Diabetes medications and blood-test supplies are sold, traded and donated on black markets because the U.S. health-care system isn’t meeting patients’ needs, a study shows. The price of insulin continues to increase, translating to $15 per day for the average user. Recent research indicates one in four people with diabetes ration their insulin because of the cost.
Health
U.S. diabetes patients turn to 'black market' for medications, supplies – Montreal Gazette

David Burns, 38, who has type 1 diabetes, prepares his insulin pen to inject himself in his home in North London on February 24, 2019. – Diabetics and insulin providers in Britain are stockpiling their precious medicine to avoid potential shortages in case Britain leaves the European Union without a deal in just over month’s time. Britain’s 3.7 million diabetics, which include Prime Minister Theresa May, depend almost entirely on insulin imports from continental Europe.
(Reuters Health) – Diabetes medications and blood-test supplies are sold, traded and donated on black markets because the U.S. healthcare system isn’t meeting patients’ needs, a study shows.
In a survey, about half of people who participated in these underground exchanges said they do it because they lack access to the proper medications and supplies to manage their diabetes, researchers report in the Journal of Diabetes Science and Technology.
“It is important for healthcare providers and policymakers to understand what people are doing to support diabetes management when faced with medication and supply access issues,” said study leader Michelle Litchman of the University of Utah College of Nursing in Salt Lake City.
The price of insulin continues to increase, translating to $15 per day for the average user, the study authors note. Recent research indicates that one in four people with diabetes ration their insulin due to cost, they add.
“While there are risks to using medications and supplies that are not prescribed to them, there are also risks to rationing or not taking medications or using supplies at all,” Litchman told Reuters Health by email.
In early 2019, the researchers surveyed 159 people who were involved in online diabetes communities, including patients and caregivers. They asked questions about underground exchange activities, access to healthcare and difficulty in purchasing diabetes items from standard sources.
More than half of the survey participants said they had donated medications or supplies, 35% received donations, 24% traded medications, 22% borrowed items and 15% purchased items. These exchanges took place among family, friends, co-workers, online acquaintances and strangers.
Overall, people who reported financial stress due to diabetes management were six times more likely to engage in underground exchanges and three times more likely to seek donations.
“The current healthcare situation in the United States is substandard for many people with chronic disease,” said Mary Rogers of the University of Michigan, in Ann Arbor, who wasn’t involved in the study.
“It is too costly. It is too slow. It is too complicated,” she said by email. “Failure to fix these problems leads to diabetic complications and unnecessary hospitalizations.”
Participants who donated medications felt compelled to give because they knew about the dire need of others, the study authors note. These respondents described a sense of duty and obligation to help. Others built up stockpiles that they donated, including insulin, pills, glucose strips, sensors and pump supplies.
Underground exchange could lead to several repercussions, including unanticipated side effects, complications of incorrect use, delay in seeking professional help and drug interactions, the authors caution. In addition, sharing and trading prescription medicines is illegal in the U.S. and other countries.
In this study, the researchers did not identify any adverse events, Litchman said.
Kebede Beyene of the University of Auckland, in New Zealand, who wasn’t involved in the study, told Reuters Health, “It seems that health professionals rarely ask patients about medicine sharing, trading or exchange, so it would make sense for health professionals to ask about medicines exchange during consultations and when dispensing medicines, particularly for high-risk medicines, such as diabetes medications, antibiotics and strong pain medications.”
“Patients can then be given information about the possible risks of taking someone else’s medicine or giving their prescribed medicines to another person,” Beyene said by email. “Community pharmacy practitioners are also in a unique position to educate about risks of medicine exchange.”
SOURCE: https://bit.ly/2MtPQa6 Journal of Diabetes Science and Technology, online December 4, 2019.
Health
Whooping cough is at a decade-high level in US

