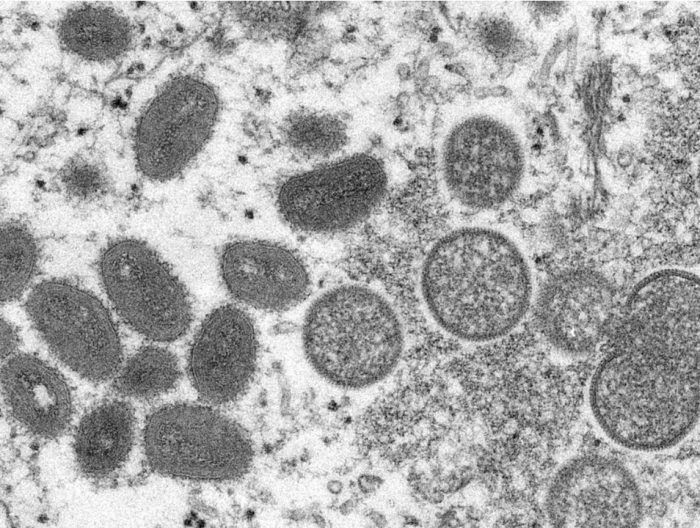
What causes monkeypox?
Like COVID-19, monkeypox is caused by a virus, but a different kind: COVID is caused by a coronavirus made of RNA, while monkeypox comes from what’s known as a poxvirus, made of DNA.
After years of COVID-19 headlines, monkeypox is now in the news.
As of June 3, Canada has confirmed 77 cases of the disease that’s been popping up around the world, with one case found in Alberta last week. According to chief medical officer of health Dr. Deena Hinshaw, the person diagnosed with monkeypox had close contact with a known case outside the province.
David Evans, a microbiology and immunology professor at the University of Alberta, and Timothy Caulfield, a professor in the U of A’s Faculty of Law and School of Public Health, spoke to Postmedia about what Albertans need to know now.
Like COVID-19, monkeypox is caused by a virus, but a different kind: COVID is caused by a coronavirus made of RNA, while monkeypox comes from what’s known as a poxvirus, made of DNA.
Monkeypox was first identified in a lab nearly 70 years ago, and unlike the virus that causes COVID, it isn’t new.
It’s endemic in several countries in west and central Africa, and health authorities there have experience tracking and treating it. But as what’s called a neglected tropical disease, monkeypox has gotten little global attention until the recent cases in non-endemic countries in Europe, as well as U.S. and Canada.
Evans, who specifically studies orthopoxviruses, explained that the monkeypox virus is sometimes used as a stand-in for research on smallpox.
“If we want to test a vaccine that we think will work against smallpox, you check whether it’ll protect against monkeypox, for example.”
While there are still questions around the current disease spread, Evans said he sees “nothing unusual” about this strain of the monkeypox virus.
“It’s not mutating into a new, deadlier strain.”
Hinshaw emphasized last week that monkeypox “does not spread easily between people.” Close, direct contact with an infected person who has symptoms is the main way the disease spreads. There’s risk, too, from contact with items that have been contaminated, like a sick person’s bedsheets or the cutlery they used to eat a meal.
There’s also the potential for monkeypox to spread in respiratory droplets during “prolonged” contact between people.
Symptoms can start out flu-like, with a fever, aches and swollen lymph nodes. After a few days, a rash appears that may spread — although in some recent cases, doctors have seen a more subtle rash with just a few sores in one area of the body.
In Alberta, if you think you’ve been in close contact with someone with monkeypox, or are having symptoms of the disease, you should self-isolate and call 811 or tell your doctor. The infection typically resolves after a few weeks, but the rash can be very painful and cause scarring.
While people should get checked if they think they have a reason to worry, the risk in this province is low.
“That’s not to say that, in the aggregate and from the perspective of global health, this isn’t a serious issue and something that deserves intense scrutiny,” Caulfield said.
“But on that individual risk level right now, I don’t think the average Albertan needs to be too concerned.”
Canada’s deputy chief public health officer Howard Njoo has said that the entire Canadian population is likely susceptible to monkeypox because routine vaccination against smallpox stopped in 1972.
But that doesn’t mean we’re in for a new monkeypox pandemic. It’s much less infectious than COVID, especially when compared to the Omicron variant.
According to the Public Health Agency of Canada (PHAC), the country has a small stockpile of three types of smallpox vaccine that can also work against monkeypox, including a newer vaccine that has far fewer side effects than the shots people would have had before routine immunization stopped.
In Quebec, where there are currently more than 70 confirmed cases of monkeypox, the province is giving access to the vaccine to high-risk contacts of a confirmed or probable monkeypox case. PHAC has said they’re watching the situation closely, but a mass vaccination campaign isn’t necessary at the moment.
Evans said past history of monkeypox outbreaks have historically been small and limited, and there’s more work ahead to find out what’s happening this time
“I think that it’s more the epidemiology of how it got into a particular population and then got spread. That is the difference in this particular case.”
— With files from The Canadian Press
masmith@postmedia.com
twitter.com/meksmith

