Health
Red Cross urges action for Papua New Guinea as COVID-19 overwhelms health system
|
|
Concerted international action is needed to support Papua New Guinea as a surge in COVID-19 cases overwhelms the Pacific country’s health system, the International Federation of Red Cross and Red Crescent Societies said on Monday.
Coronavirus cases in the island nation of 9 million have been surging in recent weeks, with 385 new cases recorded on Thursday, according to latest available government data.
There have been 26,731 officially confirmed cases and 329 deaths in the country 150 km (90 miles) north of Australia.
Less than 1% of the population has been fully vaccinated, according to Our World in Data figures, although the government anticipated months ago that it would have enough shots by now for everyone who wanted to be vaccinated.
Misinformation, public apprehension, and logistical challenges with the rollout have slowed down vaccinations, the Red Cross said.
“Urgent efforts and further support are needed in healthcare to prevent a massive loss of life in the coming days and weeks,” Uvenama Rova, PNG Red Cross secretary general, said in a statement.
According to the PNG National Control Centre for COVID-19, all major hospitals have been hit with rising cases.
“We’re at the moment barely managing with the existing load,” Gary Nou, team leader for Emergency Medical Team at the National Centre, was quoted as saying last week in a statement on the centre’s website.
A medical team from Australia arrived in Port Moresby this month, and Britain was also to send a team.
While some other nations in the Pacific region, such as the Solomon Islands and Kiribati, have also had sluggish vaccine rollouts, the tiny nation of Palau had 99% of its population over 12 vaccinated by mid-October, while Fiji had 96% of eligible people with one dose, the Red Cross said this month.
(Reporting by Lidia Kelly in Melbourne; Editing by William Mallard)
Health
Quebec successfully pushes back against rise in measles cases – CBC.ca
Quebec appears to be winning its battle against the rising tide of measles after 45 cases were confirmed province-wide this year.
“We’ve had no locally transmitted measles cases since March 25, so that’s good news,” said Dr. Paul Le Guerrier, responsible for immunization for Montreal Public Health.
There are 17 patients with measles in Quebec currently, and the most recent case is somebody who was infected while abroad, he said.
But it was no small task to get to this point.
Le Guerrier said once local transmission was detected, news was spread fast among health centres to ensure proper protocols were followed — such as not letting potentially infected people sit in waiting rooms for hours on end.
Then about 90 staffers were put to work, tracking down those who were in contact with positive cases and are not properly vaccinated. They were given post-exposure prophylaxis, which prevents disease, said Le Guerrier.
From there, a vaccination campaign was launched, especially in daycares, schools and neighbourhoods with low inoculation rates. There was an effort to convince parents to get their children vaccinated.
Vaccination in schools boosted
Some schools, mostly in Montreal, had vaccination rates as low as 30 or 40 per cent.
“Vaccination was well accepted and parents responded well,” said Le Guerrier. “Some schools went from very low to as high as 85 to 90 per cent vaccination coverage.”
But it’s not only children who aren’t properly vaccinated. Le Guerrier said people need two doses after age one to be fully inoculated, and he encouraged people to check their status.
There are all kinds of reasons why people aren’t vaccinated, but it’s only about five per cent who are against immunization, he said. So far, some 10,000 people have been vaccinated against measles province-wide during this campaign, Le Guerrier said.
The next step is to continue pushing for further vaccination, but he said, small outbreaks are likely in the future as measles is spreading abroad and travellers are likely to bring it back with them.
Need to improve vaccination rate, expert says
Dr. Donald Vinh, an infectious diseases specialist from the McGill University Health Centre, said it’s not time to rest on our laurels, but this is a good indication that public health is able to take action quickly and that people are willing to listen to health recommendations.
“We are not seeing new cases or at least the new cases are not exceeding the number of cases that we can handle,” said Vinh.
“So these are all reassuring signs, but I don’t think it’s a sign that we need to become complacent.”
Vinh said there are also signs that the public is lagging in vaccine coverage and it’s important to respond to this with improved education and access. Otherwise, microbes capitalize on our weaknesses, he said.
Getting vaccination coverage up to an adequate level is necessary, Vinh said, or more small outbreaks like this will continue to happen.
“And it’s very possible that we may not be able to get one under control if we don’t react quickly enough,” he said.
Health
Pregnant women in the Black Country urged to get whooping cough vaccine – BBC.com


