Health
Avian flu: B.C. government provides update

|
|
Thinking about a turkey with your Christmas dinner? It may be more difficult to find this year as the avian flu infects birds in B.C. and across the country.
Seven farms in Abbotsford and Chilliwack have been quarantined in the past week due to the disease, according to Ray Nickel of B.C. Poultry Industry Emergency Operations. He said it’s suspected at another farm, though the test results are not back yet.
The Canadian Food Inspection Agency says a total of 20 farms in B.C. are currently infected. They are mostly in the Lower Mainland, but also on Vancouver Island and in the Interior.
Nickel said birds are being destroyed at the farms under quarantine, and surveillance has been set up around the sites.
Among those farms where the disease has hit are B.C. hatching egg production and turkey farms.
“Right now, every province has been dealing with the (avian influenza) impact,” said Nickel.
“Turkeys are seemingly more susceptible to avian influenza than some of the other bird species, so they’ve been hit the hardest, so there are some supply issues,” he explained.
B.C.’s agriculture minister said it’s a tough situation, and that the outbreaks on commercial farms are concerning.
“This year’s been a lot more difficult. We haven’t seen the disease pressure get alleviated as we normally would,” said Lana Popham.
The minister said the province has taken a proactive stance, with rules such as requiring commercial growers to keep their flocks indoors.
“I feel confident that we’re going to get on top of this, but currently there is a lot of pressure,” Popham said.
Farmers are feeling that pressure.
“It’s always your fear that something’s going to happen to your flock, and so we’ve been on pins and needles for months already,” said Nickel, who runs his own poultry farm.
About 276,000 birds have been culled in B.C. since the beginning of the outbreak in April, but that number is expected to rise.
“While the recent cases of avian influenza are a challenging situation for the B.C. poultry industry, avian influenza is not a food safety concern,” said the CFIA, in a statement.
“There is no evidence to suggest that poultry meat or eggs could transmit the avian influenza virus to humans. Poultry products from locations under investigation are not permitted to enter the food chain,” the statement reads.
Health
Type 2 diabetes is not one-size-fits-all: Subtypes affect complications and treatment options – The Conversation


You may have heard of Ozempic, the “miracle drug” for weight loss, but did you know that it was actually designed as a new treatment to manage diabetes? In Canada, diabetes affects approximately 10 per cent of the general population. Of those cases, 90 per cent have Type 2 diabetes.
This metabolic disorder is characterized by persistent high blood sugar levels, which can be accompanied by secondary health challenges, including a higher risk of stroke and kidney disease.
Locks and keys
In Type 2 diabetes, the body struggles to maintain blood sugar levels in an acceptable range. Every cell in the body needs sugar as an energy source, but too much sugar can be toxic to cells. This equilibrium needs to be tightly controlled and is regulated by a lock and key system.
In the body’s attempt to manage blood sugar levels and ensure that cells receive the right amount of energy, the pancreatic hormone, insulin, functions like a key. Cells cover themselves with locks that respond perfectly to insulin keys to facilitate the entry of sugar into cells.
Unfortunately, this lock and key system doesn’t always perform as expected. The body can encounter difficulties producing an adequate number of insulin keys, and/or the locks can become stubborn and unresponsive to insulin.
All forms of diabetes share the challenge of high blood sugar levels; however, diabetes is not a singular condition; it exists as a spectrum. Although diabetes is broadly categorized into two main types, Type 1 and Type 2, each presents a diversity of subtypes, especially Type 2 diabetes.
These subtypes carry their own characteristics and risks, and do not respond uniformly to the same treatments.
To better serve people living with Type 2 diabetes, and to move away from a “one size fits all” approach, it is beneficial to understand which subtype of Type 2 diabetes a person lives with. When someone needs a blood transfusion, the medical team needs to know the patient’s blood type. It should be the same for diabetes so a tailored and effective game plan can be implemented.
This article explores four unique subtypes of Type 2 diabetes, shedding light on their causes, complications and some of their specific treatment avenues.
Severe insulin-deficient diabetes: We’re missing keys!
(Lili Grieco-St-Pierre, Jennifer Bruin/Created with BioRender.com)
Insulin is produced by beta cells, which are found in the pancreas. In the severe insulin-deficient diabetes (SIDD) subtype, the key factories — the beta cells — are on strike. Ultimately, there are fewer keys in the body to unlock the cells and allow entry of sugar from the blood.
SIDD primarily affects younger, leaner individuals, and unfortunately, increases the risk of eye disease and blindness, among other complications. Why the beta cells go on strike remains largely unknown, but since there is an insulin deficiency, treatment often involves insulin injections.
Severe insulin-resistant diabetes: But it’s always locked!
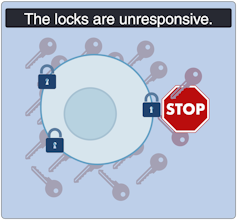
(Lili Grieco-St-Pierre, Jennifer Bruin/Created with BioRender.com)
In the severe insulin-resistant diabetes (SIRD) subtype, the locks are overstimulated and start ignoring the keys. As a result, the beta cells produce even more keys to compensate. This can be measured as high levels of insulin in the blood, also known as hyperinsulinemia.
This resistance to insulin is particularly prominent in individuals with higher body weight. Patients with SIRD have an increased risk of complications such as fatty liver disease. There are many treatment avenues for these patients but no consensus about the optimal approach; patients often require high doses of insulin.
Mild obesity-related diabetes: The locks are sticky!