The Canadian government says it will donate up to 200,000 vaccine doses to fight the mpox outbreak in Congo and other African countries.
It says the donated doses of Imvamune will come from Canada’s existing supply and will not affect the country’s preparedness for mpox cases in this country.
Minister of Health Mark Holland says the donation “will help to protect those in the most affected regions of Africa and will help prevent further spread of the virus.”
Dr. Madhukar Pai, Canada research chair in epidemiology and global health, says although the donation is welcome, it is a very small portion of the estimated 10 million vaccine doses needed to control the outbreak.
Vaccine donations from wealthier countries have only recently started arriving in Africa, almost a month after the World Health Organization declared the mpox outbreak a public health emergency of international concern.
A few days after the declaration in August, Global Affairs Canada announced a contribution of $1 million for mpox surveillance, diagnostic tools, research and community awareness in Africa.
On Thursday, the Africa Centres for Disease Control and Prevention said mpox is still on the rise and that testing rates are “insufficient” across the continent.
Jason Kindrachuk, Canada research chair in emerging viruses at the University of Manitoba, said donating vaccines, in addition to supporting surveillance and diagnostic tests, is “massively important.”
But Kindrachuk, who has worked on the ground in Congo during the epidemic, also said that the international response to the mpox outbreak is “better late than never (but) better never late.”
“It would have been fantastic for us globally to not be in this position by having provided doses a much, much longer time prior than when we are,” he said, noting that the outbreak of clade I mpox in Congo started in early 2023.
Clade II mpox, endemic in regions of West Africa, came to the world’s attention even earlier — in 2022 — as that strain of virus spread to other countries, including Canada.
Two doses are recommended for mpox vaccination, so the donation may only benefit 100,000 people, Pai said.
Pai questioned whether Canada is contributing enough, as the federal government hasn’t said what percentage of its mpox vaccine stockpile it is donating.
“Small donations are simply not going to help end this crisis. We need to show greater solidarity and support,” he said in an email.
“That is the biggest lesson from the COVID-19 pandemic — our collective safety is tied with that of other nations.”
This report by The Canadian Press was first published Sept. 13, 2024.
Canadian Press health coverage receives support through a partnership with the Canadian Medical Association. CP is solely responsible for this content.
The Canadian Press. All rights reserved.

