Health
Alive inside: How do we reach 'vegetative' patients when tests show they're aware of everything – National Post

“The ominous events in the early morning hours of August 12, 1997 led to a tragedy in Lloydminster, Saskatchewan….” – from a Saskatchewan Court of Queen’s Bench ruling issued in 1998.
There was a small band playing at the Dr. Cooke Extended Care Centre’s annual Christmas party this year, and tables laden with shortbread and popcorn curls and Christmas cookies. On one side of the room sat Jeffrey Tremblay and his father, Paul. Jeff has lived at the Lloydminster facility since he was 19 years old. He turns 41 this week.
Jeff can’t move or speak. He has to be tube-fed through his stomach. He’s aware of what’s going on, Paul says, which is remarkable given doctors wrote Jeff off as being trapped in a vegetative state for 16 years. Only Jeff wasn’t vegetative. Roughly 20 per cent of people like Jeff who are assumed to be totally unconscious — no idea of who they are or where they are, unable to exhibit any “willful behaviour” — are actually aware, lingering undetected somewhere in a state between life and nothingness.
New guidelines could help in the search to find them.
It’s not clear how much Jeff knows about the role he’s playing in what some are calling a revolution in the treatment of the catastrophically brain injured. A senseless attack sent Jeff into the unknowable world he now inhabits.
Jeffrey Tremblay and his father Paul in October 2018.
The assault happened after a night out at a bar with friends. Jeff, the kid with the heart of gold and a smile that could light up a room, was beaten into a coma in a fit of jealousy over a girl. His assailant, then 19, six-feet-two-inches tall and weighing 250 pounds, kicked skinny, wiry, 130-pound Jeff in the chest with enough force to propel a football 25 yards. Jeff’s heart went into arrhythmia, starving his brain of oxygen. When he arrived in emergency by ambulance, he had no pulse, no blood pressure, no “respiratory effort,” no movement. His pupils were fixed and dilated. The blow to his chest “at the critical time of the cardiac electrical cycle,” Saskatchewan Court of Queen’s Bench justice Robert Hrabinsky would write, led to “no effective circulation for many minutes.”
Jeff remained comatose for three weeks, until one day Paul, camped out around the clock in Jeff’s hospital room, looked up from his crossword puzzle and saw his son’s wide-open eyes and that great big smile, and thought, ‘Geez, he’s going to be fine.’”
He wasn’t. Jeff was awake, but doctors said his brain injury, his neurological loss, was so extensive, so diffuse he likely had no awareness whatsoever. “It’s tough to hear when a doctor says that. They want you to pull the plug,” Paul said. “I wasn’t prepared to do that.”
Paul didn’t know much about the brain back then but one day he found a story about a neuroscientist named Adrian Owen, a British-born researcher who for years had been using brain scans to reach inside the minds of people considered all but gone, unable to speak or move or signal to the outside world, “I can hear you. I’m in here.”
They want you to pull the plug
Sixteen years after his beating, Jeff was flown to London, where he was slid inside a functional magnetic resonance imaging scanner, or fMRI, which measures brain activity by detecting changes in blood oxygenation and flow, and shown a short Alfred Hitchcock movie — Bang! You’re Dead! Jeff’s brain fired off the same peaks and dips in electrical activity in the frontal and parietal regions of the brain at critical points of the movie that were uncannily identical to healthy volunteers shown the same eight-minute clip. Before then, Jeff had shown no “higher-order” signs of awareness, Owen and his team wrote in the journal PNAS in 2014, no communication in any form. The experiment suggested he was exhibiting executive processing, that he was able to engage in “complex thoughts about real-world events unfolding over time.”
Owen not only reached Jeff. The Western University scientist has used fMRI to help people once diagnosed “vegetative” follow commands, acknowledge where they are and with whom, and answer questions like, “are you in pain,” by decoding their brain activity.
Now, tests that can detect covert consciousness, not just expensive, bulky fMRI, but bedside EEG machines that use small discs on the scalp to measure brain activity, are moving a step closer to routine use. New guidelines from the American Academy of Neurology and other bodies recommend that, where there is any ambiguity or “inconclusive” findings, brain imaging should be used to hunt for emerging signs of consciousness in the brain injured who have no recourse to speech or action — a “milestone” development in the history of brain science, Owen and colleagues wrote in a paper, “Alive Inside,” in the journal Bioethics.
