Health
The case for improving the detection and treatment of obstructive sleep apnea following stroke

|
|
KEY POINTS
-
Obstructive sleep apnea (OSA) is prevalent and harmful after stroke.
-
Investigation of sleep disorders, particularly OSA, should be strongly considered for patients who have had a stroke, with the goal of improving nonvascular outcomes.
-
Obstructive sleep apnea should be treated like a vascular risk factor.
-
Future trials will assess whether treatment for OSA initiated early after stroke reduces stroke recurrence.
Stroke is a leading cause of death and disability for people in Canada. Beyond the initial brain injury, the sequelae of stroke may also include several comorbidities, with sleep disorders being among the most important. Obstructive sleep apnea (OSA) and sleep–wake disturbances are highly prevalent among patients who have had a stroke; they may be both a risk factor for and a consequence of stroke, and can substantially affect stroke recovery and functional outcomes.1 Moreover, post-stroke fatigue is a top research priority for patients who have had a stroke.2
In related research, Jeffers and colleagues3 used cross-sectional data from the Canadian Community Health Survey to study relative rates of 4 self-reported sleep disturbances, namely having trouble staying awake, either short (< 5 h) or long (> 9 h) nightly sleep duration, having trouble going to or staying asleep, and having unrefreshing sleep. Almost two-thirds of respondents who reported a history of stroke also reported sleep difficulties; those with a history of stroke also reported each form of sleep disturbance significantly more frequently than those without a history a stroke.
Although the authors of the related research did not specifically examine OSA, many of the sleep concerns among those who reported a history of stroke were likely driven by OSA, the most common post-stroke sleep disorder, which has been reported to occur in as many as 72% of patients who have had a stroke or transient ischemic attack (TIA), depending on OSA severity.4 Patients with pre-existing OSA have poorer functional outcomes and spend more time in rehabilitation after a stroke.5 Randomized controlled trials have shown that treatment of post-stroke OSA using continuous positive airway pressure (CPAP) improves neurologic recovery and quality of life, and reduces daytime sleepiness and depressive symptoms.6,7
Given that OSA is a well-established risk factor for stroke, with a greater adjusted relative risk for stroke similar to or higher than traditional modifiable vascular risk factors that are commonly managed after stroke,8 it would make sense that OSA be routinely screened for and treated after stroke. However, a 2019 study suggested otherwise.9
Lack of screening for OSA after stroke may be explained by several barriers. Obstructive sleep apnea often presents atypically after stroke, and many patients with OSA who have had a stroke do not have the typical clinical features of OSA, such as obesity and daytime sleepiness.10 Many clinicians may be unaware of the importance of managing OSA and any associated symptoms after stroke. Moreover, testing for sleep disorders requires a multidisciplinary approach, and stroke rehabilitation centres may not have the necessary expertise to conduct sleep testing. Furthermore, the current gold standard for diagnosing OSA, in-laboratory sleep testing or polysomnography, is inconvenient for patients who are vulnerable and those with disabilities, and access to such testing in some Canadian centres may be limited. In a randomized controlled trial that assigned 250 consecutively recruited patients with a history of stroke or TIA to either ambulatory or in-laboratory sleep testing, rates of OSA diagnosis and treatment, as well as functional outcomes and daytime sleepiness, were significantly improved in the ambulatory testing arm.11 These results suggest that removing the barriers associated with in-laboratory sleep testing (through the use of ambulatory testing for OSA) may enhance outcomes among patients who have had a stroke or TIA.
Finally, screening for and management of OSA after stroke is underemphasized in stroke guidelines. For example, the 2014 and 2018 guidelines from the American Heart Association and the American Stroke Association for the secondary prevention of stroke stated that evaluation for OSA “may be considered” for patients with stroke or TIA.12 The most recent version of the Canadian Stroke Best Practice Recommendations removed recommendations on management of sleep apnea,13 although earlier versions did comment on OSA.