MILWAUKEE (AP) — Whooping cough is at its highest level in a decade for this time of year, U.S. health officials reported Thursday.
There have been 18,506 cases of whooping cough reported so far, the Centers for Disease Control and Prevention said. That’s the most at this point in the year since 2014, when cases topped 21,800.
The increase is not unexpected — whooping cough peaks every three to five years, health experts said. And the numbers indicate a return to levels before the coronavirus pandemic, when whooping cough and other contagious illnesses plummeted.
Still, the tally has some state health officials concerned, including those in Wisconsin, where there have been about 1,000 cases so far this year, compared to a total of 51 last year.
Nationwide, CDC has reported that kindergarten vaccination rates dipped last year and vaccine exemptions are at an all-time high. Thursday, it released state figures, showing that about 86% of kindergartners in Wisconsin got the whooping cough vaccine, compared to more than 92% nationally.
Whooping cough, also called pertussis, usually starts out like a cold, with a runny nose and other common symptoms, before turning into a prolonged cough. It is treated with antibiotics. Whooping cough used to be very common until a vaccine was introduced in the 1950s, which is now part of routine childhood vaccinations. It is in a shot along with tetanus and diphtheria vaccines. The combo shot is recommended for adults every 10 years.
“They used to call it the 100-day cough because it literally lasts for 100 days,” said Joyce Knestrick, a family nurse practitioner in Wheeling, West Virginia.
Whooping cough is usually seen mostly in infants and young children, who can develop serious complications. That’s why the vaccine is recommended during pregnancy, to pass along protection to the newborn, and for those who spend a lot of time with infants.
But public health workers say outbreaks this year are hitting older kids and teens. In Pennsylvania, most outbreaks have been in middle school, high school and college settings, an official said. Nearly all the cases in Douglas County, Nebraska, are schoolkids and teens, said Justin Frederick, deputy director of the health department.
That includes his own teenage daughter.
“It’s a horrible disease. She still wakes up — after being treated with her antibiotics — in a panic because she’s coughing so much she can’t breathe,” he said.
It’s important to get tested and treated with antibiotics early, said Dr. Kris Bryant, who specializes in pediatric infectious diseases at Norton Children’s in Louisville, Kentucky. People exposed to the bacteria can also take antibiotics to stop the spread.
“Pertussis is worth preventing,” Bryant said. “The good news is that we have safe and effective vaccines.”
___
AP data journalist Kasturi Pananjady contributed to this report.
___
The Associated Press Health and Science Department receives support from the Robert Wood Johnson Foundation. The AP is solely responsible for all content.
The Canadian Press. All rights reserved.
Health
Scientists show how sperm and egg come together like a key in a lock
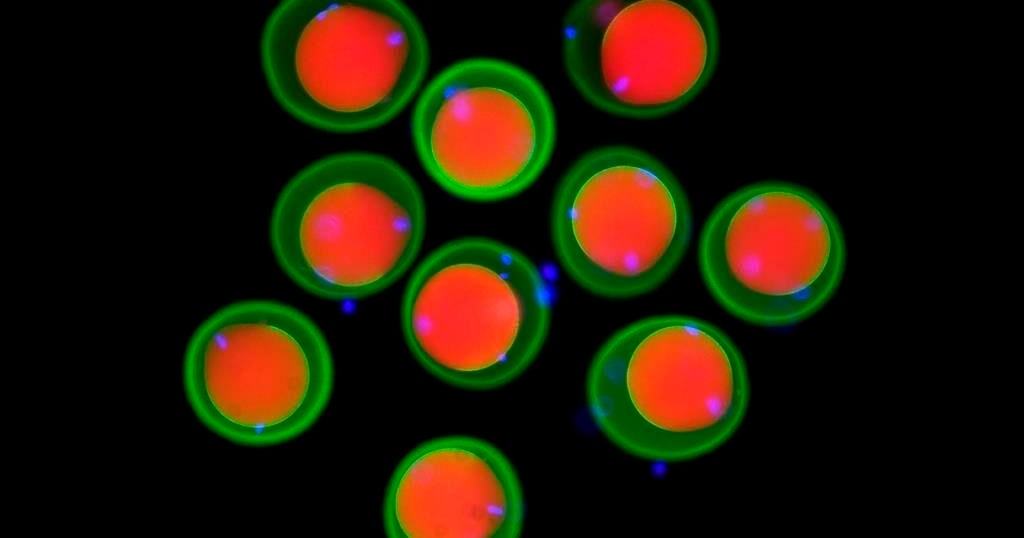
How a sperm and egg fuse together has long been a mystery.
New research by scientists in Austria provides tantalizing clues, showing fertilization works like a lock and key across the animal kingdom, from fish to people.
“We discovered this mechanism that’s really fundamental across all vertebrates as far as we can tell,” said co-author Andrea Pauli at the Research Institute of Molecular Pathology in Vienna.
The team found that three proteins on the sperm join to form a sort of key that unlocks the egg, allowing the sperm to attach. Their findings, drawn from studies in zebrafish, mice, and human cells, show how this process has persisted over millions of years of evolution. Results were published Thursday in the journal Cell.
Scientists had previously known about two proteins, one on the surface of the sperm and another on the egg’s membrane. Working with international collaborators, Pauli’s lab used Google DeepMind’s artificial intelligence tool AlphaFold — whose developers were awarded a Nobel Prize earlier this month — to help them identify a new protein that allows the first molecular connection between sperm and egg. They also demonstrated how it functions in living things.
It wasn’t previously known how the proteins “worked together as a team in order to allow sperm and egg to recognize each other,” Pauli said.
Scientists still don’t know how the sperm actually gets inside the egg after it attaches and hope to delve into that next.
Eventually, Pauli said, such work could help other scientists understand infertility better or develop new birth control methods.
The work provides targets for the development of male contraceptives in particular, said David Greenstein, a genetics and cell biology expert at the University of Minnesota who was not involved in the study.
The latest study “also underscores the importance of this year’s Nobel Prize in chemistry,” he said in an email.
___
The Associated Press Health and Science Department receives support from the Howard Hughes Medical Institute’s Science and Educational Media Group. The AP is solely responsible for all content.
The Canadian Press. All rights reserved.
Health
Turn Your Wife Into Your Personal Sex Kitten


Product Name: Turn Your Wife Into Your Personal Sex Kitten
All orders are protected by SSL encryption – the highest industry standard for online security from trusted vendors.

Turn Your Wife Into Your Personal Sex Kitten is backed with a 60 Day No Questions Asked Money Back Guarantee. If within the first 60 days of receipt you are not satisfied with Wake Up Lean™, you can request a refund by sending an email to the address given inside the product and we will immediately refund your entire purchase price, with no questions asked.
-

 News17 hours ago
News17 hours agoCanadanewsmedia news October 18, 2024: Testy B.C. election campaign reaches final day
-

 News17 hours ago
News17 hours agoUS to probe Tesla’s ‘Full Self-Driving’ system after pedestrian killed in low visibility conditions
-

 News17 hours ago
News17 hours agoAdvocates urge Ontario to change funding for breast prostheses, ostomy supplies
-

 News17 hours ago
News17 hours agoMore details expected on proposed deal that would see tobacco giants pay billions
-

 News17 hours ago
News17 hours ago‘Kindness’ influencers on TikTok give money to strangers. Why is that controversial?
-

 News17 hours ago
News17 hours agoHousing, health, and plastic straws: Here’s how B.C. politicians are wooing voters
-

 News17 hours ago
News17 hours agoTesty B.C. election campaign sees leaders attacking each other more than policy
-

 News17 hours ago
News17 hours agoRwanda shrugs off ‘sportswashing’ criticism in pursuit of a winning development formula