“The problem up until now has been that we develop these techniques, we put them out there, we tell people how to do them and the only patients that benefit are the people who make it into other research institutions,” Owen says. “It hasn’t been incorporated into guidelines for how one treats these patients. And that has now changed.”


Neuroscientist Adrian Owen.
Owen is pushing for the tests to be adopted even more widely, used not just months or years out from a brain injury, but at the front end in the first hours after a traumatic brain injury to help predict which patients might recover from a vegetative state, which ones might benefit from rehabilitation. Most decisions to remove life support — to pull the proverbial “plug” — occur within the first 72 hours after injury. If we can improve prognosis in that group, if we can better understand who might make some recovery, “we can perhaps save some of those lives,” Owen says.
“Maybe a different decision is right for some of those patients.”
Most remarkably, others are testing deep brain stimulation and other interventions to “re-awaken” or hasten awareness in people in minimally conscious states, even years out from their injury.
But the rapidly evolving field is also raising serious ethical challenges, about how we think about consciousness; about false hope and about the existential risks of making people more aware of an existence many would consider a living nightmare.
If someone can modulate their neural activity — communicate via signals from his or her brain — is that a sufficient, or even reliable proxy for speech? And if we find a way to communicate, what, then, do we ask them? Is there anything we can do to make you more comfortable? Is there anything you’d prefer to watch on TV? Do you wish to continue living?
“What is most tantalizing about this prospect is that it would allow a seriously brain-injured patient to express their current wishes, which may well have changed radically in the interval (sometimes decades) before they expressed any premorbid opinion,” Owen wrote this year in the journal Neuron.
“Ultimately, the morally challenging question of whether theirs is a life that is ‘worth living’ is one that could be answered by the patient using fMRI,” he said.


A PET-fMRI machine at the Brain Imaging Centre in Ottawa.
Sophisticated neuroimaging is already being used to involve some “covertly aware” patients in their daily care. But fMRI is expensive, bulky and nowhere near every hospital has one. However, 20 years from now brain-computer interfaces that use electrical signals from the brain to say, manipulate a computer, or move a robotic arm, could be as common as smartphones, Owen wrote.
But this is where things get dicey, says Dr. Judy Illes, Canada Research Chair in neuroethics at the University of British Columbia.
“How reliable is the signal? How do we make sure that it’s the intent of the person, that it hasn’t been hacked and that it is reproducible?” Illes wonders.
When it comes to communicating hunger or pain, it might matter less if the signal is noisy. “It’s not good to overmedicate someone but it’s much worse to under-medicate,” Illes says.
But could the signals be used in a courtroom as a form of testimony? To redirect an inheritance from the children who don’t visit anymore, to a nurse? Enable a person to request a medically assisted death?
Individuals who we thought were in a persistent vegetative state may not be and, in some cases, certainly are not
And what good is the information that a loved one appears to have some conscious processing, if there’s little available to help them? “I think that’s where I get stuck,” Illes says.
This much is true. “The technology has advanced to the point that we must attend to the fact that individuals who we thought were in a persistent vegetative state may not be and, in some cases, certainly are not. And those numbers are bigger than we ever thought,” she says.
Today, the standard way of checking for any “residual” or preserved awareness or cognitive function in brains damaged by a stroke, cardiac arrest or bash to the head are bedside scales that use response and command-following tasks — look this way or that, squeeze my hand, move a foot, follow the tennis ball with your eyes.
However, people diagnosed as being in a vegetative state, or the much larger group known as the minimally conscious, simply can’t marshal the resources to, say, blink an eye, or move a foot on command. It’s not a muscular problem. They aren’t paralyzed. Rather, there’s a central nervous system problem, a disconnection that’s preventing them from executing any movement at all, Owen says. But their thoughts, their mental process could be intact.
These people do spontaneously move. They often grunt; they’ll open their eyes or move a hand. The problem is knowing whether that’s a conscious response or merely chance.
