Health
Take 2 steps and call me in the morning: Exercise as a prescription for depression – CBC.ca

Judy Mulloy’s voice breaks and her eyes well up with tears as she describes how a simple walk in the park and chair yoga has helped her through the pandemic.
“Oh, it’s a happy cry, I assure you,” she said. “My life has changed around. It’s no longer a thing of sadness.”
Mulloy, 56, first turned to physical activity years ago to manage her depression. She says staying active in her hometown of Nelson, B.C., hasn’t eliminated her need for a daily antidepressant.
“But the thing that can boost my mood is to go for a walk. Go for a swim. Do some exercise,” she said.
That tonic began to dry up when the first COVID-19 lockdown hit in 2020 and gyms and recreation centres were shuttered. Mulloy responded to a social media post looking for volunteers for a study that replaced facilities and classes with a commercially available app.
“I’ve not looked back. It’s been amazing,” she said.
Anxiety, depression increased in pandemic
The study was conceived by Eli Puterman, an assistant professor at the School of Kinesiology at the University of British Columbia in Vancouver.
Puterman says he was moved by surveys such as the poll done for Mental Health Research Canada in early 2020, which suggested anxiety levels had quadrupled and depression levels doubled during the pandemic.
“People were suffering. So, we wanted to see whether we can support people,” Puterman said.
His research team recruited over 300 people, gave them a free subscription to an exercise app and divided them into four randomized groups that either did yoga, high-intensity interval training, a combination of the two, or were relegated to a wait list.
Each week, participants completed a standard questionnaire that’s used in the diagnosis and treatment of depression. Using a scale of zero to three, people reported how often they experienced symptoms such as sleeplessness or feeling lonely.
The results were reported in the British Journal of Sports Medicine last fall.
“Everyone dropped in their depression levels,” Puterman said.
Judy Mulloy gets emotional explaining how exercise has helped her regain hope and change aspects of her life that were contributing to her depression. 1:40
While none of the participants were screened to determine whether they had been diagnosed as clinically depressed, of those who were active in the study, the ones who reported the most severe symptoms at the start showed the biggest improvement, Puterman said.
“I am surprised by how drastic of an effect it was,” he said.
Past studies show similar results
Puterman’s results are only the latest to link physical activity and mood. “There’s been enough studies,” said Vancouver psychiatrist Dr. Ron Remick.
Remick thinks physical activity can be as effective as some more common treatments for depression, such as psychotherapy or antidepressants. But while it’s true that research going back decades demonstrates the ability of exercise to measurably reduce symptoms of depression and stave off relapse, on its own, it may not be enough to treat severe depression, a complex disease that can have multiple causes.


Remick’s advocacy for movement as medicine comes from his own experience. Seven years ago, as medical director of the Mood Disorders Association of British Columbia he pioneered a weekly program of low-impact movement for his patients called Jump Step.
It involved outdoor walks, floor exercises and cardio routines combined with a group medical visit.
When the pandemic struck, the program went virtual. Participants were given the only equipment they’d need: a yoga mat and an exercise band. Jump Step now runs for eight weeks, four times a year. Its results have drawn attention from the B.C. government, which was interested in potentially implementing it provincewide.
“Much like our earlier research, it has continued to show that a significant number of people who do a program like this have significant improvement in their depressive symptoms,” Remick said.
‘A break from all of that chatter’
Michael Sarvari leads the weekly classes. Sarvari draws on his own experience as someone who wrestled with severe depression for most of his life until one day, he says, he crawled out of bed and convinced himself to do a pushup. The next day he tried two, and so on.
“When you’re depressed, your mind is so busy with negative thoughts and chatter,” Sarvari said.
“When you kind of take yourself out of your mind and into your body doing physical things, you get a break from all of that chatter. It kind of creates that calm within yourself.”
Sarvari says it’s hard to overstate the benefits of basic, regular physical activity
“I could be homeless because I wasn’t able to support myself. I wasn’t able to work,” he said. “I would be in a very dark place and possibly not alive because I was suicidal for many years.”
Ron Remick, medical director for the Mood Disorders Association of British Columbia, explains how a small amount of moderate exercise can help tackle depression and reduce your risk of some diseases. 0:50
Researchers are hoping to ease that kind of personal suffering while acknowledging there’s a payoff for the wider public if they’re successful. A decade ago, the World Economic Forum and the Harvard School of Public Health forecast the global cost of mental health conditions by 2030 to be over $7 trillion a year.
“Changes occur slowly in medicine even when the evidence is there for a long long time,” said Remick.
Unlike a pill, prescribing exercise has to be tailored to a patient’s abilities by doctors who know how to motivate people.
Puterman says while there is ample evidence to support his broader findings, some research gaps remain. Most of the participants in his study were white and maintained their jobs during the pandemic. He plans to focus a future study on more diverse and vulnerable communities.
Health
Whooping cough cases up slightly in N.L., as officials warn about risks to infants – CBC.ca