Fundamental to the question of whether clinicians should screen for and manage OSA after TIA or stroke is whether treatment of OSA after stroke or TIA reduces incident vascular events or mortality. Although studies assessing the impact of CPAP on nonvascular outcomes among patients with post-stroke OSA have shown positive outcomes, trials evaluating whether CPAP can reduce the risk of incident stroke or death have been largely negative.6 The largest of these trials, the Sleep Apnea Cardiovascular Endpoints (SAVE) trial,7 randomized 2717 patients with coronary or cerebrovascular disease (including 1432 with ischemic stroke or intracerebral hemorrhage) to receive CPAP or usual care. Although the overall findings showed no significant reduction in risk of vascular events or death, a preplanned post hoc subgroup analysis showed that patients who had good adherence to CPAP had a significantly lower risk of cerebrovascular events than those in the usual care group. This was consistent with the findings of earlier, smaller trials that also showed that significant reductions in incident vascular events occurred in subgroups with good CPAP adherence. 14,15 Since randomization was not respected in these subgroup analyses, the findings should be interpreted with caution.
It is important to note that the evidence for various interventions in stroke care has varied over time. Evidence related to OSA is rapidly evolving, and future trials that look at outcomes related to OSA after stroke will need to reconsider how OSA is defined and consider selecting patients on the basis of distinct clinical phenotypes. 16,17 For patients who cannot tolerate CPAP, many new treatment alternatives — including use of pharmacological agents, hypoglossal nerve stimulation, oropharyngeal exercises and dental appliances — have been shown to be effective outside of the stroke population; these need to be evaluated for patients who have had a stroke or TIA.18 Reflecting what has been seen in other studies evaluating secondary stroke prevention strategies (e.g., antiplatelet trials), interventions for OSA will need to be administered in the hours and days after stroke and not in a delayed fashion, as was done in the SAVE trial. Furthermore, in future trials, sample sizes and follow-up periods need to be carefully calculated to assure adequate power and outcome assessment.6
Investigation of sleep disorders, particularly OSA, should be strongly considered for patients who have had a stroke, with the goal of improving nonvascular outcomes, such as daytime sleepiness, mood and functional outcomes. A good argument can be made for treating OSA like any other vascular risk factor.8 Future trials, such as the ongoing Sleep for Stroke Management and Recovery Trial (Sleep SMART Trial; NCT03812653), will assess whether CPAP treatment for OSA that is started early after stroke reduces stroke recurrence.
Footnotes
-
Competing interests: Mark Boulos reports funding from the Canadian Institutes of Health Research, Canadian Partnership for Stroke Recovery, Alternative Funding Plan from the Academic Health Sciences Centres of Ontario, Ontario Genomics and McLaughlin Centre for Molecular Medicine. He also reports consulting fees and honoraria from Jazz Pharmaceuticals, Paladin Labs, Eisai and the OntarioMD Peer Leader Program; travel support from McGill University; and receipt of sleep equipment or research support from Braebon Medical Corporation, The Mahaffy Family Research Fund and Green Mountain.
-
This article was solicited and has not been peer reviewed.