Except in circumstances such as complete brain death, relying on neurological exams at the beside is, in many cases, “hopelessly unreliable,” Owen says.


Images of “healthy” vs. “vegetative brains.”
Brain imaging takes behaviour out of the equation.
In a ground-breaking Science paper published in 2006, Owen and colleagues reported that an apparently vegetative woman showed distinct patterns of brain activity when asked, while lying inside a fMRI, to imagine herself playing tennis, or walking through the rooms of her house. The pattern of her brain activity was indistinguishable from what is seen in healthy volunteers. Owen believes she was entirely aware during the scanning procedure.
Next, working with Steven Laureys from the University of Liege, Owen showed that, of 54 patients in a vegetative or minimally conscious state, five 5 were able to “willfully modulate” their brain activity. One was able to answer yes or no to questions during functional MRI even though it remained impossible to establish any form of communication at the bedside. Then, in an experiment that made worldwide headlines, the team slid a man named Scott Routley inside an fMRI scanner and asked if he was in pain. The Sarnia, Ont. man had remained in what doctors were convinced was a vegetative state for 12 years after a police cruiser rushing to the scene of a crime slammed into his car in December 1999. Lying inside the scanner, Scott was told to imagine walking around his house if the answer was “yes” or playing tennis if the answer was “no.” “Do any parts of your body hurt right now,” Owen asked Routley. The answer was, no.


Images of “healthy” vs. “vegetative brains.”
Since then, Owen and his team have used imaging to ask patients if they prefer the temperature lower or higher, whether they still like watching hockey. “One of the sad truths is that they get exposed to an awful lot of whatever it is they used to like before they had a brain injury,” Owen says. “If you were a great lover of Celine Dion 20 years ago when you had your brain injury, maybe you don’t want to listen to that anymore. We can return a little autonomy to patients.”
Ironically, they’re often relatively healthy. They breathe on their own. Their hearts beat on their own. They’re not being kept alive, except, like Jeff Tremblay, they have to be fed and hydrated. There’s no “plug’ to pull. They can only die by withdrawing nutrition and hydration.
The better their responses in the fMRI scanner, the more likely they are to recover, Owen believes. And there have been some spectacular cases of recovery, including Juan Torres, to whom Owen devotes an entire chapter of his book, Into the Gray Zone. The Toronto-area man suffered a catastrophic brain injury when he was 19 years old. Today, six years out, he has re-enrolled in school. “He’s intellectually right back to where he was before,” Owen says.
But Juan is truly the exception. “People often think these people go from being in a vegetative state to being back on the golf course. That almost never happens,’ Owen says.
We’ve got patients who we know are on the edge of being able to establish communication
However, he and others are starting to think about interventions that might accelerate their return to consciousness, even a normal life. “Twenty years ago, people would say to me, ‘isn’t there some sort of surgery you could do to fix these patients?
“Well, maybe, but we didn’t know where to start. You need the basic imaging and you need to understand what’s causing the problem before you can solve the problem of how to fix people. And I think we’re getting there. We’re just at the tipping point right now,” Owen says.
Researchers are testing different drug therapies, including anti-virals as well as a sleeping pill called zolpidem that famously and transiently roused Louis Viljoen, of Johannesburg, from a vegetative state in 2006. Twenty minutes after his first dose, he opened his eyes, looked at his mother and said, “Hello mummy.” More recently, in October, British scientists floated the idea of using the psychedelic psilocybin, the active substance in magic mushrooms, the idea being the hallucinogen might increase brain complexity and brain plasticity — the brain’s ability to rewire itself, and grow new neurons.
The biggest hope, however, may rest with deep-brain stimulation, or DBS. Dr. Nicholas Schiff is a neuroscientist at Weill Cornell Medicine in New York City. Schiff was also the lead author of a breakthrough study published in Nature in 2007 involving a 38-year-old man who had spent more than five years in a minimally conscious state who can now communicate with his family, thanks to pulses of electric current to his brain.
By stimulating the central thalamus, which relays motor and sensory signals to the cerebral cortex, the part of the brain involved in consciousness, Schiff’s team was able to help the man name objects, make hand gestures and eat without a feeding tube — suggesting DBS “can promote significant late functional recovery from severe traumatic brain injury” even years after the injury occurred.
