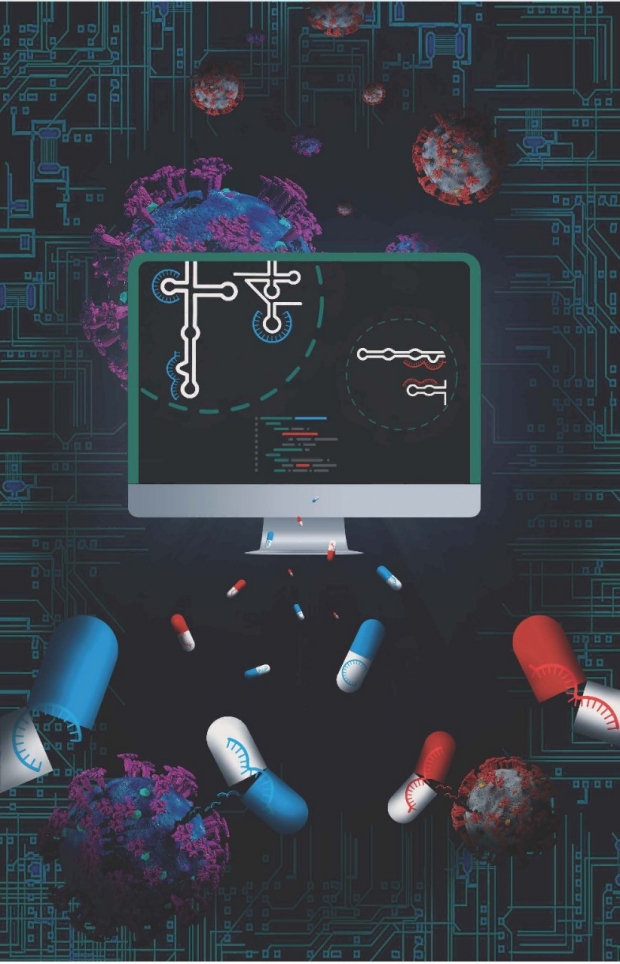
Glenn and Hagey wondered if antiviral drugs targeting more mundane, but equally important, steps in the viral life cycle could stop or slow infections — genome packaging, for example. After all, packing may be boring, but it’s key to a successful trip, whether you’re going to Paris or to the cell next door. And it can be surprisingly complex.
The genome of influenza A virus, for instance, consists of eight separate, single-stranded RNA segments. Each segment folds on itself in a bespoke combination of stems and loops dictated by the sequence of their building blocks, called nucleotides. Viral protein butlers then collaborate to tidily tuck one of each of the eight segments into an outer shell, much the way parents fit a college-bound child’s belongings into the back of the car. The new viral particle is then ready for its maiden voyage to continue the cycle of infection. Other viruses have other packing requirements. But once a successful blueprint has been committed to memory, it is unlikely to be jettisoned, and it is shared among family members like a favorite recipe.
The researchers used a type of analysis called SHAPE and computational modeling to identify a segment of RNA called PSL2 with a predicted three-dimensional structure that is nearly 100% identical among various seasonal and pandemic influenza A strains. When they mutated the sequence of PSL2, the virus was unable to infect cells grown in the laboratory — confirming the importance of the region to viral replication.
Hagey and her colleagues then designed several short stretches of single-stranded DNA that would recognize and bind to matching sequences on PSL2 — latching onto and interfering with its ability to contort itself into the precisely defined shape necessary for successful packing. They designed the DNA pieces to resist degradation and last longer in the body using a technique called locked nucleic acids, or LNAs.
Nowhere to go
The researchers found that treating the laboratory-grown cells with certain LNAs either before or after infection with an influenza strain called H1N1, or swine flu, dramatically reduced the ability of the virus to make new infectious particles. Additionally, they saw no signs of the virus mutating to escape the effects of the LNA even after several generations. In contrast, when they treated the cells with Tamiflu, the virus quickly altered its genome to sidestep the anti-influenza drug, which inhibits the activity of a viral protein that facilitates the release of new viral particles from an infected cell.
“We found that if we design drugs against these highly conserved structures necessary for viral genome packaging, there are very few ways the virus can escape,” Glenn said. “This structure is shared in every known isolate of influenza A, including bird flu and swine flu. So, if we are able to translate these findings into humans, it’s possible we could see universal protection with just one dose.”
The researchers then tested whether laboratory mice would be protected against influenza infection by the most effective LNA. They found that a single dose of the antiviral administered in the animals’ noses one week before exposure to a lethal dose of the virus protected 100% of the treated animals from death. In contrast, the control animals became severely ill and were all humanely sacrificed by day six. They then increased the dose of the LNA and administered it two weeks before virus exposure. Again, none of the mice died, and most were only mildly ill.
Finally, the researchers explored whether the low-level viral replication experienced by the mice in the first series of experiments could protect them from future infection. Sixty-five days after their initial infection, the researchers exposed the same mice again, but with 10 times the normal lethal dose.
“They didn’t bat an eye,” Glenn said. “They didn’t lose weight or appear sick at all. This indicates their initial exposure led to enough residual viral replication to stimulate a broad immune response that remains protective months later.”
A check on COVID-19
The researchers conducted a similar series of experiments with the SARS-CoV-2 virus. As with influenza, they found that LNAs targeting highly conserved structured regions important in the viral genome inhibited the replication of the virus in human cells grown in the laboratory. Even a highly mutated version of the SARS-CoV-2 virus isolated from a chronically infected cancer patient was unable to replicate in the presence of the antiviral.
The protective effect extended to Syrian hamsters, an animal commonly used to study SARS-CoV-2 infection. Hamsters given two single daily sniffs of the LNA before romping with infected peers remained healthy and, after four days, had dramatically less virus in their lungs than control animals.
The researchers are now testing the approach in pigs, using the same dose and intra-nasal applicators they hope to one day use in humans. They foresee a time during the next pandemic when strategically designed LNAs, which they term programmable antivirals, could be used to treat already infected people, to protect people during the lag between vaccination and the development of protective immunity, or to provide prophylactic protection if there is no available vaccine.
“COVID-19 caught us with our pants down,” Glenn said. “But what really keeps me up at night is the likelihood of a highly pathogenic virus like the 1918 influenza pandemic or a new, weaponized version of influenza. Today we have nothing to stop its spread, and a virus like that could kill hundreds of millions of people. But our approach could be enacted ahead of time and provide protection against a wide range of viruses.”
Researchers from the University of North Carolina at Chapel Hill; Utah State University; the University of Cincinnati College of Medicine; the University of Texas Medical Branch; the National Institute of Allergy and Infectious Diseases; the Chan Zuckerberg Biohub; and the Veterans Administration Medical Center, Palo Alto, also contributed to the study.
The study was supported by the National Institutes of Health (grants 5T32AI007328-24, 5T32DK007056, R56A1111460, U19A1109662, RO1AI132191 and U19AI171421), the Department of Defense, an influenza Harrington Scholar Innovator grant, a COVID-19 Harrington Scholar Innovator grant, a Mona M. Burgess Stanford Bio-X Interdisciplinary graduate fellowship, Fastgrants and the Dr. Tri Cao Nguyen Fund for Pandemic Preparedness.