipating a decline in rates this summer, Antunes also cautioned that the speed of the decline will be “slow.”
“Let’s not forget on the way down I think interest rate declines are going to be way slower and certainly take more time than when they came up,” he said.
Antunes also mentioned that the U.S. is in a more precarious position when it comes to the prospect of rate cuts.
“In the U.S., they’re not having as much certainty around rates coming down,” he said. “This is why that differential on interest rates is causing the dollar to come down a little bit. But it’s also important to note that if U.S. rates stay high, that is going to have an impact on market rates even here in Canada as well.”
To watch Antunes’ full interview with BNN Bloomberg, click the video above.
News
Richard Chevolleau Short Film “Marvelous Marvin” Set to go to Camera
|
|
|
|
|
|
|
|
|
-



 Sports6 hours ago
Sports6 hours agoTeam Canada’s Olympics looks designed by Lululemon
-
Real eState14 hours ago
Search platform ranks Moncton real estate high | CTV News – CTV News Atlantic
-
Tech13 hours ago
Motorola's Edge 50 Phone Line Has Moto AI, 125-Watt Charging – CNET
-



 Investment22 hours ago
Investment22 hours agoSo You Own Algonquin Stock: Is It Still a Good Investment? – The Motley Fool Canada
-



 Science17 hours ago
Science17 hours agoSpace exploration: A luxury or a necessity? – Phys.org
-
News24 hours ago
Federal budget will include tax hike for wealthy Canadians, sources say – CBC.ca
-



 Investment20 hours ago
Investment20 hours agoGoldman Sachs Backs AI in Hospitals With $47.5 Million Kontakt.io Investment – BNN Bloomberg
-



 Politics17 hours ago
Politics17 hours agoLiz Truss backs Donald Trump to win US presidential election – BBC.com