“We’ve got patients who we know are on the edge of being able to establish communication, but we don’t really know what to do for them yet,” says Schiff, adding that it’s a population of patients that has been horribly neglected for years.
“Just because we identify consciousness and awareness, it’s not enough. It’s terrible to know we can make these measurements, identify awareness and not be doing what needs to be done, which is to build a medical infrastructure to support these people.”
But how quickly should we be moving? And is there a risk of overestimating what fMRI mental imagery really means? The fact this area is so fraught with ethical challenges is precisely because we don’t know what it’s like to be in such a state, or whether a person’s mental processes are functioning at full capacity. A signal is one thing. But what does it mean?
“I’ve always imagined a clinician entering a room and saying, ‘I have wonderful news! John is aware! We know this because he’s volitionally modulating his brain activity,” Andrew Peterson, an assistant professor at George Mason University, who works with Owen’s lab, wrote in an email.
“My gut tells me that families might not know what to do with this information. What they will want to know is whether their loved one can hear their voices, feel their touch, or if he or she is experiencing pain.” However, the tests aren’t pitch perfect. Accuracy rates range from 60 to 80 per cent.


The Tremblay family in October 2018.
What’s more, to truly tap into a person’s state of mind requires a rich, two-way conversation, and the current technology, whether fMRI or less cumbersome, bedside EEG machines, prevents that, Peterson said. Such deeply profound decisions as “do you wish to stop being fed or hydrated” couldn’t be handled, legally or ethically, as if it were a “yes” or “no” game of 20 Questions.
A more likely scenario is how brain imaging might influence legal fights around decisions to withdraw life support.
Consider this example, Peterson says: A person’s advance directive states, “I don’t want to live if I’m in a vegetative state.” But then brain imaging detects covert consciousness. “One family member thinks that this clearly shows that the patient is not in a vegetative state and they shouldn’t withdraw care,” Peterson said. Other family members insist any detection of “covert” consciousness is irrelevant because their son or daughter or spouse could remain in that brain state for the rest of his or her life.
And it’s mostly young people who are most likely to end up with disorders of consciousness. Young people are resilient, Peterson says. They don’t die from the initial injury. Instead, they’re left in that grey zone between consciousness and unconsciousness.
And it’s impossible to know what their interior lives might be like. Some people might be relieved to learn their loved one can hear, can process speech, that they are fully aware of everything that is going on around them. Others will be horrified, and left with gut-wrenching questions about quality of life.
My gut tells me that families might not know what to do with this information
Still, the harms associated with undetected consciousness, whether it’s unnecessary pain or prematurely withdrawing care, is just too great not to starting moving the research into practice, Peterson said. “At the very least, it seems that clinicians have an ethical duty to discuss this option with families” in appropriate cases.
Before he took his son to Owen’s London lab, “everything was a dark hole,” Paul Tremblay says. “Everything was negative, negative, negative.”
“But the more you read about it, it’s just not true.”
Jeff can’t communicate. But Paul reads his eyes, to see if he’s listening or not. He smiles when he’s happy, grimaces when he’s sad, groans when he’s in pain. When he’s really tired, like most of us Jeff doesn’t listen very much. Paul takes his son to the movies once a week. He remains in touch with Owen’s lab.
“It might not help Jeff, in the long run,” Paul said. “But I think Jeff is helping the research.”
In 1998, Jeff Tremblay’s attacker was convicted of aggravated assault.
He served eight months of a three-year prison sentence.