(Lili Grieco-St-Pierre, Jennifer Bruin/Created with BioRender.com)
Mild obesity-related (MOD) diabetes represents a nuanced aspect of Type 2 diabetes, often observed in individuals with higher body weight. Unlike more severe subtypes, MOD is characterized by a more measured response to insulin. The locks are “sticky,” so it is challenging for the key to click in place and open the lock. While MOD is connected to body weight, the comparatively less severe nature of MOD distinguishes it from other diabetes subtypes.
To minimize complications, treatment should include maintaining a healthy diet, managing body weight, and incorporating as much aerobic exercise as possible. This is where drugs like Ozempic can be prescribed to control the evolution of the disease, in part by managing body weight.
Mild age-related diabetes: I’m tired of controlling blood sugar!
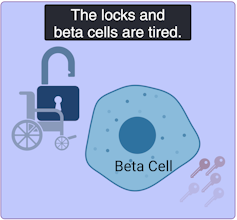
(Lili Grieco-St-Pierre, Jennifer Bruin/Created with BioRender.com)
Mild age-related diabetes (MARD) happens more often in older people and typically starts later in life. With time, the key factory is not as productive, and the locks become stubborn. People with MARD find it tricky to manage their blood sugar, but it usually doesn’t lead to severe complications.
Among the different subtypes of diabetes, MARD is the most common.
Unique locks, varied keys
While efforts have been made to classify diabetes subtypes, new subtypes are still being identified, making proper clinical assessment and treatment plans challenging.
In Canada, unique cases of Type 2 diabetes were identified in Indigenous children from Northern Manitoba and Northwestern Ontario by Dr. Heather Dean and colleagues in the 1980s and 90s. Despite initial skepticism from the scientific community, which typically associated Type 2 diabetes with adults rather than children, clinical teams persisted in identifying this as a distinct subtype of Type 2 diabetes, called childhood-onset Type 2 diabetes.
Read more:
Indigenous community research partnerships can help address health inequities
Childhood-onset Type 2 diabetes is on the rise across Canada, but disproportionately affects Indigenous youth. It is undoubtedly linked to the intergenerational trauma associated with colonization in these communities. While many factors are likely involved, recent studies have discovered that exposure of a fetus to Type 2 diabetes during pregnancy increases the risk that the baby will develop diabetes later in life.
Acknowledging this distinct subtype of Type 2 diabetes in First Nations communities has led to the implementation of a community-based health action plan aimed at addressing the unique challenges faced by Indigenous Peoples. It is hoped that partnered research between communities and researchers will continue to help us understand childhood-onset Type 2 diabetes and how to effectively prevent and treat it.
A mosaic of conditions
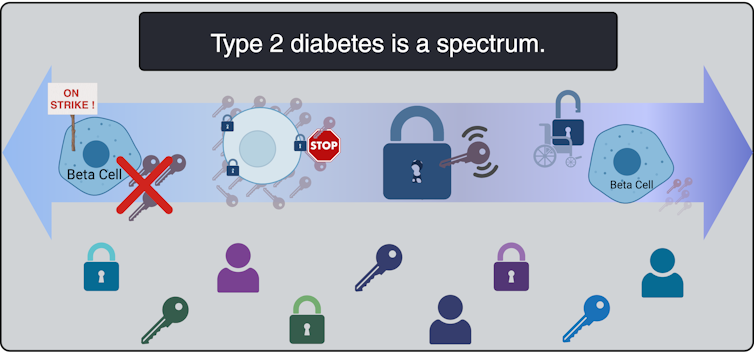
(Lili Grieco-St-Pierre, Jennifer Bruin/Created with BioRender.com)
Type 2 diabetes is not uniform; it’s a mosaic of conditions, each with its own characteristics. Since diabetes presents so uniquely in every patient, even categorizing into subtypes does not guarantee how the disease will evolve. However, understanding these subtypes is a good starting point to help doctors create personalized plans for people living with the condition.
While Indigenous communities, lower-income households and individuals living with obesity already face a higher risk of developing Type 2 diabetes than the general population, tailored solutions may offer hope for better management. This emphasizes the urgent need for more precise assessments of diabetes subtypes to help customize therapeutic strategies and management strategies. This will improve care for all patients, including those from vulnerable and understudied populations.
Health
Quebec successfully pushes back against rise in measles cases – CBC.ca
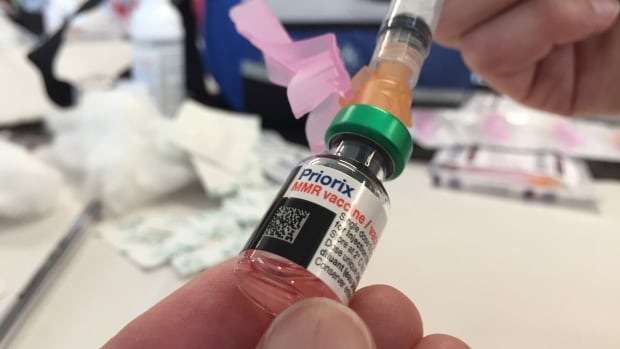
Quebec appears to be winning its battle against the rising tide of measles after 45 cases were confirmed province-wide this year.
“We’ve had no locally transmitted measles cases since March 25, so that’s good news,” said Dr. Paul Le Guerrier, responsible for immunization for Montreal Public Health.
There are 17 patients with measles in Quebec currently, and the most recent case is somebody who was infected while abroad, he said.
But it was no small task to get to this point.
Le Guerrier said once local transmission was detected, news was spread fast among health centres to ensure proper protocols were followed — such as not letting potentially infected people sit in waiting rooms for hours on end.
Then about 90 staffers were put to work, tracking down those who were in contact with positive cases and are not properly vaccinated. They were given post-exposure prophylaxis, which prevents disease, said Le Guerrier.
From there, a vaccination campaign was launched, especially in daycares, schools and neighbourhoods with low inoculation rates. There was an effort to convince parents to get their children vaccinated.
Vaccination in schools boosted
Some schools, mostly in Montreal, had vaccination rates as low as 30 or 40 per cent.
“Vaccination was well accepted and parents responded well,” said Le Guerrier. “Some schools went from very low to as high as 85 to 90 per cent vaccination coverage.”
But it’s not only children who aren’t properly vaccinated. Le Guerrier said people need two doses after age one to be fully inoculated, and he encouraged people to check their status.
There are all kinds of reasons why people aren’t vaccinated, but it’s only about five per cent who are against immunization, he said. So far, some 10,000 people have been vaccinated against measles province-wide during this campaign, Le Guerrier said.
The next step is to continue pushing for further vaccination, but he said, small outbreaks are likely in the future as measles is spreading abroad and travellers are likely to bring it back with them.
Need to improve vaccination rate, expert says
Dr. Donald Vinh, an infectious diseases specialist from the McGill University Health Centre, said it’s not time to rest on our laurels, but this is a good indication that public health is able to take action quickly and that people are willing to listen to health recommendations.
“We are not seeing new cases or at least the new cases are not exceeding the number of cases that we can handle,” said Vinh.
“So these are all reassuring signs, but I don’t think it’s a sign that we need to become complacent.”
Vinh said there are also signs that the public is lagging in vaccine coverage and it’s important to respond to this with improved education and access. Otherwise, microbes capitalize on our weaknesses, he said.
Getting vaccination coverage up to an adequate level is necessary, Vinh said, or more small outbreaks like this will continue to happen.
“And it’s very possible that we may not be able to get one under control if we don’t react quickly enough,” he said.
Health
Pregnant women in the Black Country urged to get whooping cough vaccine – BBC.com