Newfoundland and Labrador’s top doctor is warning people to stay up to date on whooping cough vaccinations after a small increase in cases this year.
The province usually sees three to four cases of the disease annually. Up to 10 cases have been reported already since January, however, prompting the province’s chief medical officer to raise the issue publicly.
The increase “generally means there’s a little bit more circulating in the community than what’s presenting for care and testing,” Dr. Janice Fitzgerald said Tuesday.
While officials aren’t overly concerned about a future spike in cases, Fitzgerald said, higher infection rates place infants in particular at risk.
Children under the age of one aren’t yet old enough for the whooping cough vaccine and don’t have immunity to the disease, Fitzgerald said. Infections in small children can be more severe and lead to pneumonia, neurological issues and hospitalization.
Fitzgerald said parents, grandparents and caregivers should check to ensure their vaccinations are up to date.
Whooping cough, also known as pertussis, causes a persistent nagging cough that’s sometimes severe enough to cause vomiting. Vaccines for the disease are offered in early childhood, during high school and in adulthood. Booster shots should be given 10 years after the high school dose, Fitzgerald said.
“Immunity can wane over time,” she said. “Pertussis does circulate on a regular basis in our community.”
The small increase in cases isn’t yet ringing alarm bells for undervaccination within the general population, she added, noting the province still has a vaccination rate over 90 per cent.
Download our free CBC News app to sign up for push alerts for CBC Newfoundland and Labrador. Click here to visit our landing page.
Health
Supervised consumption sites urgently needed, says study – Sudbury.com

A study in the Canadian Medical Association Journal (CMAJ) said the opioid drug crisis has reached such a critical level that a public safety response is urgently required and that includes the need for expanded supervised consumption sites.
The report was published by the medical journal Monday and was authored by Shaleesa Ledlie, David N. Juurlink, Mina Tadrous, Muhammad Mamdani, J. Michael Paterson and Tara Gomes; physicians and scientists associated with the University of Toronto, Sunnybrook Research Institute and the Li Ka Shing Knowledge Institute at St. Michael’s Hospital.
“The drug toxicity crisis continues to accelerate across Canada, with rapid increases in opioid-related harms following the onset of the COVID-19 pandemic,” the authors wrote. “We sought to describe trends in the burden of opioid-related deaths across Canada throughout the pandemic, comparing these trends by province or territory, age and sex.”
The study determined that across Canada, the burden of premature opioid-related deaths doubled between 2019 and 2021, representing more than one-quarter of deaths among younger adults. The disproportionate loss of life in this demographic group highlights the critical need for targeted prevention efforts, said the study.
The researchers found that the death rate increased significantly as fentanyl was introduced to the mix of street drugs that individuals were using, in some cases, unknowingly.
The authors said this demonstrates the need for consumption sites, not only as overwatch as people with addictions consume their drugs, but also to make an effort to identify the substances and inform those people beforehand.
“The increased detection of fentanyl in opioid-related deaths in Canada highlights the need for expansion of harm-reduction programs, including improved access to drug-checking services, supervised consumption sites, and treatment for substance use disorders,” the authors wrote.
The study said a more intense public safety response is needed.
“Given the rapidly evolving nature of the drug toxicity crisis, a public safety response is urgently required and may include continued funding of safer opioid supply programs that were expanded beginning in March 2020, improved flexibility in take-home doses of opioid agonist treatment, and enhanced training for health care workers, harm reduction workers, and people who use drugs on appropriate responses to opioid toxicities involving polysubstance use.
In conclusion, the authors wrote that during the height of the COVID pandemic in 2020 and 2021, the burden of premature death from accidental opioid toxicities in Canada dramatically increased, especially in Alberta, Saskatchewan, and Manitoba.
“In 2021, more than 70 per cent of opioid-related deaths occurred among males and about 30 per cent occurred among people aged 30–39 years, representing one in every four deaths in this age group. The disproportionate rates of opioid-related deaths observed in these demographic groups highlight the critical need for the expansion of targeted harm reduction–based policies and programs across Canada,” said the study.
The full text of the report can be found online here.
Health
Business Plan Approved for Cancer Centre at NRGH – My Cowichan Valley Now


A business plan for a new BC Cancer Centre at Nanaimo Regional General Hospital has been approved by the province.
Health Minister Adrian Dix says the state-of-the-art cancer facility will benefit patients in Nanaimo and the surrounding region through the latest medical technology.
The facility will have 12 exam rooms, four consultation rooms and space for medical physicists and radiation therapists, medical imaging and radiation treatment of cancer patients.
The procurement process is underway, and construction is expected to begin in 2025 and be complete in 2028.
Upgrades to NRGH have also been approved, such as a new single-storey addition to the ambulatory care building and expanded pharmacy.
Dix says Nanaimo’s population is growing rapidly and aging, and stronger health services in the region, so people get the health care they need closer to home.
-
Business21 hours ago
Rupture on TC Energy's NGTL gas pipeline sparks wildfire in Alberta – The Globe and Mail
-
News22 hours ago
Loblaws Canada groceries: Shoppers slam store for green onions with roots chopped off — 'I wouldn't buy those' – Yahoo News Canada
-
Investment21 hours ago
Saudi Arabia Highlights Investment Initiatives in Tourism at International Hospitality Investment Forum
-
Art21 hours ago
Squatters at Gordon Ramsay's Pub Have 'Left the Building' After Turning It Into an Art Café – PEOPLE
-



 Tech14 hours ago
Tech14 hours agoCytiva Showcases Single-Use Mixing System at INTERPHEX 2024 – BioPharm International
-



 Politics21 hours ago
Politics21 hours agoThe Earthquake Shaking BC Politics
-


 Sports24 hours ago
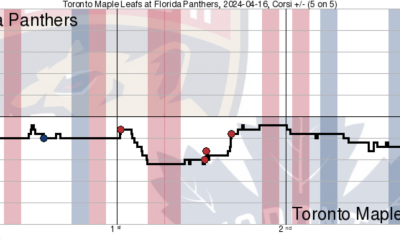
Sports24 hours agoGame in 10: Maple Leafs squander multi-goal lead to Florida, draw the Boston Bruins in the first round – Maple Leafs Hot Stove
-



 Investment20 hours ago
Investment20 hours agoBill Morneau slams Freeland’s budget as a threat to investment, economic growth






