Health
13 times more babies born with syphilis in Canada over 4 years, data shows

|
|
The Current15:57Tackling rising syphilis cases across Canada
There has been a sharp increase in the number of babies born in Canada with syphilis, an infection that one doctor says “can be particularly devastating in pregnancy.”
“It can lead to outcomes such as fetal demise … or stillbirth,” said Dr. Darrell Tan, an infectious disease physician at St. Michael’s Hospital in Toronto, and the Canada Research Chair in HIV Prevention and STI Research.
“And then in a child [born with syphilis] there can be many, many manifestations … it can affect organ systems like the brain, the bones and joints, virtually any organ system in the body,” he told The Current’s guest host Mark Kelley.
Figures from the Public Health Agency of Canada (PHAC) show that there were seven cases of congenital syphilis in 2017, but 96 cases in 2021 — an increase of 1,271 per cent over four years. A similar trend has been observed south of the border.
Thirty newborns in Manitoba have been infected with congenital syphilis through the first eight months of 2020, according to information obtained by the Opposition NDP.
That increase is tied to rates of infection within the general population, which have been increasing steadily for the past decade. Last month, health authorities in B.C. revealed a 27 per cent increase in cases from 2021-22.
Historically, the disease has disproportionately affected men who have sex with men (MSM), but Dr. Troy Grennan said B.C. figures show a shift in 2022.
“For the first time the majority — so more than 50 per cent — of the new cases we’re seeing [in B.C. are] in non-MSM populations,” said Grennan, lead physician at B.C.’s Centre for Disease Control’s sexual health programs.
“One of the key challenges around that is that we’re seeing increasing cases in folks who are capable of getting pregnant,” he said.
Experts say there’s likely multiple factors behind the increase, including reduced condom use — a 2020 survey found that seven in 10 of Canadian respondents don’t use condoms. Some experts also point to the increasing availability of routine testing, and the idea that numbers are up in part because more infections are being detected.
Tan said the spread into new demographics “may simply be a numbers game.”
“When you have cases, case rates that are going up to this degree, you start to see it spread beyond just the core sexual networks that had traditionally been involved,” he said.
If caught early, an infection can be easily treated with antibiotics. But Tan said that structural inequalities, such as racism and the legacy of colonization, can also “impact people’s willingness or perhaps ability to access care at earlier stages — where we can maybe nip things in the bud.”


Diverse symptoms, or none at all
Syphilis can present a diverse range of symptoms, which can complicate catching the infection early, Tan said.
On initial infection, an ulcer can appear at the part of the body that was exposed, he said. But that ulcer might be painless, and perhaps on a body part where it’s hard to see, such as the vagina or rectum.
In other cases, the infection sparks a fever or rash. These symptoms may prompt someone to seek medical attention, but they can also be mistaken for many other illnesses.
“The most confusing and frustrating thing is that it can cause no symptoms at all, and people can contract it without even realizing it,” Tan said.
If left untreated, the infection can have serious implications, including neurological problems, organ damage, loss of vision and even death.


