Trends in respiratory illnesses in Windsor-Essex and beyond have prompted a joint letter from the region’s health-care leaders urging the public to get flu shots and updated COVID-19 vaccines.
Health
Windsor-Essex health leaders concerned about ‘aggressive’ flu season, increased respiratory illness

“Today, we are asking residents of this region to once again do their part to address the spread of these dangerous viruses,” the letter states.
According to the letter, getting an annual flu shot and staying up to date on COVID-19 vaccination are “simple and effective ways” to limit the spread of illness, putting less burden on the Windsor-Essex health care system.
“Coughs, fever, chills, runny noses,” Nesathurai said.
Among emergency department patients between the ages 11 and 18, a third of them are there due to respiratory illness.
Among emergency patients under the age of four, half of them are cases of respiratory illness.
“You have to remember, we were closed down in January of this year,” Musyj told the Star. “We’ve been coming out of that. That’s why the pandemic issue is dramatic. A lot of toddlers haven’t been exposed to any type of viruses for two years.”
Influenza and COVID-19 aren’t the only causes for concern. The U.S. has seen an increase in cases of respiratory syncytial virus (RSV) — a common winter virus that causes mild cold-like symptoms in healthy individuals, but is potentially dangerous to infants and the elderly.
“We’re seeing increased demands in our paediatric area, for sure,” said Musyj, noting that WRH has been taking in patients from other parts of the province where hospital systems are even more burdened.
“Right now, Ottawa, GTA (Greater Toronto Area), and Kitchener-Waterloo are struggling — more so than Windsor-Essex,” Musyj said.
“It could be worse (locally). Unfortunately, it’s probably where we’re heading.”
“That’s been escalated to now,” Musyj told the Star. “It’s really starting now.”
Flu shots are available for all Ontario residents who are older than six months of age.
The bivalent COVID-19 vaccine — meant to target the now dominant Omicron variant — is now available to all Ontario residents ages 12 and older.
The Windsor-Essex vaccination rate for COVID-19 booster shots remains below the provincial average.
While 80.9 per cent of all residents in the region have received at least two doses of COVID-19 vaccine, only 16.4 per cent have received a fourth dose — and there has been little change to the statistics over the past four months.
Health
Canada to donate up to 200,000 vaccine doses to combat mpox outbreaks in Africa

The Canadian government says it will donate up to 200,000 vaccine doses to fight the mpox outbreak in Congo and other African countries.
It says the donated doses of Imvamune will come from Canada’s existing supply and will not affect the country’s preparedness for mpox cases in this country.
Minister of Health Mark Holland says the donation “will help to protect those in the most affected regions of Africa and will help prevent further spread of the virus.”
Dr. Madhukar Pai, Canada research chair in epidemiology and global health, says although the donation is welcome, it is a very small portion of the estimated 10 million vaccine doses needed to control the outbreak.
Vaccine donations from wealthier countries have only recently started arriving in Africa, almost a month after the World Health Organization declared the mpox outbreak a public health emergency of international concern.
A few days after the declaration in August, Global Affairs Canada announced a contribution of $1 million for mpox surveillance, diagnostic tools, research and community awareness in Africa.
On Thursday, the Africa Centres for Disease Control and Prevention said mpox is still on the rise and that testing rates are “insufficient” across the continent.
Jason Kindrachuk, Canada research chair in emerging viruses at the University of Manitoba, said donating vaccines, in addition to supporting surveillance and diagnostic tests, is “massively important.”
But Kindrachuk, who has worked on the ground in Congo during the epidemic, also said that the international response to the mpox outbreak is “better late than never (but) better never late.”
“It would have been fantastic for us globally to not be in this position by having provided doses a much, much longer time prior than when we are,” he said, noting that the outbreak of clade I mpox in Congo started in early 2023.
Clade II mpox, endemic in regions of West Africa, came to the world’s attention even earlier — in 2022 — as that strain of virus spread to other countries, including Canada.
Two doses are recommended for mpox vaccination, so the donation may only benefit 100,000 people, Pai said.
Pai questioned whether Canada is contributing enough, as the federal government hasn’t said what percentage of its mpox vaccine stockpile it is donating.
“Small donations are simply not going to help end this crisis. We need to show greater solidarity and support,” he said in an email.
“That is the biggest lesson from the COVID-19 pandemic — our collective safety is tied with that of other nations.”
This report by The Canadian Press was first published Sept. 13, 2024.
Canadian Press health coverage receives support through a partnership with the Canadian Medical Association. CP is solely responsible for this content.
The Canadian Press. All rights reserved.
Health
How many Nova Scotians are on the doctor wait-list? Number hit 160,000 in June