• Email: skirkey@postmedia.com | Twitter: sharon_kirkey
Health
Toronto reports 2 more measles cases. Use our tool to check the spread in Canada – Toronto Star


/* OOVVUU Targeting */
const path = ‘/news/canada’;
const siteName = ‘thestar.com’;
let domain = ‘thestar.com’;
if (siteName === ‘thestar.com’)
domain = ‘thestar.com’;
else if (siteName === ‘niagarafallsreview.ca’)
domain = ‘niagara_falls_review’;
else if (siteName === ‘stcatharinesstandard.ca’)
domain = ‘st_catharines_standard’;
else if (siteName === ‘thepeterboroughexaminer.com’)
domain = ‘the_peterborough_examiner’;
else if (siteName === ‘therecord.com’)
domain = ‘the_record’;
else if (siteName === ‘thespec.com’)
domain = ‘the_spec’;
else if (siteName === ‘wellandtribune.ca’)
domain = ‘welland_tribune’;
else if (siteName === ‘bramptonguardian.com’)
domain = ‘brampton_guardian’;
else if (siteName === ‘caledonenterprise.com’)
domain = ‘caledon_enterprise’;
else if (siteName === ‘cambridgetimes.ca’)
domain = ‘cambridge_times’;
else if (siteName === ‘durhamregion.com’)
domain = ‘durham_region’;
else if (siteName === ‘guelphmercury.com’)
domain = ‘guelph_mercury’;
else if (siteName === ‘insidehalton.com’)
domain = ‘inside_halton’;
else if (siteName === ‘insideottawavalley.com’)
domain = ‘inside_ottawa_valley’;
else if (siteName === ‘mississauga.com’)
domain = ‘mississauga’;
else if (siteName === ‘muskokaregion.com’)
domain = ‘muskoka_region’;
else if (siteName === ‘newhamburgindependent.ca’)
domain = ‘new_hamburg_independent’;
else if (siteName === ‘niagarathisweek.com’)
domain = ‘niagara_this_week’;
else if (siteName === ‘northbaynipissing.com’)
domain = ‘north_bay_nipissing’;
else if (siteName === ‘northumberlandnews.com’)
domain = ‘northumberland_news’;
else if (siteName === ‘orangeville.com’)
domain = ‘orangeville’;
else if (siteName === ‘ourwindsor.ca’)
domain = ‘our_windsor’;
else if (siteName === ‘parrysound.com’)
domain = ‘parrysound’;
else if (siteName === ‘simcoe.com’)
domain = ‘simcoe’;
else if (siteName === ‘theifp.ca’)
domain = ‘the_ifp’;
else if (siteName === ‘waterloochronicle.ca’)
domain = ‘waterloo_chronicle’;
else if (siteName === ‘yorkregion.com’)
domain = ‘york_region’;
let sectionTag = ”;
try
if (domain === ‘thestar.com’ && path.indexOf(‘wires/’) = 0)
sectionTag = ‘/business’;
else if (path.indexOf(‘/autos’) >= 0)
sectionTag = ‘/autos’;
else if (path.indexOf(‘/entertainment’) >= 0)
sectionTag = ‘/entertainment’;
else if (path.indexOf(‘/life’) >= 0)
sectionTag = ‘/life’;
else if (path.indexOf(‘/news’) >= 0)
sectionTag = ‘/news’;
else if (path.indexOf(‘/politics’) >= 0)
sectionTag = ‘/politics’;
else if (path.indexOf(‘/sports’) >= 0)
sectionTag = ‘/sports’;
else if (path.indexOf(‘/opinion’) >= 0)
sectionTag = ‘/opinion’;
} catch (ex)
const descriptionUrl = ‘window.location.href’;
const vid = ‘mediainfo.reference_id’;
const cmsId = ‘2665777’;
let url = `https://pubads.g.doubleclick.net/gampad/ads?iu=/58580620/$domain/video/oovvuu$sectionTag&description_url=$descriptionUrl&vid=$vid&cmsid=$cmsId&tfcd=0&npa=0&sz=640×480&ad_rule=0&gdfp_req=1&output=vast&unviewed_position_start=1&env=vp&impl=s&correlator=`;
url = url.split(‘ ‘).join(”);
window.oovvuuReplacementAdServerURL = url;
Canada has seen a concerning rise in measles cases in the first months of 2024.