Pregnant women urged to get whooping cough vaccine
Pregnant women in the Black Country are being urged to get vaccinated against whooping cough after a rise in cases.
The bacterial infection of the lungs spreads very easily and can cause serious problems, especially in babies and young children.
The Black Country Integrated Care Board (ICB) is advising pregnant women between 16 and 32 weeks to contact their GP to get the vaccine so their baby has protection from birth.
The UK Health Security Agency warned earlier this year of a steady decline in uptake of the vaccine in pregnant women and children.
Symptoms of the infection, also known as “100-day cough”, are similar to a cold, with a runny nose and sore throat.
Sally Roberts, chief nursing officer for the ICB, which covers Wolverhampton, Dudley, Walsall and Sandwell, said anyone could catch it, but it was more serious for young children and babies.
“Getting vaccinated while you’re pregnant is highly effective in protecting your baby from developing whooping cough in the first few weeks of their life – ideally from 16 weeks up to 32 weeks of pregnancy,” she said.
“If for any reason you miss having the vaccine, you can still have it up until you go into labour.”
Follow BBC West Midlands on Facebook, X and Instagram. Send your story ideas to: newsonline.westmidlands@bbc.co.uk
Health
Measles cases stabilize in Montreal – CityNews Montreal
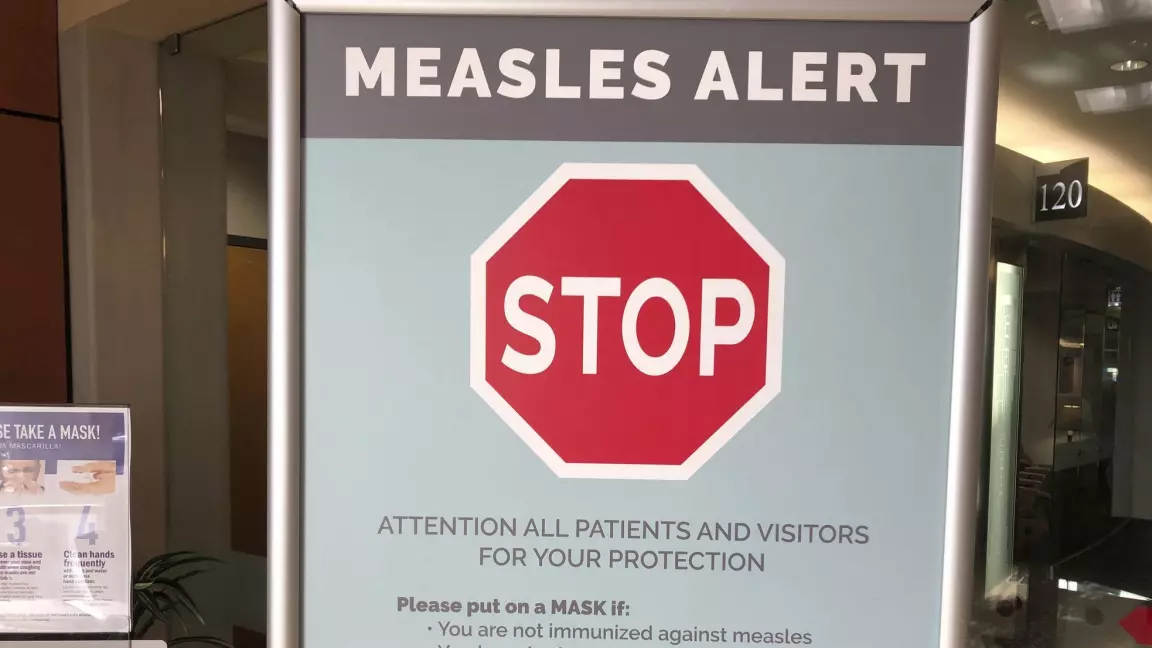
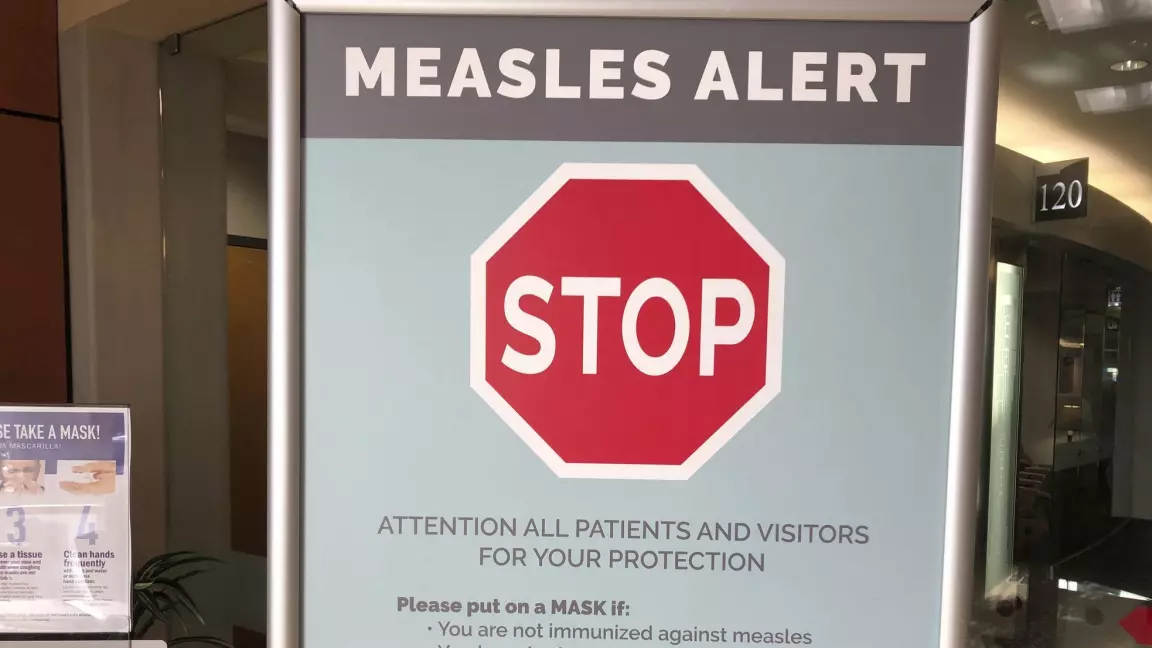
The number of measles cases has stabilized, according to the Montreal Public Health.
Since March 25, there have been no contaminations reported within the community.
“Our teams have identified all contact cases of measles,” said media relations advisor Geneviève Paradis. “It’s a laborious task: each measles case produces hundreds of contacts.”