Vaccine work ‘not very far along’
Research into syphilis is complicated by the fact that the “bacterium is very difficult to work with,” said Caroline Cameron, one of the few researchers studying the infection in Canada.
“We really don’t understand how it works, how it infects a person or ways to appropriately combat it, or prevent that infection,” said Cameron, a professor in the department of biochemistry and microbiology at the University of Victoria.
While Cameron said she was drawn to those challenges, they’ve dissuaded many other researchers — but that is slowly changing.
“We are starting to get more philanthropic organizations who are providing funding for research and we’re starting to see more people join the field, which is what is really needed in order to get those innovative research programs going,” she said.
The aim is to produce better medical interventions, perhaps even a vaccine for syphilis, she said. But the difficulties in studying it mean that, globally, the research is “not very far along,” she said.
“Conservative estimates [for a vaccine] are five to 10 years away. But we really need more people to join the field to expand the research population,” she said.
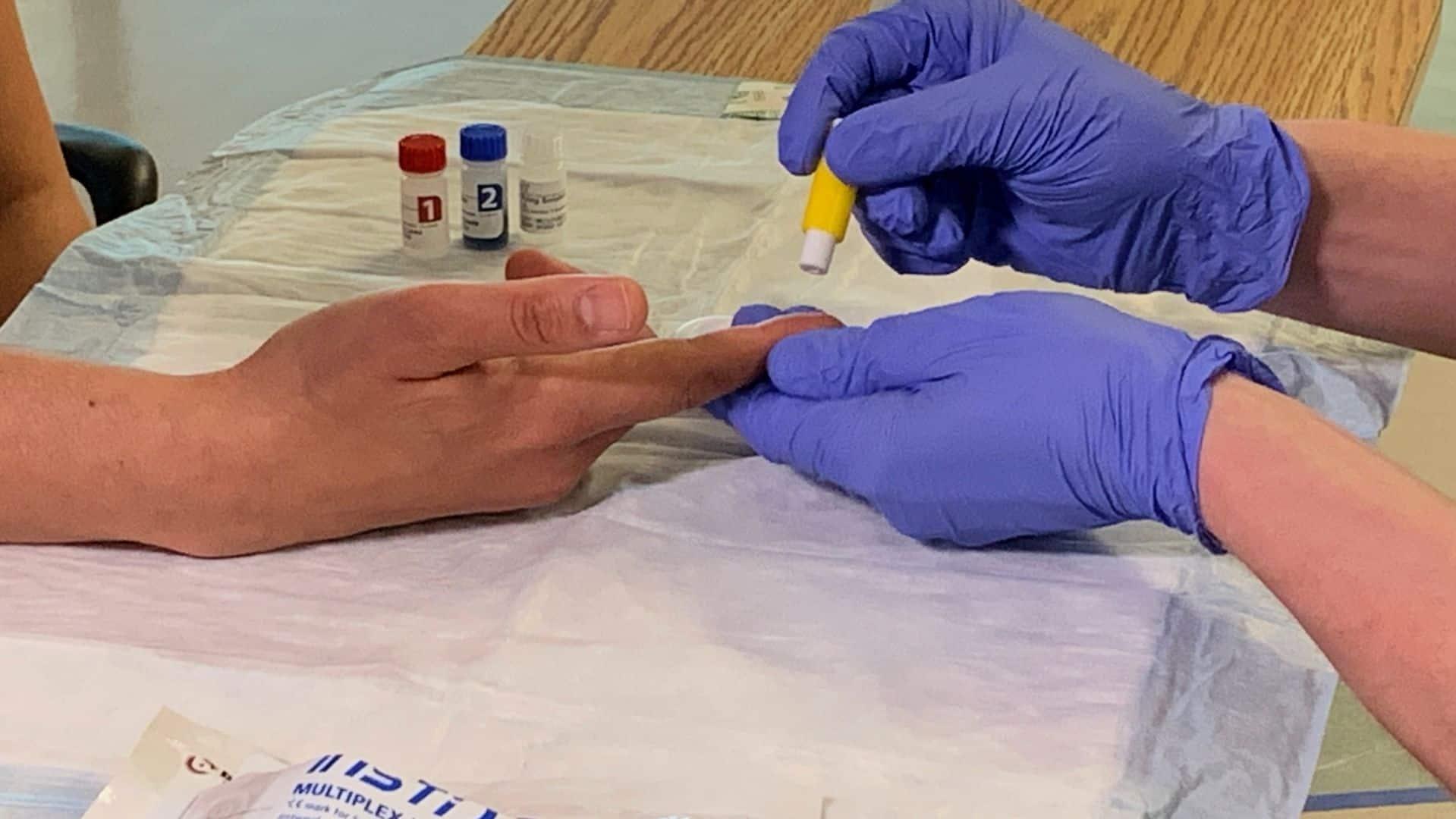
Doctors and outreach workers are hopeful wider use of a new rapid test for syphilis could help slow the spread of the dangerous sexually transmitted infection.
Get tested, get treated
Syphilis can be detected by a simple blood test “that can be ordered by any clinician relatively easily,” but the challenge is often knowing when to request it, Tan said.
He suggested people who are sexually active with multiple partners should seek routine STI testing, as frequently as every three months.
PHAC guidelines stipulate universal screening for syphilis during the first trimester of pregnancy. For those at greater risk of exposure, the guidelines suggest a repeat screening at 28 to 32 weeks, and again at delivery.
However, problems can arise for “folks who unfortunately don’t access pre-natal care,” he said.
“We do have very effective treatments … simply two or more injections of plain old penicillin,” Tan said.
“But if folks are not accessing care earlier in the course of infection … then we can see cases continue to spiral as we’ve seen, and have a hard time getting control of the epidemic.”