By the third week of March, the country had already recorded more than three times the number of cases as all of last year. Canada had just 12 cases of measles in 2023, up from three in 2022.
function buildUserSwitchAccountsForm()
var form = document.getElementById(‘user-local-logout-form-switch-accounts’);
if (form) return;
// build form with javascript since having a form element here breaks the payment modal.
var switchForm = document.createElement(‘form’);
switchForm.setAttribute(‘id’,’user-local-logout-form-switch-accounts’);
switchForm.setAttribute(‘method’,’post’);
switchForm.setAttribute(‘action’,’https://www.thestar.com/tncms/auth/logout/?return=https://www.thestar.com/users/login/?referer_url=https%3A%2F%2Fwww.thestar.com%2Fnews%2Fcanada%2Ftoronto-reports-2-more-measles-cases-use-our-tool-to-check-the-spread-in-canada%2Farticle_20aa7df4-e88f-11ee-8fad-8f8368d7ff53.html’);
switchForm.setAttribute(‘style’,’display:none;’);
var refUrl = document.createElement(‘input’); //input element, text
refUrl.setAttribute(‘type’,’hidden’);
refUrl.setAttribute(‘name’,’referer_url’);
refUrl.setAttribute(‘value’,’https://www.thestar.com/news/canada/toronto-reports-2-more-measles-cases-use-our-tool-to-check-the-spread-in-canada/article_20aa7df4-e88f-11ee-8fad-8f8368d7ff53.html’);
var submit = document.createElement(‘input’);
submit.setAttribute(‘type’,’submit’);
submit.setAttribute(‘name’,’logout’);
submit.setAttribute(‘value’,’Logout’);
switchForm.appendChild(refUrl);
switchForm.appendChild(submit);
document.getElementsByTagName(‘body’)[0].appendChild(switchForm);
function handleUserSwitchAccounts()
window.sessionStorage.removeItem(‘bd-viafoura-oidc’); // clear viafoura JWT token
// logout user before sending them to login page via return url
document.getElementById(‘user-local-logout-form-switch-accounts’).submit();
return false;
buildUserSwitchAccountsForm();
#ont-map-iframepadding:0;width:100%;border:0;overflow:hidden;
#ontario-cases-iframepadding:0;width:100%;border:0;overflow:hidden;
#province-table-iframepadding:0;width:100%;border:0;overflow:hidden;
console.log(‘=====> bRemoveLastParagraph: ‘,0);
Health
Cancer Awareness Month – Métis Nation of Alberta


Cancer Awareness Month
Posted on: Apr 18, 2024
April is Cancer Awareness Month
As we recognize Cancer Awareness Month, we stand together to raise awareness, support those affected, advocate for prevention, early detection, and continued research towards a cure. Cancer is the leading cause of death for Métis women and the second leading cause of death for Métis men. The Otipemisiwak Métis Government of the Métis Nation Within Alberta is working hard to ensure that available supports for Métis Citizens battling cancer are culturally appropriate, comprehensive, and accessible by Métis Albertans at all stages of their cancer journey.
Receiving a cancer diagnosis, whether for yourself or a loved one, can feel overwhelming, leaving you unsure of where to turn for support. In June, our government will be launching the Cancer Supports and Navigation Program which will further support Métis Albertans and their families experiencing cancer by connecting them to OMG-specific cancer resources, external resources, and providing navigation support through the health care system. This program will also include Métis-specific peer support groups for those affected by cancer.
With funding from the Canadian Partnership Against Cancer (CPAC) we have also developed the Métis Cancer Care Course to ensure that Métis Albertans have access to culturally safe and appropriate cancer services. This course is available to cancer care professionals across the country and provides an overview of who Métis people are, our culture, our approaches to health and wellbeing, our experiences with cancer care, and our cancer journey.
Together, we can make a difference in the fight against cancer and ensure equitable access to culturally safe and appropriate care for all Métis Albertans. Please click on the links below to learn more about the supports available for Métis Albertans, including our Compassionate Care: Cancer Transportation program.
I wish you all good health and happiness!
Bobbi Paul-Alook
Secretary of Health & Seniors
Health
Type 2 diabetes is not one-size-fits-all: Subtypes affect complications and treatment options – The Conversation


You may have heard of Ozempic, the “miracle drug” for weight loss, but did you know that it was actually designed as a new treatment to manage diabetes? In Canada, diabetes affects approximately 10 per cent of the general population. Of those cases, 90 per cent have Type 2 diabetes.
This metabolic disorder is characterized by persistent high blood sugar levels, which can be accompanied by secondary health challenges, including a higher risk of stroke and kidney disease.