HALIFAX – The Nova Scotia government says it could be months before it reveals how many people are on the wait-list for a family doctor.
The head of the province’s health authority told reporters Wednesday that the government won’t release updated data until the 160,000 people who were on the wait-list in June are contacted to verify whether they still need primary care.
Karen Oldfield said Nova Scotia Health is working on validating the primary care wait-list data before posting new numbers, and that work may take a matter of months. The most recent public wait-list figures are from June 1, when 160,234 people, or about 16 per cent of the population, were on it.
“It’s going to take time to make 160,000 calls,” Oldfield said. “We are not talking weeks, we are talking months.”
The interim CEO and president of Nova Scotia Health said people on the list are being asked where they live, whether they still need a family doctor, and to give an update on their health.
A spokesperson with the province’s Health Department says the government and its health authority are “working hard” to turn the wait-list registry into a useful tool, adding that the data will be shared once it is validated.
Nova Scotia’s NDP are calling on Premier Tim Houston to immediately release statistics on how many people are looking for a family doctor. On Tuesday, the NDP introduced a bill that would require the health minister to make the number public every month.
“It is unacceptable for the list to be more than three months out of date,” NDP Leader Claudia Chender said Tuesday.
Chender said releasing this data regularly is vital so Nova Scotians can track the government’s progress on its main 2021 campaign promise: fixing health care.
The number of people in need of a family doctor has more than doubled between the 2021 summer election campaign and June 2024. Since September 2021 about 300 doctors have been added to the provincial health system, the Health Department said.
“We’ll know if Tim Houston is keeping his 2021 election promise to fix health care when Nova Scotians are attached to primary care,” Chender said.
This report by The Canadian Press was first published Sept. 11, 2024.
The Canadian Press. All rights reserved.

ST. JOHN’S, N.L. – Newfoundland and Labrador‘s chief medical officer is monitoring the rise of whooping cough infections across the province as cases of the highly contagious disease continue to grow across Canada.
Dr. Janice Fitzgerald says that so far this year, the province has recorded 230 confirmed cases of the vaccine-preventable respiratory tract infection, also known as pertussis.
Late last month, Quebec reported more than 11,000 cases during the same time period, while Ontario counted 470 cases, well above the five-year average of 98. In Quebec, the majority of patients are between the ages of 10 and 14.
Meanwhile, New Brunswick has declared a whooping cough outbreak across the province. A total of 141 cases were reported by last month, exceeding the five-year average of 34.
The disease can lead to severe complications among vulnerable populations including infants, who are at the highest risk of suffering from complications like pneumonia and seizures. Symptoms may start with a runny nose, mild fever and cough, then progress to severe coughing accompanied by a distinctive “whooping” sound during inhalation.
“The public, especially pregnant people and those in close contact with infants, are encouraged to be aware of symptoms related to pertussis and to ensure vaccinations are up to date,” Newfoundland and Labrador’s Health Department said in a statement.
Whooping cough can be treated with antibiotics, but vaccination is the most effective way to control the spread of the disease. As a result, the province has expanded immunization efforts this school year. While booster doses are already offered in Grade 9, the vaccine is now being offered to Grade 8 students as well.
Public health officials say whooping cough is a cyclical disease that increases every two to five or six years.
Meanwhile, New Brunswick’s acting chief medical officer of health expects the current case count to get worse before tapering off.
A rise in whooping cough cases has also been reported in the United States and elsewhere. The Pan American Health Organization issued an alert in July encouraging countries to ramp up their surveillance and vaccination coverage.
This report by The Canadian Press was first published Sept. 10, 2024.
The Canadian Press. All rights reserved.


Dolphins will bring in another quarterback, while Tagovailoa deals with concussion
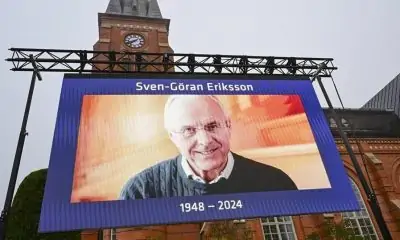

David Beckham among soccer dignitaries attending ex-England coach Sven-Goran Eriksson’s funeral


Vancouver Whitecaps cautious of lowly San Jose Earthquakes


Edmonton Oilers sign defenceman Travis Dermott to professional tryout


Alberta town adopts new resident code of conduct to address staff safety


United Airlines will offer free internet on flights using service from Elon Musk’s SpaceX


Kirk’s walk-off single in 11th inning lifts Blue Jays past Cardinals 4-3


Unifor says workers at Walmart warehouse in Mississauga, Ont., vote to join union