Health
Avian influenza spread: WHO gives public health warning as FDA calms food safety concerns – Food Ingredients First


23 April 2024 — The World Health Organization (WHO) has warned that the ongoing spread of avian influenza poses a “significant public health concern” and urged health authorities, especially in the US, to closely monitor infections in cows. However, the US FDA maintains that the virus is not currently a concern to consumer health and downplayed its impact on commercial milk production.
Earlier this month, the largest producer of fresh eggs in the US halted production at a Texas plant after bird flu was detected in its chickens. Cal-Maine Foods said that about 3.6% of its total flock was destroyed after the infection.
However, the virus, also known as H5N1, has now been found in at least 26 dairy herds across eight US states, marking the first time this strain of bird flu has been detected in cattle, according to officials.
At least 21 states have restricted cattle importations from states where the virus is known to have infected dairy cows.
The US Department of Agriculture’s Animal and Plant Health Inspection Service strongly recommends minimizing the movement of cattle, but has not issued federal quarantine orders.
Public health threat
The US Centers for Disease Control and Prevention (CDC) confirmed this month that a dairy worker in Texas, who reportedly had exposure to dairy cattle presumed to have had avian influenza, contracted the virus and is now recovering.
“This infection does not change the H5N1 bird flu human health risk assessment for the US general public, which CDC considers to be low,” the agency said in a press release, while acknowledging that people who come into more frequent contact with possibly infected birds or other mammals have a higher risk.
Meanwhile, WHO’s chief scientist, Dr. Jeremy Farrar, told reporters recently in Geneva, Switzerland, that H5N1 has had an “extremely high” mortality rate among the several hundred people known to have been infected with it to date.


“H5N1 is an influenza infection, predominantly started in poultry and ducks and has spread effectively over the course of the last one or two years to become a global zoonotic — animal — pandemic,” said Farrar.
“The great concern, of course, is that in doing so and infecting ducks and chickens — but now increasingly mammals — the virus now evolves and develops the ability to infect humans.
“And then critically, the ability to go from human-to-human transmission.”
Concerns with cattle
US health officials have stressed that bird flu’s risk to the public is low, and the country’s food supply remains safe and stable.
“At this time, there continues to be no concern that this circumstance poses a risk to consumer health or that it affects the safety of the interstate commercial milk supply,” the FDA said in a statement.
According to officials, farmers are being urged to test cows that show symptoms of infection and separate them from the herd, where they usually recover within two weeks.
US producers are not permitted to sell milk from sick cows, while milk sold across state lines must be pasteurized or heat-treated to kill viruses, including influenza.

“We firmly believe that pasteurization provides a safe milk supply,” Tracey Forfa, director of the FDA’s Center for Veterinary Medicine, told a webinar audience last week.
However, WHO’s Farrar has urged further caution by public health authorities “because it [the virus] may evolve into transmitting in different ways.”
“Do the milking structures of cows create aerosols? Is it the environment which they’re living in? Is it the transport system that is spreading this around the country?” he said.
“This is a huge concern, and I think we have to…make sure that if H5N1 did come across to humans with human-to-human transmission that we were in a position to immediately respond with access equitably to vaccines, therapeutics and diagnostics.”
According to a new European Food Safety Authority report, outbreaks of avian influenza continue to spread in the EU and beyond.
By Joshua Poole
To contact our editorial team please email us at
editorial@cnsmedia.com
If you found this article valuable, you may wish to receive our newsletters.
Subscribe now to receive the latest news directly into your inbox.
Health
York Region urges you to get up to date on vaccinations – NewmarketToday.ca

York Region Public Health is reminding residents to keep up to date on their vaccinations as National Immunization Awareness Week begins.
The regional municipality said it is important to stay up to date on recommended vaccinations to ensure protection from contagious diseases. That includes updated COVID-19 vaccinations for vulnerable populations, recommended as part of a spring vaccination campaign.
“We know vaccines are safe and the best way to stay protected against vaccine-preventable disease,” the region said in a news release.
National Immunization Awareness Week runs from April 22 to 30, with this year’s theme being “Protect your future, get immunized.”
This spring, the region is still doing COVID-19 vaccinations. While walk-ins are no longer available as of April 2, you can book an appointment to visit a York Region clinic.
The spring COVID-19 vaccination campaign is aimed at more vulnerable groups who have received a COVID-19 vaccine before. Those include seniors, those living in seniors living facilities like long-term care homes, immunocompromised individuals and those in Indigenous households who are 55 or older. Public health also recommends the COVID-19 vaccine for those who have not yet received one.
York Region Public Health is also reminding residents of the need for other vaccines.
Measles cases have sprung up in Ontario and York Region recently. The region is recommending that people ensure they previously raised two valid doses of the measles vaccine. The region will also start providing measles vaccines April 29 for those overdue and for who do not have access to the vaccine through a health-care provider.
School-aged vaccinations are also available for free for children in junior kindergarten to Grade 12.
You can access immunization information at york.ca/immunziations or by contacting Access York at 1-877-464-9675.
“Vaccination helps protect everyone in our families, communities and schools,” the region said. “ By continuing to stay up to date on your immunizations, you help protect infants who are too young to be vaccinated and those not able to get vaccinated due to medical conditions.”
Health
Bird flu raises concern of WHO – ecns