Locks and keys
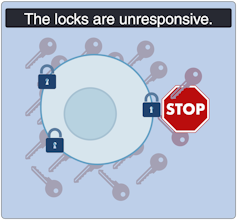
In Type 2 diabetes, the body struggles to maintain blood sugar levels in an acceptable range. Every cell in the body needs sugar as an energy source, but too much sugar can be toxic to cells. This equilibrium needs to be tightly controlled and is regulated by a lock and key system.
In the body’s attempt to manage blood sugar levels and ensure that cells receive the right amount of energy, the pancreatic hormone, insulin, functions like a key. Cells cover themselves with locks that respond perfectly to insulin keys to facilitate the entry of sugar into cells.
Unfortunately, this lock and key system doesn’t always perform as expected. The body can encounter difficulties producing an adequate number of insulin keys, and/or the locks can become stubborn and unresponsive to insulin.
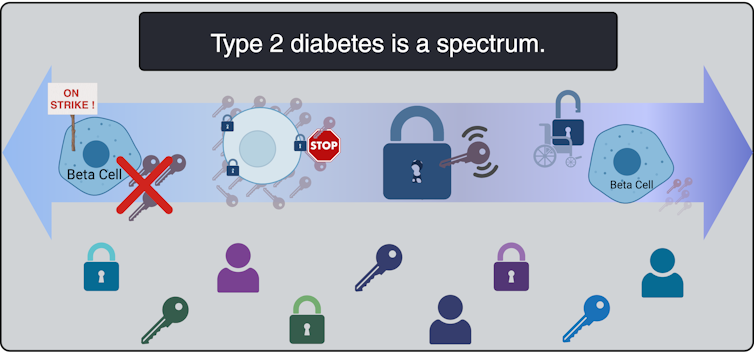
All forms of diabetes share the challenge of high blood sugar levels; however, diabetes is not a singular condition; it exists as a spectrum. Although diabetes is broadly categorized into two main types, Type 1 and Type 2, each presents a diversity of subtypes, especially Type 2 diabetes.
These subtypes carry their own characteristics and risks, and do not respond uniformly to the same treatments.
To better serve people living with Type 2 diabetes, and to move away from a “one size fits all” approach, it is beneficial to understand which subtype of Type 2 diabetes a person lives with. When someone needs a blood transfusion, the medical team needs to know the patient’s blood type. It should be the same for diabetes so a tailored and effective game plan can be implemented.
This article explores four unique subtypes of Type 2 diabetes, shedding light on their causes, complications and some of their specific treatment avenues.
Severe insulin-deficient diabetes: We’re missing keys!
(Lili Grieco-St-Pierre, Jennifer Bruin/Created with BioRender.com)
Insulin is produced by beta cells, which are found in the pancreas. In the severe insulin-deficient diabetes (SIDD) subtype, the key factories — the beta cells — are on strike. Ultimately, there are fewer keys in the body to unlock the cells and allow entry of sugar from the blood.
SIDD primarily affects younger, leaner individuals, and unfortunately, increases the risk of eye disease and blindness, among other complications. Why the beta cells go on strike remains largely unknown, but since there is an insulin deficiency, treatment often involves insulin injections.
Severe insulin-resistant diabetes: But it’s always locked!
(Lili Grieco-St-Pierre, Jennifer Bruin/Created with BioRender.com)
In the severe insulin-resistant diabetes (SIRD) subtype, the locks are overstimulated and start ignoring the keys. As a result, the beta cells produce even more keys to compensate. This can be measured as high levels of insulin in the blood, also known as hyperinsulinemia.
This resistance to insulin is particularly prominent in individuals with higher body weight. Patients with SIRD have an increased risk of complications such as fatty liver disease. There are many treatment avenues for these patients but no consensus about the optimal approach; patients often require high doses of insulin.
Mild obesity-related diabetes: The locks are sticky!

(Lili Grieco-St-Pierre, Jennifer Bruin/Created with BioRender.com)
Mild obesity-related (MOD) diabetes represents a nuanced aspect of Type 2 diabetes, often observed in individuals with higher body weight. Unlike more severe subtypes, MOD is characterized by a more measured response to insulin. The locks are “sticky,” so it is challenging for the key to click in place and open the lock. While MOD is connected to body weight, the comparatively less severe nature of MOD distinguishes it from other diabetes subtypes.