All community transmission cases since February 2024 have been caused by returning travelers who were either unvaccinated or partially vaccinated.
Currently, there are 18 measles cases in Montreal – with 46 total in Quebec. This according to the April 18 figures from the provincial government.
“With the summer vacations approaching, if you’re travelling, it is essential to check if you are protected against measles,” explained Paradis.
According to Montreal Public Health, a person needs to have received two doses after the age of 12 months to be immunized against the virus.
They’ve launched a vaccination campaign throughout the region, and currently, 11,341 people have been vaccinated against measles in Montreal between March 19 and April 15.
Vaccination is also being provided in schools and at local service points.
“The vaccination operation is under the responsibility of the five CIUSSS of the territory,” concluded Paradis.
-



 Science6 hours ago
Science6 hours agoJeremy Hansen – The Canadian Encyclopedia
-



 Tech24 hours ago
Tech24 hours agoCytiva Showcases Single-Use Mixing System at INTERPHEX 2024 – BioPharm International
-



 Health20 hours ago
Health20 hours agoSupervised consumption sites urgently needed, says study – Sudbury.com
-



 Investment6 hours ago
Investment6 hours agoUK Mulls New Curbs on Outbound Investment Over Security Risks – BNN Bloomberg
-
News19 hours ago
Canada's 2024 budget announces 'halal mortgages'. Here's what to know – National Post
-
News18 hours ago
2024 federal budget's key takeaways: Housing and carbon rebates, students and sin taxes – CBC News
-



 Science19 hours ago
Science19 hours agoGiant, 82-foot lizard fish discovered on UK beach could be largest marine reptile ever found – Livescience.com
-
Art15 hours ago
Canada's art installation at Venice Biennale rooted in research, history, beauty – Hamilton Spectator