HALIFAX – The Nova Scotia government says it could be months before it reveals how many people are on the wait-list for a family doctor.
The head of the province’s health authority told reporters Wednesday that the government won’t release updated data until the 160,000 people who were on the wait-list in June are contacted to verify whether they still need primary care.
Karen Oldfield said Nova Scotia Health is working on validating the primary care wait-list data before posting new numbers, and that work may take a matter of months. The most recent public wait-list figures are from June 1, when 160,234 people, or about 16 per cent of the population, were on it.
“It’s going to take time to make 160,000 calls,” Oldfield said. “We are not talking weeks, we are talking months.”
The interim CEO and president of Nova Scotia Health said people on the list are being asked where they live, whether they still need a family doctor, and to give an update on their health.
A spokesperson with the province’s Health Department says the government and its health authority are “working hard” to turn the wait-list registry into a useful tool, adding that the data will be shared once it is validated.
Nova Scotia’s NDP are calling on Premier Tim Houston to immediately release statistics on how many people are looking for a family doctor. On Tuesday, the NDP introduced a bill that would require the health minister to make the number public every month.
“It is unacceptable for the list to be more than three months out of date,” NDP Leader Claudia Chender said Tuesday.
Chender said releasing this data regularly is vital so Nova Scotians can track the government’s progress on its main 2021 campaign promise: fixing health care.
The number of people in need of a family doctor has more than doubled between the 2021 summer election campaign and June 2024. Since September 2021 about 300 doctors have been added to the provincial health system, the Health Department said.
“We’ll know if Tim Houston is keeping his 2021 election promise to fix health care when Nova Scotians are attached to primary care,” Chender said.
This report by The Canadian Press was first published Sept. 11, 2024.
The Canadian Press. All rights reserved.
Health
Newfoundland and Labrador monitoring rise in whooping cough cases: medical officer

ST. JOHN’S, N.L. – Newfoundland and Labrador‘s chief medical officer is monitoring the rise of whooping cough infections across the province as cases of the highly contagious disease continue to grow across Canada.
Dr. Janice Fitzgerald says that so far this year, the province has recorded 230 confirmed cases of the vaccine-preventable respiratory tract infection, also known as pertussis.
Late last month, Quebec reported more than 11,000 cases during the same time period, while Ontario counted 470 cases, well above the five-year average of 98. In Quebec, the majority of patients are between the ages of 10 and 14.
Meanwhile, New Brunswick has declared a whooping cough outbreak across the province. A total of 141 cases were reported by last month, exceeding the five-year average of 34.
The disease can lead to severe complications among vulnerable populations including infants, who are at the highest risk of suffering from complications like pneumonia and seizures. Symptoms may start with a runny nose, mild fever and cough, then progress to severe coughing accompanied by a distinctive “whooping” sound during inhalation.
“The public, especially pregnant people and those in close contact with infants, are encouraged to be aware of symptoms related to pertussis and to ensure vaccinations are up to date,” Newfoundland and Labrador’s Health Department said in a statement.
Whooping cough can be treated with antibiotics, but vaccination is the most effective way to control the spread of the disease. As a result, the province has expanded immunization efforts this school year. While booster doses are already offered in Grade 9, the vaccine is now being offered to Grade 8 students as well.
Public health officials say whooping cough is a cyclical disease that increases every two to five or six years.
Meanwhile, New Brunswick’s acting chief medical officer of health expects the current case count to get worse before tapering off.
A rise in whooping cough cases has also been reported in the United States and elsewhere. The Pan American Health Organization issued an alert in July encouraging countries to ramp up their surveillance and vaccination coverage.
This report by The Canadian Press was first published Sept. 10, 2024.
The Canadian Press. All rights reserved.
-

 Sports18 hours ago
Sports18 hours agoDolphins will bring in another quarterback, while Tagovailoa deals with concussion
-

 Sports20 hours ago
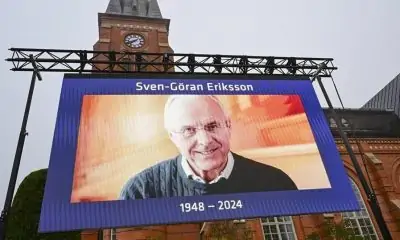
Sports20 hours agoDavid Beckham among soccer dignitaries attending ex-England coach Sven-Goran Eriksson’s funeral
-

 News20 hours ago
News20 hours agoVancouver Whitecaps cautious of lowly San Jose Earthquakes
-

 Sports14 hours ago
Sports14 hours agoEdmonton Oilers sign defenceman Travis Dermott to professional tryout
-

 News20 hours ago
News20 hours agoAlberta town adopts new resident code of conduct to address staff safety
-

 Tech16 hours ago
Tech16 hours agoUnited Airlines will offer free internet on flights using service from Elon Musk’s SpaceX
-

 Sports7 hours ago
Sports7 hours agoKirk’s walk-off single in 11th inning lifts Blue Jays past Cardinals 4-3
-

 News19 hours ago
News19 hours agoUnifor says workers at Walmart warehouse in Mississauga, Ont., vote to join union