To minimize complications, treatment should include maintaining a healthy diet, managing body weight, and incorporating as much aerobic exercise as possible. This is where drugs like Ozempic can be prescribed to control the evolution of the disease, in part by managing body weight.
Mild age-related diabetes: I’m tired of controlling blood sugar!
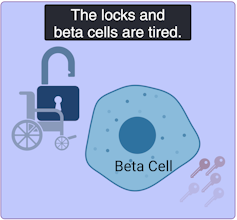
(Lili Grieco-St-Pierre, Jennifer Bruin/Created with BioRender.com)
Mild age-related diabetes (MARD) happens more often in older people and typically starts later in life. With time, the key factory is not as productive, and the locks become stubborn. People with MARD find it tricky to manage their blood sugar, but it usually doesn’t lead to severe complications.
Among the different subtypes of diabetes, MARD is the most common.
Unique locks, varied keys
While efforts have been made to classify diabetes subtypes, new subtypes are still being identified, making proper clinical assessment and treatment plans challenging.
In Canada, unique cases of Type 2 diabetes were identified in Indigenous children from Northern Manitoba and Northwestern Ontario by Dr. Heather Dean and colleagues in the 1980s and 90s. Despite initial skepticism from the scientific community, which typically associated Type 2 diabetes with adults rather than children, clinical teams persisted in identifying this as a distinct subtype of Type 2 diabetes, called childhood-onset Type 2 diabetes.
Read more:
Indigenous community research partnerships can help address health inequities
Childhood-onset Type 2 diabetes is on the rise across Canada, but disproportionately affects Indigenous youth. It is undoubtedly linked to the intergenerational trauma associated with colonization in these communities. While many factors are likely involved, recent studies have discovered that exposure of a fetus to Type 2 diabetes during pregnancy increases the risk that the baby will develop diabetes later in life.
Acknowledging this distinct subtype of Type 2 diabetes in First Nations communities has led to the implementation of a community-based health action plan aimed at addressing the unique challenges faced by Indigenous Peoples. It is hoped that partnered research between communities and researchers will continue to help us understand childhood-onset Type 2 diabetes and how to effectively prevent and treat it.
A mosaic of conditions
(Lili Grieco-St-Pierre, Jennifer Bruin/Created with BioRender.com)
Type 2 diabetes is not uniform; it’s a mosaic of conditions, each with its own characteristics. Since diabetes presents so uniquely in every patient, even categorizing into subtypes does not guarantee how the disease will evolve. However, understanding these subtypes is a good starting point to help doctors create personalized plans for people living with the condition.
While Indigenous communities, lower-income households and individuals living with obesity already face a higher risk of developing Type 2 diabetes than the general population, tailored solutions may offer hope for better management. This emphasizes the urgent need for more precise assessments of diabetes subtypes to help customize therapeutic strategies and management strategies. This will improve care for all patients, including those from vulnerable and understudied populations.
-



 Sports24 hours ago
Sports24 hours agoAuston Matthews denied 70th goal as depleted Leafs lose last regular-season game – Toronto Sun
-
Media4 hours ago
DJT Stock Rises. Trump Media CEO Alleges Potential Market Manipulation. – Barron's
-
Business23 hours ago
BC short-term rental rules take effect May 1 – CityNews Vancouver
-
Media7 hours ago
Trump Media alerts Nasdaq to potential market manipulation from 'naked' short selling of DJT stock – CNBC
-
Art22 hours ago
Collection of First Nations art stolen from Gordon Head home – Times Colonist
-



 Investment23 hours ago
Investment23 hours agoBenjamin Bergen: Why would anyone invest in Canada now? – National Post
-
Media19 hours ago
DJT Stock Jumps. The Truth Social Owner Is Showing Stockholders How to Block Short Sellers. – Barron's
-
Art22 hours ago
Crafting the Painterly Art Style in Eternal Strands – IGN First – IGN