This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY-NC-ND 4.0) licence, which permits use, distribution and reproduction in any medium, provided that the original publication is properly cited, the use is noncommercial (i.e., research or educational use), and no modifications or adaptations are made. See: https://creativecommons.org/licenses/by-nc-nd/4.0/





Health
Toronto reports 2 more measles cases. Use our tool to check the spread in Canada – Toronto Star


/* OOVVUU Targeting */
const path = ‘/news/canada’;
const siteName = ‘thestar.com’;
let domain = ‘thestar.com’;
if (siteName === ‘thestar.com’)
domain = ‘thestar.com’;
else if (siteName === ‘niagarafallsreview.ca’)
domain = ‘niagara_falls_review’;
else if (siteName === ‘stcatharinesstandard.ca’)
domain = ‘st_catharines_standard’;
else if (siteName === ‘thepeterboroughexaminer.com’)
domain = ‘the_peterborough_examiner’;
else if (siteName === ‘therecord.com’)
domain = ‘the_record’;
else if (siteName === ‘thespec.com’)
domain = ‘the_spec’;
else if (siteName === ‘wellandtribune.ca’)
domain = ‘welland_tribune’;
else if (siteName === ‘bramptonguardian.com’)
domain = ‘brampton_guardian’;
else if (siteName === ‘caledonenterprise.com’)
domain = ‘caledon_enterprise’;
else if (siteName === ‘cambridgetimes.ca’)
domain = ‘cambridge_times’;
else if (siteName === ‘durhamregion.com’)
domain = ‘durham_region’;
else if (siteName === ‘guelphmercury.com’)
domain = ‘guelph_mercury’;
else if (siteName === ‘insidehalton.com’)
domain = ‘inside_halton’;
else if (siteName === ‘insideottawavalley.com’)
domain = ‘inside_ottawa_valley’;
else if (siteName === ‘mississauga.com’)
domain = ‘mississauga’;
else if (siteName === ‘muskokaregion.com’)
domain = ‘muskoka_region’;
else if (siteName === ‘newhamburgindependent.ca’)
domain = ‘new_hamburg_independent’;
else if (siteName === ‘niagarathisweek.com’)
domain = ‘niagara_this_week’;
else if (siteName === ‘northbaynipissing.com’)
domain = ‘north_bay_nipissing’;
else if (siteName === ‘northumberlandnews.com’)
domain = ‘northumberland_news’;
else if (siteName === ‘orangeville.com’)
domain = ‘orangeville’;
else if (siteName === ‘ourwindsor.ca’)
domain = ‘our_windsor’;
else if (siteName === ‘parrysound.com’)
domain = ‘parrysound’;
else if (siteName === ‘simcoe.com’)
domain = ‘simcoe’;
else if (siteName === ‘theifp.ca’)
domain = ‘the_ifp’;
else if (siteName === ‘waterloochronicle.ca’)
domain = ‘waterloo_chronicle’;
else if (siteName === ‘yorkregion.com’)
domain = ‘york_region’;
let sectionTag = ”;
try
if (domain === ‘thestar.com’ && path.indexOf(‘wires/’) = 0)
sectionTag = ‘/business’;
else if (path.indexOf(‘/autos’) >= 0)
sectionTag = ‘/autos’;
else if (path.indexOf(‘/entertainment’) >= 0)
sectionTag = ‘/entertainment’;
else if (path.indexOf(‘/life’) >= 0)
sectionTag = ‘/life’;
else if (path.indexOf(‘/news’) >= 0)
sectionTag = ‘/news’;
else if (path.indexOf(‘/politics’) >= 0)
sectionTag = ‘/politics’;
else if (path.indexOf(‘/sports’) >= 0)
sectionTag = ‘/sports’;
else if (path.indexOf(‘/opinion’) >= 0)
sectionTag = ‘/opinion’;
} catch (ex)
const descriptionUrl = ‘window.location.href’;
const vid = ‘mediainfo.reference_id’;
const cmsId = ‘2665777’;
let url = `https://pubads.g.doubleclick.net/gampad/ads?iu=/58580620/$domain/video/oovvuu$sectionTag&description_url=$descriptionUrl&vid=$vid&cmsid=$cmsId&tfcd=0&npa=0&sz=640×480&ad_rule=0&gdfp_req=1&output=vast&unviewed_position_start=1&env=vp&impl=s&correlator=`;
url = url.split(‘ ‘).join(”);
window.oovvuuReplacementAdServerURL = url;
Canada has seen a concerning rise in measles cases in the first months of 2024.
By the third week of March, the country had already recorded more than three times the number of cases as all of last year. Canada had just 12 cases of measles in 2023, up from three in 2022.
function buildUserSwitchAccountsForm()
var form = document.getElementById(‘user-local-logout-form-switch-accounts’);
if (form) return;
// build form with javascript since having a form element here breaks the payment modal.