The World Health Organization (WHO) said the rising number of bird flu cases has raised “great concern” because it had an “extremely high” mortality rate among those who had been infected around the world.
The WHO’s data show that from 2003 through March 2024, a total of 889 worldwide human cases of H5N1 infection had been recorded in 23 countries, resulting in 463 deaths and a 52 percent mortality rate. The majority of deaths occurred in Southeast Asian countries and Egypt.
The most recent death was in Vietnam in late March, when a 21-year-old male without underlying conditions died of the infection after bird hunting. So far, cases in Europe and the United States have been mild.
Jeremy Farrar, chief scientist at the WHO, said recently that H5N1, predominantly started in poultry and ducks, “has spread effectively over the course of the last one or two years to become a global zoonotic — animal — pandemic”.
He said that the great concern is that the virus is increasingly infecting mammals and then develops the ability to infect humans. It would become critical if the virus develops the ability to “go from human-to-human transmission”, Farrar said.
In the past month, health officials have detected H5N1 in cows and goats from 29 dairy herds across eight states in the US, saying it is an alarming development because those livestock weren’t considered susceptible to H5N1.
The development worries health experts and officials because humans regularly come into contact with livestock on farms. In the US, there are only two recorded cases of human infection — one in 2022 and one in April this year in Texas. Both infected individuals worked in close proximity to livestock, but their symptoms were mild.
Wenqing Zhang, head of the WHO’s global influenza program, told the Daily Mail that “bird-to-cow, cow-to-cow and cow-to-bird transmission have also been registered during these current outbreaks, which suggest that the virus may have found other routes of transition than we previously understood”.
Zhang said that multiple herds of cow infections in the US states meant “a further step of the virus spillover to mammals”.
The virus has been found in raw milk, but the Texas Health Services department has said the cattle infections don’t present a concern for the commercial milk supply, as dairies are required to destroy milk from sick cows. In addition, pasteurization also kills the virus.
Darin Detwiler, a former food safety adviser to the Food and Drug Administration and the US Agriculture Department, said that Americans should avoid rare meat and runny eggs while the outbreak in cattle is going on to avoid the possibility of infection from those foods.
Nevertheless, both the WHO and the Centers for Disease Control and Prevention (CDC) said that the risk the virus poses to the public is still low. Currently no human-to-human infection has been detected.
On the potential HN51 public health risk, Farrar cautioned that vaccine development was not “where we need to be”.
According to a report by Barron’s, under the current plan by the US Health and Human Services Department, if there is an H5N1 pandemic, the government would be able to supply a few hundred thousand doses within weeks, then 135 million within about four months.
People would need two doses of the shot to be fully protected. That means the US government would be able to inoculate about 68 million people — 20 percent — of 330 million in case of an outbreak.
The situation is being closely watched by scientists and health officials. Some experts said that a high mortality rate might not necessarily hold true in the event the virus became contagious among people.
“We may not see the level of mortality that we’re really concerned about,” Seema Lakdawala, a virologist at Emory University, told The New York Times. “Preexisting immunity to seasonal flu strains will provide some protection from severe disease.”
Agencies contributed to this story.
-
Business20 hours ago
Honda to build electric vehicles and battery plant in Ontario, sources say – Global News
-



 Science21 hours ago
Science21 hours agoWill We Know if TRAPPIST-1e has Life? – Universe Today
-



 Health18 hours ago
Health18 hours agoSee how chicken farmers are trying to stop the spread of bird flu – Fox 46 Charlotte
-



 Health21 hours ago
Health21 hours agoSimcoe-Muskoka health unit urges residents to get immunized
-



 Investment19 hours ago
Investment19 hours agoOwn a cottage or investment property? Here's how to navigate the new capital gains tax changes – The Globe and Mail
-



 Science23 hours ago
Science23 hours agoLyrid meteor shower 2024: How to see a stunning fireball tonight – BBC Science Focus
-
News16 hours ago
Freeland defends budget measures, as premiers push back on federal involvement – CBC News
-



 Politics24 hours ago
Politics24 hours agoThe Politics of Pessimism