Pregnant women urged to get whooping cough vaccine
Pregnant women in the Black Country are being urged to get vaccinated against whooping cough after a rise in cases.
The bacterial infection of the lungs spreads very easily and can cause serious problems, especially in babies and young children.
The Black Country Integrated Care Board (ICB) is advising pregnant women between 16 and 32 weeks to contact their GP to get the vaccine so their baby has protection from birth.
The UK Health Security Agency warned earlier this year of a steady decline in uptake of the vaccine in pregnant women and children.
Symptoms of the infection, also known as “100-day cough”, are similar to a cold, with a runny nose and sore throat.
Sally Roberts, chief nursing officer for the ICB, which covers Wolverhampton, Dudley, Walsall and Sandwell, said anyone could catch it, but it was more serious for young children and babies.
“Getting vaccinated while you’re pregnant is highly effective in protecting your baby from developing whooping cough in the first few weeks of their life – ideally from 16 weeks up to 32 weeks of pregnancy,” she said.
“If for any reason you miss having the vaccine, you can still have it up until you go into labour.”
Follow BBC West Midlands on Facebook, X and Instagram. Send your story ideas to: newsonline.westmidlands@bbc.co.uk
-



 Science7 hours ago
Science7 hours agoJeremy Hansen – The Canadian Encyclopedia
-



 Investment7 hours ago
Investment7 hours agoUK Mulls New Curbs on Outbound Investment Over Security Risks – BNN Bloomberg
-



 Tech6 hours ago
Tech6 hours agoSave $700 Off This 4K Projector at Amazon While You Still Can – CNET
-



 Health20 hours ago
Health20 hours agoSupervised consumption sites urgently needed, says study – Sudbury.com
-



 Sports5 hours ago
Sports5 hours agoAuston Matthews denied 70th goal as depleted Leafs lose last regular-season game – Toronto Sun
-
Real eState6 hours ago
Sick of Your Blue State? These Real Estate Agents Have Just the Place for You. – The New York Times
-


 Tech5 hours ago
Tech5 hours ago'Kingdom Come: Deliverance II' Revealed In Epic New Trailer And It Looks Incredible – Forbes
-
News20 hours ago
Canada's 2024 budget announces 'halal mortgages'. Here's what to know – National Post