var switchForm = document.createElement(‘form’);
switchForm.setAttribute(‘id’,’user-local-logout-form-switch-accounts’);
switchForm.setAttribute(‘method’,’post’);
switchForm.setAttribute(‘action’,’https://www.thestar.com/tncms/auth/logout/?return=https://www.thestar.com/users/login/?referer_url=https%3A%2F%2Fwww.thestar.com%2Fnews%2Fcanada%2Ftoronto-reports-2-more-measles-cases-use-our-tool-to-check-the-spread-in-canada%2Farticle_20aa7df4-e88f-11ee-8fad-8f8368d7ff53.html’);
switchForm.setAttribute(‘style’,’display:none;’);
var refUrl = document.createElement(‘input’); //input element, text
refUrl.setAttribute(‘type’,’hidden’);
refUrl.setAttribute(‘name’,’referer_url’);
refUrl.setAttribute(‘value’,’https://www.thestar.com/news/canada/toronto-reports-2-more-measles-cases-use-our-tool-to-check-the-spread-in-canada/article_20aa7df4-e88f-11ee-8fad-8f8368d7ff53.html’);
var submit = document.createElement(‘input’);
submit.setAttribute(‘type’,’submit’);
submit.setAttribute(‘name’,’logout’);
submit.setAttribute(‘value’,’Logout’);
switchForm.appendChild(refUrl);
switchForm.appendChild(submit);
document.getElementsByTagName(‘body’)[0].appendChild(switchForm);
function handleUserSwitchAccounts()
window.sessionStorage.removeItem(‘bd-viafoura-oidc’); // clear viafoura JWT token
// logout user before sending them to login page via return url
document.getElementById(‘user-local-logout-form-switch-accounts’).submit();
return false;
buildUserSwitchAccountsForm();
#ont-map-iframepadding:0;width:100%;border:0;overflow:hidden;
#ontario-cases-iframepadding:0;width:100%;border:0;overflow:hidden;
#province-table-iframepadding:0;width:100%;border:0;overflow:hidden;
console.log(‘=====> bRemoveLastParagraph: ‘,0);
Health
Cancer Awareness Month – Métis Nation of Alberta


Cancer Awareness Month
Posted on: Apr 18, 2024
April is Cancer Awareness Month
As we recognize Cancer Awareness Month, we stand together to raise awareness, support those affected, advocate for prevention, early detection, and continued research towards a cure. Cancer is the leading cause of death for Métis women and the second leading cause of death for Métis men. The Otipemisiwak Métis Government of the Métis Nation Within Alberta is working hard to ensure that available supports for Métis Citizens battling cancer are culturally appropriate, comprehensive, and accessible by Métis Albertans at all stages of their cancer journey.
Receiving a cancer diagnosis, whether for yourself or a loved one, can feel overwhelming, leaving you unsure of where to turn for support. In June, our government will be launching the Cancer Supports and Navigation Program which will further support Métis Albertans and their families experiencing cancer by connecting them to OMG-specific cancer resources, external resources, and providing navigation support through the health care system. This program will also include Métis-specific peer support groups for those affected by cancer.
With funding from the Canadian Partnership Against Cancer (CPAC) we have also developed the Métis Cancer Care Course to ensure that Métis Albertans have access to culturally safe and appropriate cancer services. This course is available to cancer care professionals across the country and provides an overview of who Métis people are, our culture, our approaches to health and wellbeing, our experiences with cancer care, and our cancer journey.
Together, we can make a difference in the fight against cancer and ensure equitable access to culturally safe and appropriate care for all Métis Albertans. Please click on the links below to learn more about the supports available for Métis Albertans, including our Compassionate Care: Cancer Transportation program.
I wish you all good health and happiness!
Bobbi Paul-Alook
Secretary of Health & Seniors
Health
Type 2 diabetes is not one-size-fits-all: Subtypes affect complications and treatment options – The Conversation


You may have heard of Ozempic, the “miracle drug” for weight loss, but did you know that it was actually designed as a new treatment to manage diabetes? In Canada, diabetes affects approximately 10 per cent of the general population. Of those cases, 90 per cent have Type 2 diabetes.
This metabolic disorder is characterized by persistent high blood sugar levels, which can be accompanied by secondary health challenges, including a higher risk of stroke and kidney disease.
Locks and keys
In Type 2 diabetes, the body struggles to maintain blood sugar levels in an acceptable range. Every cell in the body needs sugar as an energy source, but too much sugar can be toxic to cells. This equilibrium needs to be tightly controlled and is regulated by a lock and key system.
In the body’s attempt to manage blood sugar levels and ensure that cells receive the right amount of energy, the pancreatic hormone, insulin, functions like a key. Cells cover themselves with locks that respond perfectly to insulin keys to facilitate the entry of sugar into cells.
Unfortunately, this lock and key system doesn’t always perform as expected. The body can encounter difficulties producing an adequate number of insulin keys, and/or the locks can become stubborn and unresponsive to insulin.
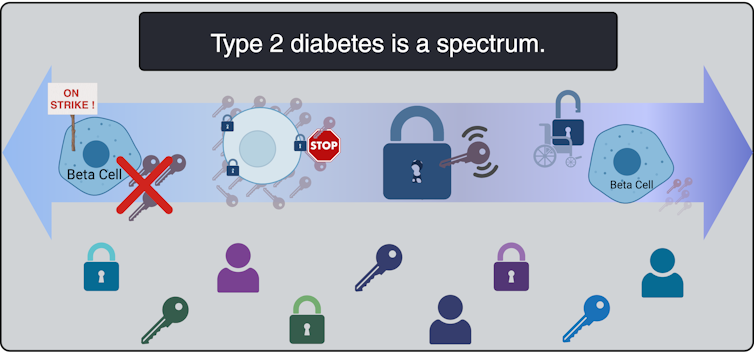
All forms of diabetes share the challenge of high blood sugar levels; however, diabetes is not a singular condition; it exists as a spectrum. Although diabetes is broadly categorized into two main types, Type 1 and Type 2, each presents a diversity of subtypes, especially Type 2 diabetes.
These subtypes carry their own characteristics and risks, and do not respond uniformly to the same treatments.
To better serve people living with Type 2 diabetes, and to move away from a “one size fits all” approach, it is beneficial to understand which subtype of Type 2 diabetes a person lives with. When someone needs a blood transfusion, the medical team needs to know the patient’s blood type. It should be the same for diabetes so a tailored and effective game plan can be implemented.
This article explores four unique subtypes of Type 2 diabetes, shedding light on their causes, complications and some of their specific treatment avenues.
Severe insulin-deficient diabetes: We’re missing keys!
(Lili Grieco-St-Pierre, Jennifer Bruin/Created with BioRender.com)
Insulin is produced by beta cells, which are found in the pancreas. In the severe insulin-deficient diabetes (SIDD) subtype, the key factories — the beta cells — are on strike. Ultimately, there are fewer keys in the body to unlock the cells and allow entry of sugar from the blood.
SIDD primarily affects younger, leaner individuals, and unfortunately, increases the risk of eye disease and blindness, among other complications. Why the beta cells go on strike remains largely unknown, but since there is an insulin deficiency, treatment often involves insulin injections.
Severe insulin-resistant diabetes: But it’s always locked!
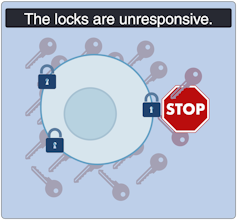
(Lili Grieco-St-Pierre, Jennifer Bruin/Created with BioRender.com)
In the severe insulin-resistant diabetes (SIRD) subtype, the locks are overstimulated and start ignoring the keys. As a result, the beta cells produce even more keys to compensate. This can be measured as high levels of insulin in the blood, also known as hyperinsulinemia.
This resistance to insulin is particularly prominent in individuals with higher body weight. Patients with SIRD have an increased risk of complications such as fatty liver disease. There are many treatment avenues for these patients but no consensus about the optimal approach; patients often require high doses of insulin.
Mild obesity-related diabetes: The locks are sticky!

(Lili Grieco-St-Pierre, Jennifer Bruin/Created with BioRender.com)
Mild obesity-related (MOD) diabetes represents a nuanced aspect of Type 2 diabetes, often observed in individuals with higher body weight. Unlike more severe subtypes, MOD is characterized by a more measured response to insulin. The locks are “sticky,” so it is challenging for the key to click in place and open the lock. While MOD is connected to body weight, the comparatively less severe nature of MOD distinguishes it from other diabetes subtypes.
To minimize complications, treatment should include maintaining a healthy diet, managing body weight, and incorporating as much aerobic exercise as possible. This is where drugs like Ozempic can be prescribed to control the evolution of the disease, in part by managing body weight.
Mild age-related diabetes: I’m tired of controlling blood sugar!
(Lili Grieco-St-Pierre, Jennifer Bruin/Created with BioRender.com)
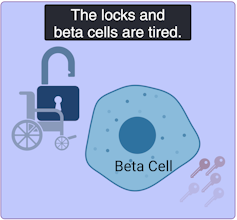
Mild age-related diabetes (MARD) happens more often in older people and typically starts later in life. With time, the key factory is not as productive, and the locks become stubborn. People with MARD find it tricky to manage their blood sugar, but it usually doesn’t lead to severe complications.
Among the different subtypes of diabetes, MARD is the most common.
Unique locks, varied keys
While efforts have been made to classify diabetes subtypes, new subtypes are still being identified, making proper clinical assessment and treatment plans challenging.
In Canada, unique cases of Type 2 diabetes were identified in Indigenous children from Northern Manitoba and Northwestern Ontario by Dr. Heather Dean and colleagues in the 1980s and 90s. Despite initial skepticism from the scientific community, which typically associated Type 2 diabetes with adults rather than children, clinical teams persisted in identifying this as a distinct subtype of Type 2 diabetes, called childhood-onset Type 2 diabetes.
Read more:
Indigenous community research partnerships can help address health inequities
Childhood-onset Type 2 diabetes is on the rise across Canada, but disproportionately affects Indigenous youth. It is undoubtedly linked to the intergenerational trauma associated with colonization in these communities. While many factors are likely involved, recent studies have discovered that exposure of a fetus to Type 2 diabetes during pregnancy increases the risk that the baby will develop diabetes later in life.
Acknowledging this distinct subtype of Type 2 diabetes in First Nations communities has led to the implementation of a community-based health action plan aimed at addressing the unique challenges faced by Indigenous Peoples. It is hoped that partnered research between communities and researchers will continue to help us understand childhood-onset Type 2 diabetes and how to effectively prevent and treat it.
A mosaic of conditions
(Lili Grieco-St-Pierre, Jennifer Bruin/Created with BioRender.com)
Type 2 diabetes is not uniform; it’s a mosaic of conditions, each with its own characteristics. Since diabetes presents so uniquely in every patient, even categorizing into subtypes does not guarantee how the disease will evolve. However, understanding these subtypes is a good starting point to help doctors create personalized plans for people living with the condition.
While Indigenous communities, lower-income households and individuals living with obesity already face a higher risk of developing Type 2 diabetes than the general population, tailored solutions may offer hope for better management. This emphasizes the urgent need for more precise assessments of diabetes subtypes to help customize therapeutic strategies and management strategies. This will improve care for all patients, including those from vulnerable and understudied populations.
-



 Sports23 hours ago
Sports23 hours agoAuston Matthews denied 70th goal as depleted Leafs lose last regular-season game – Toronto Sun
-
Media4 hours ago
DJT Stock Rises. Trump Media CEO Alleges Potential Market Manipulation. – Barron's
-
Business22 hours ago
BC short-term rental rules take effect May 1 – CityNews Vancouver
-
Media6 hours ago
Trump Media alerts Nasdaq to potential market manipulation from 'naked' short selling of DJT stock – CNBC
-
Art22 hours ago
Collection of First Nations art stolen from Gordon Head home – Times Colonist
-



 Investment22 hours ago
Investment22 hours agoBenjamin Bergen: Why would anyone invest in Canada now? – National Post
-



 Tech24 hours ago
Tech24 hours ago'Kingdom Come: Deliverance II' Revealed In Epic New Trailer And It Looks Incredible – Forbes
-
Media18 hours ago
DJT Stock Jumps. The Truth Social Owner Is Showing Stockholders How to Block Short Sellers. – Barron's



